Responding to pandemic (H1N1) 2009 influenza in Aboriginal communities in NSW through collaboration between NSW Health and the Aboriginal community-controlled health sector
Sian Rudge A C and Peter D. Massey BA Centre for Aboriginal Health, NSW Department of Health
B Hunter New England Area Health Service
C Corresponding author. Email: sian.rudge@doh.health.nsw.gov.au
NSW Public Health Bulletin 21(2) 26-29 https://doi.org/10.1071/NB09040
Published: 8 April 2010
Abstract
As a vulnerable population, Aboriginal people in NSW were thought likely to be at more risk of serious illness from pandemic (H1N1) 2009 influenza than non-Aboriginal people. As such, the importance of consulting with Aboriginal people and communities was recognised early in the pandemic. This consultation was to enable key messages to be disseminated appropriately and to facilitate access to health care. Key stakeholders in the response were the NSW Department of Health, Area Health Services, the NSW Aboriginal Health and Medical Research Council, and Aboriginal Community Controlled Health Services. Regular teleconferences between the key stakeholders facilitated the flow of information and assisted with the identification of issues. A consultation process between Hunter New England Area Health Service and six Aboriginal communities helped inform the development of resources as well as the planning and delivery of pandemic-related services.
Aboriginal people were four times more likely to be admitted to hospital with pandemic (H1N1) 2009 influenza than non-Aboriginal people.
Pandemic (H1N1) 2009 influenza poses a risk to the health of Aboriginal people and communities in NSW. The disease is more infectious then seasonal influenza1 and can cause severe illness and death. Many of the health conditions associated with influenza complications are more common among Aboriginal people.2 Aboriginal communities have suffered more than other communities in past pandemics.3 Initial data for this pandemic from several countries showed increased rates of hospitalisation and deaths associated with H1N1 in Indigenous populations.4,5
As such, there was an awareness within NSW Health and the NSW Aboriginal Health and Medical Research Council (AH&MRC) at the beginning of the pandemic of the importance of ensuring that important messages were communicated appropriately and access to care facilitated. The engagement of Aboriginal people and services in the development and implementation of pandemic responses has been an essential part of the public health response.
This article describes: the epidemiology of the pandemic (H1N1) 2009 influenza among Aboriginal people in NSW; the collaboration between NSW Health and the Aboriginal community-controlled health sector to develop an appropriate response to protect Aboriginal people; the consultation process between the Hunter New England Area Health Service and local Aboriginal communities; and the application of an emergency management framework to manage a pandemic within Aboriginal communities.
Pandemic (H1N1) 2009 influenza in Aboriginal people in NSW
Methods
Information on people with pandemic (H1N1) 2009 influenza was collected by NSW Health public health units and collated through NetEpi, the web-based NSW Health surveillance and outbreak data collection system.6 With the national move to the PROTECT phase of the public health response, the focus of testing shifted to people who were hospitalised with influenza-like illness. Consequently reported numbers of confirmed cases describe only a proportion of the total number of people who were infected with pandemic influenza. The rate of hospitalisation associated with the pandemic however, provides a more accurate indication of the epidemiology and spread of pandemic (H1N1) 2009 influenza. The NSW public health network investigated Aboriginal status and risk factors on all admissions through inpatient data systems and direct contact with families and the person’s medical officer.
Results
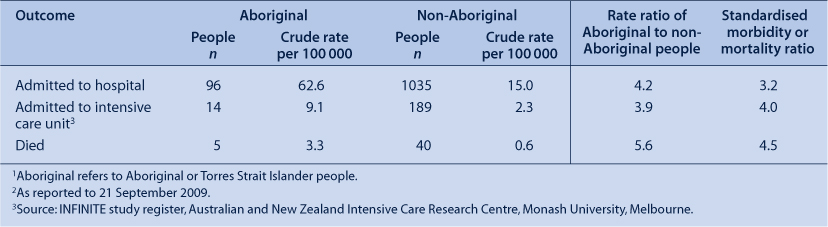
A total of 1214 people were hospitalised in NSW with pandemic (H1N1) 2009 influenza to 31 August 2009, including 225 people admitted to intensive care units (ICUs). Aboriginal status was reported for 93.2% (n = 1131) of people hospitalised; 90.2% (n = 203) of ICU admissions; and for 93.8% (n = 45) of pandemic influenza-related deaths. Of those admitted to hospital, 96 (7.8%) identified as Aboriginal and/or Torres Strait Islander. The rate ratios for admission to hospital, admission to ICUs and death were higher in the Aboriginal population compared with the non-Aboriginal population in NSW (Table 1).
|
Aboriginal people hospitalised with pandemic (H1N1) 2009 influenza were younger than non-Aboriginal people (median age of 24.5 years compared with 31.7 years). The ratio of males to females was similar for Aboriginal and non-Aboriginal people admitted to hospital.
While risk factor data were incomplete, 72 (75%) Aboriginal people hospitalised with pandemic (H1N1) 2009 influenza were reported to have known risk factors. Risk factors reported in the Aboriginal people admitted to hospital included: asthma; chronic obstructive pulmonary disease; chronic diseases of the heart, liver and kidneys; diabetes, neurological disease and smoking; pregnancy and recent delivery; and other morbidities. Twenty-four Aboriginal people admitted to hospital had no underlying risk factors reported. Risk factor data for non-Aboriginal people hospitalised in NSW have not yet been published.
Collaboration between NSW Health and the Aboriginal community-controlled health sector to control pandemic (H1N1) 2009 influenza
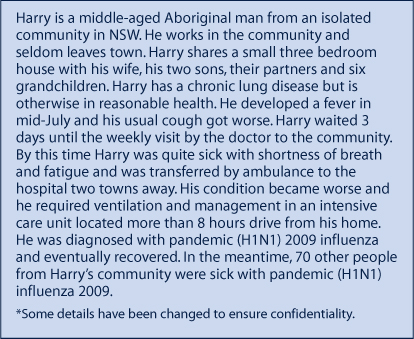
Some of the challenges of managing the influenza pandemic in Aboriginal communities are illustrated by the case study presented in Box 1.
|
The AH&MRC, Aboriginal Community Controlled Health Services (ACCHSs), and NSW Department of Health and area health services (AHSs) were key partners during the response to and recovery from the pandemic. While relationships existed between these partners before the pandemic, the urgency created by the response to the pandemic required a rapid development or strengthening of these relationships.
In NSW regular teleconferences between the partners were established early in the response to the pandemic. These were found to be valuable in supporting the partnership, determining the priority issues, identifying gaps in communication, and developing and making available common resources. Within the NSW Department of Health, the teleconferences were initiated and lead by the Chief Health Officer. A liaison officer role was established to: facilitate information flow between the key partners; identify and follow-up with issues related to anti-influenza medication orders; and assist with the preparation and dissemination of resources and messages for Aboriginal people and health services.
Prior to the pandemic public health units in NSW, which have a direct role in the public health management of disease outbreaks for the area health services, had differing levels of engagement with the Aboriginal community-controlled health sector. Here we focus on the response by the Hunter New England Area Health Service (HNEAHS), which has a long-standing relationship with the ACCHSs that are located within its geographical boundaries.
Consultation process between HNEAHS and Aboriginal communities
As a result of HNEAHS’s strong, existing partnership concerns associated with controlling pandemic (H1N1) 2009 influenza were able to be gathered through a rapid consultation process with six Aboriginal communities. The communities served by the ACCHSs in Newcastle, Inverell, Armidale, Taree, Tamworth and Forster were consulted. Input was gained from stakeholders and key informants in these communities were approached to participate in the influenza consultation.
The consultations consisted of focus group discussions which were included in community activities and group meetings. The groups were facilitated by at least one Aboriginal team member. During the focus group information was provided about the nature of influenza, its transmission, and the evolving pandemic. The community members were then encouraged to talk about potential issues and solutions.
The consultation identified issues which were subsequently grouped into five areas, with a number of potential solutions:
-
local identified ‘go to’ people need to have an understanding of pandemic influenza. ‘Go to’ people are local people who are trusted and easily accessed, and who the community already go to for advice. They may be health workers who can advise on what to do in the event of an infectious disease incident
-
information must be presented simply, clearly and demonstrate respect for local culture
-
sick people need to know where to go to get help and how to get there without infecting others
-
infection control messages should be aligned with the reality of life in Aboriginal communities, and recognise the importance of attending family and cultural gatherings
-
Aboriginal people need to have a say in how support is provided.8
This consultation helped inform resource development as well as the planning and delivery of pandemic-related services by the AHS. These findings were shared more widely with the pandemic response key stakeholder group, and resources were disseminated for use by other AHSs and ACCHSs.
Managing a pandemic through an emergency framework with Aboriginal communities
An emergency or disaster response framework offers the opportunity to address many of the issues associated with a rapidly emerging disease. Respectful collaboration with Aboriginal communities is vital in responding in an appropriate way to an emergency situation.
The principles that underpin the National Emergency Strategy for Remote Indigenous Communities, Keeping our mob safe7 are built around respectful collaboration. The principles include:
-
communication relating to emergency management is based on culturally friendly language and the use of different and appropriate communication media for remote Indigenous communities
-
community emergency management plans are developed in consultation and partnership with remote Indigenous communities and local governance structures
-
community emergency management in remote Indigenous communities is included as part of the mainstream service provision work plans of all agencies
-
flexible models of service delivery are used to meet the emergency management needs of remote Indigenous communities.
Although a large part of NSW is classified as being remote, most of the NSW Aboriginal Australian population live in rural, regional and urban NSW. However, many Aboriginal communities in NSW have community structures and community-based services that enable the principles used in remote areas to be applied.
Further strengthening of collaboration
The response to the pandemic highlighted the strengths of the existing partnerships between the Aboriginal community-controlled health sector and NSW Health. The response also identified, at a state and AHS level, where support for both day to day management of public health issues and public health emergencies could be improved.
The issues identified by the communities in the rapid consultation process with HNEAHS are now forming the basis of a large national project to reduce the future risk of pandemic influenza to Aboriginal communities. Funded by the National Health and Medical Research Council, the project is using a participatory action research methodology to hear from communities and build understanding. The aims of the project are to: identify barriers to mainstream management strategies and treatment plans in communities; develop culturally appropriate and effective management strategies and treatment plans by consulting with communities; and share what is found with other Indigenous communities across Australia.
Conclusion
Aboriginal people were admitted to hospital with pandemic (H1N1) 2009 influenza at rates more than four times higher than non-Aboriginal people. This highlights the importance of providing a co-ordinated and respectful response with partners for this vulnerable population. The rapidly emerging disease required an emergency strategy that was developed in collaboration with Aboriginal communities.
As a result of the influenza pandemic, engagement between the NSW Department of Health, AHSs, ACCHSs and Aboriginal communities has been strengthened. The strength of this engagement will continue to grow if the NSW public health network can prioritise this work and invest in the challenges posed by future public health emergencies to ensure that public health responses are effective and sustainable.
Acknowledgments
We acknowledge the AH&MRC, the NSW public health network, and the Area Health Services Managers for Aboriginal Health for their work in this field. We also acknowledge the work of the Australian and New Zealand Intensive Care Research Centre of Monash University, Melbourne for the development of the intensive care influenza A (INFINITE study) register and co-ordination of the intensive care data collection.
[1] Fraser C, Donnelly CA, Cauchemez S, Hanage WP, Van Kerkhove MD, Hollingsworth TD, et al. Pandemic potential of a strain of influenza A (H1N1): early findings. Science 2009; 324(5934): 1557–61.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS | (Cited 9 October 2009.)
[3] Curson P, McCracken K. An Australian perspective of the 1918–1919 influenza pandemic. N S W Public Health Bull 2006; 17 103–7.
| Crossref | GoogleScholarGoogle Scholar | PubMed | (Cited 03/09/2009.)

