A polio intervention in East African refugees to NSW
Mitchell M. Smith A C and Sanjyot Vagholkar BA NSW Refugee Health Service
B General Practice Unit, Fairfield Hospital and School of Public Health and Community Medicine, University of NSW
C Corresponding author. Email: mitchell.smith@sswahs.nsw.gov.au
NSW Public Health Bulletin 20(6) 77-80 https://doi.org/10.1071/NB07125
Published: 24 June 2009
Abstract
This paper summarises a public health intervention in Sydney, NSW in late 2006 that resulted from the potential exposure of a number of refugees to polio virus while in transit in Nairobi, Kenya. The intervention involved the attempted follow-up of 113 persons at risk, assessment for symptoms and immunisation where indicated. No symptomatic cases were found. Seventy-five people were immunised with inactivated poliomyelitis vaccine. The intervention highlighted the importance of close collaboration between health services, the Department of Immigration and Citizenship and settlement service agencies, and provided several lessons to consider when assessing newly arrived refugees.
New South Wales (NSW) receives between 3000 and 4000 permanent refugee settlers each year.1 In the past 5 years, nearly 43% of these have come from African countries, in particular the Sudan but also Sierra Leone, Liberia, Burundi and others.1
In October 2006, the then Department of Immigration and Multicultural Affairs (DIMA), now known as the Department of Immigration and Citizenship, was notified of a confirmed case of polio in a girl in Dadaab refugee camp in northern Kenya.2 A small number of refugees from the Dadaab camp had come to Australia in the period of concern. Additionally, a number of refugees from other camps (mainly in Kenya and Tanzania) had passed through the International Organization for Migration (IOM) Transit Centre in Kilmani, Nairobi, and had potentially been in contact with refugees from the Dadaab region.
A subcommittee of the Communicable Diseases Network of Australia (CDNA) met and, in consultation with DIMA, recommended that refugees who may have come into contact with polio be assessed for signs and symptoms of the disease and be vaccinated if appropriate. A similar intervention was underway in the United States.3
In the latter part of 2006, NSW had not received any refugee settlers from Dadaab camp, but received 113 people who had transited through Nairobi in the period in question. It was recognised that not everyone who passed through Nairobi en route to Australia had actually been in the transit camp, so not all were deemed at risk.
Planning
Advice concerning the intervention was received from CDNA. Refugees who had passed through the transit centre in Nairobi before arrival in Australia would:
-
be contacted and given information in their language about the current situation and be asked to attend a clinic for review;
-
be clinically assessed for signs or symptoms of polio and, if indicated, have a stool specimen collected for polio testing;
-
have polio vaccination(s) as per age; and
-
be given hand washing advice (including a fact sheet from CDNA).
People living in the same household (other than refugee family members) were to be assessed and treated in a similar manner.
DIMA provided advice about the settlement locations of those refugees requiring follow-up. The refugees were dispersed across three area health services as follows:
-
Sydney West Area Health Service, 70 refugees;
-
Sydney South West Area Health Service, 20 refugees; and
-
Wollongong region, South Eastern Sydney Illawarra Area Health Service, 23 refugees.
Ten family units (ranging in size from one to nine people) had arrived under refugee visas (subclass 200) and were therefore in direct contact with the DIMA-funded settlement service, the Australian Centre for Languages (ACL).4,5 Eighteen family units had arrived on Special Humanitarian Program visas, having been sponsored: their initial settlement needs were met by family members or other sponsors.4 Arrivals in the latter category are historically more difficult to contact and engage.
A teleconference was held on 31 October 2006 between the NSW Department of Health, relevant public health unit directors and the NSW Refugee Health Service with the following outcomes:
-
a protocol was drafted outlining roles and responsibilities for public health units, the Refugee Health Service and ACL;
-
the Refugee Health Service was tasked with co-ordinating the intervention;
-
the Refugee Health Service and each of the three relevant public health units were to consider the most suitable arrangements for local service provision and data collection; and
-
no proactive media involvement was planned, for fear of stigmatisation.
The State Vaccine Centre was contacted and it advised that 170 doses of inactivated poliomyelitis vaccine (IPV) were in stock.
Intervention
A mix of arrangements for service provision was made depending on numbers to be seen and the existing services in each area health service:
Sydney West Area Health Service
-
Clinics (staffed by the public health unit and Refugee Health Service) held at community health centres;
-
Existing outpatient clinic for refugee children at the Children’s Hospital, Westmead;
-
Routine Refugee Health Service clinics; and
-
Home visits by public health unit staff.
Sydney South West Area Health Service
-
General Practice Unit, Fairfield Hospital, assisted by public health unit staff;
-
General practitioners; and
-
Routine Refugee Health Service clinic.
South Eastern Sydney Illawarra Area Health Service
-
General practitioners.
Close liaison was required with ACL to identify current addresses of the refugee settlers, inform them of the need to be assessed and assist with transporting people to the various locations. Immunisation status was assessed through documentation (rarely present) or history.
Outcomes
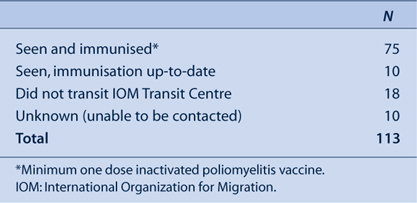
DIMA flagged 113 refugees as having come to NSW via Nairobi in the period of interest. Of these, 103 could be contacted. Eighty-five people were confirmed as having passed through the Nairobi IOM Transit Centre between early September and mid October 2006, and were therefore at potential risk of exposure to polio. Characteristics of these 85 people are listed in Table 1 and the numbers of refugees assessed and immunised are shown in Table 2.

|
|
None of the refugees who had transited in the Nairobi transit centre had relevant symptoms. Therefore, following the protocol for the intervention, no stool samples were collected. Seventy-five recent arrivals were immunised and 19 household contacts were also assessed and vaccinated.
While the majority of people were seen within 2 weeks of the start of the intervention (i.e. by mid November 2006), difficulties in contacting some refugees and failure of others to attend meant that some individuals were not seen until December. A small number were not contacted (Table 2) despite multiple attempts by ACL staff to locate them by telephone and through community contacts. The 10 people who were not assessed were four young males and one family of six; all were Sudanese entrants on sponsored Special Humanitarian Program visas. People on this visa generally have less engagement with formal settlement services after arrival.
Other logistic challenges included:
-
some new arrivals frequently moving house;
-
large families (up to nine people);
-
the short timeframe for implementation of the intervention prevented translation of the fact sheets, so information about polio and personal hygiene was given verbally through interpreters or settlement workers who spoke the appropriate language;
-
insufficient availability of suitably qualified interpreters;
-
transport needs, including the need for staff or volunteers to accompany the refugees to clinics;
-
limited capacity of ACL staff to assist due to an ongoing need to assist other new arrivals during the period;
-
IPV not being held by general practitioners, requiring transport of the vaccine to general practice clinics; and
-
difficulties ascertaining past history of vaccination among the refugees, including a lack of documentation.
The episode did not attract any media attention. This was seen as a positive outcome for the refugee settlers, given that in the past there has been unwarranted concern about refugee settlers and imported infectious diseases.6
Discussion
This was the first time, to our knowledge, that a targeted follow-up of refugee entrants had occurred in NSW in response to a specific disease concern. Despite the logistic challenges outlined, the majority of those needing to be assessed were seen and immunised where appropriate.
The willingness of general practitioners and various hospital, community health and public health unit staff to be involved was vital during this intervention. The NSW Refugee Health Service acted as a central co-ordination point and this was seen as useful, particularly because the Service had existing links with local DIMA staff, settlement service providers, public health units, the General Practice Unit at Fairfield Hospital and other relevant service providers.
A number of lessons were learnt from this public health intervention. In a similar situation in the future, we would recommend:
-
direct contact between health service staff and patients in preference to contact via settlement service (e.g. ACL) staff, to help ensure that health information being communicated is appropriate, and to facilitate logistic arrangements;
-
that specific additional resources be made available to settlement services for such an intervention, as these services play an important liaison role;
-
access to an adequate number of volunteers with suitable transport to get newly arrived refugees to health services efficiently;
-
timely efforts at the national level to enhance interpreter availability for certain minority languages;
-
increased information for mainstream health staff in this setting to help sensitise them to working with traumatised, newly arrived refugee families;
-
more communication in the early stages involving all relevant agencies, which would help to identify logistic barriers and to share potential solutions; and
-
that a detailed protocol covering roles and responsibilities for health and non-health agencies be prepared to assist implementation of the intervention.
The intervention highlighted the fact that even with resource-intensive pursuit of individuals and families, not all newly arrived refugees can necessarily be tracked down. This has implications for other disease outbreaks requiring rigorous follow-up, and for routine screening of certain conditions among new arrivals to NSW.
Conclusion
This intervention relating to poliomyelitis assessment and immunisation was ultimately successful, yet it presented a number of logistical and other challenges for those involved. It is likely that there will be further interventions of this type in the future, requiring interaction between clinical and public health staff and agencies involved with newly arrived refugees. Lessons from this event may inform the response to similar episodes.
Acknowledgments
The authors would like to thank medical, nursing and administrative staff from all health services that contributed to this intervention. The support and liaison provided by Dr Kathy King and other staff from the Department of Immigration and Citizenship is appreciated. The vital assistance from ACL settlement service staff is also warmly acknowledged.
[1]
[2]
[3]
[4]
[5]
[6]

