Communicable Diseases Report, NSW, September and October 2008
NSW Department of Health
NSW Public Health Bulletin 19(12) 218-222 https://doi.org/10.1071/NB08060
Published: 7 January 2009
Abstract
For updated information, including data and facts on specific diseases, visit http://www.health.nsw.gov.au and click on Infectious Diseases or access the site directly at: http://www.health.nsw.gov.au/publichealth/infectious/index.asp.
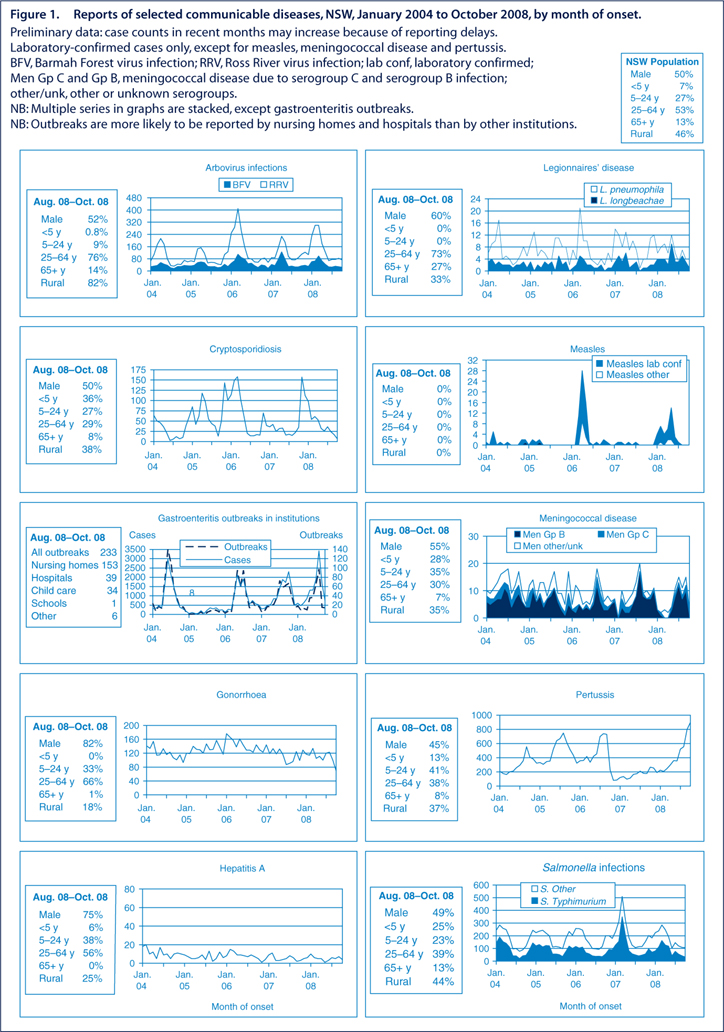
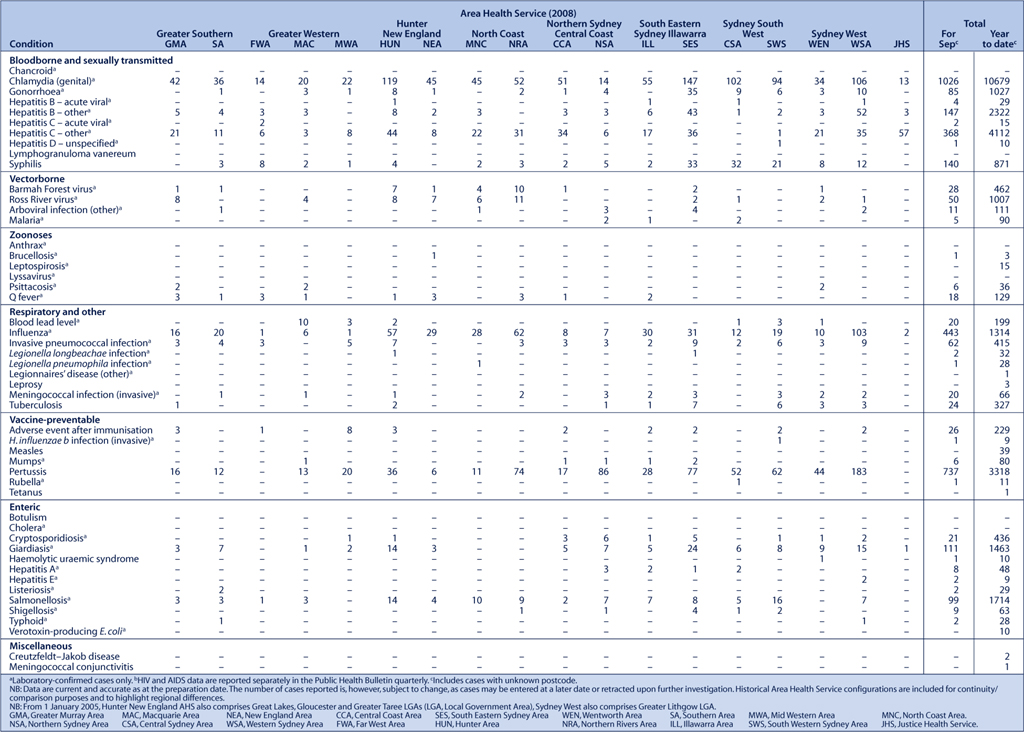
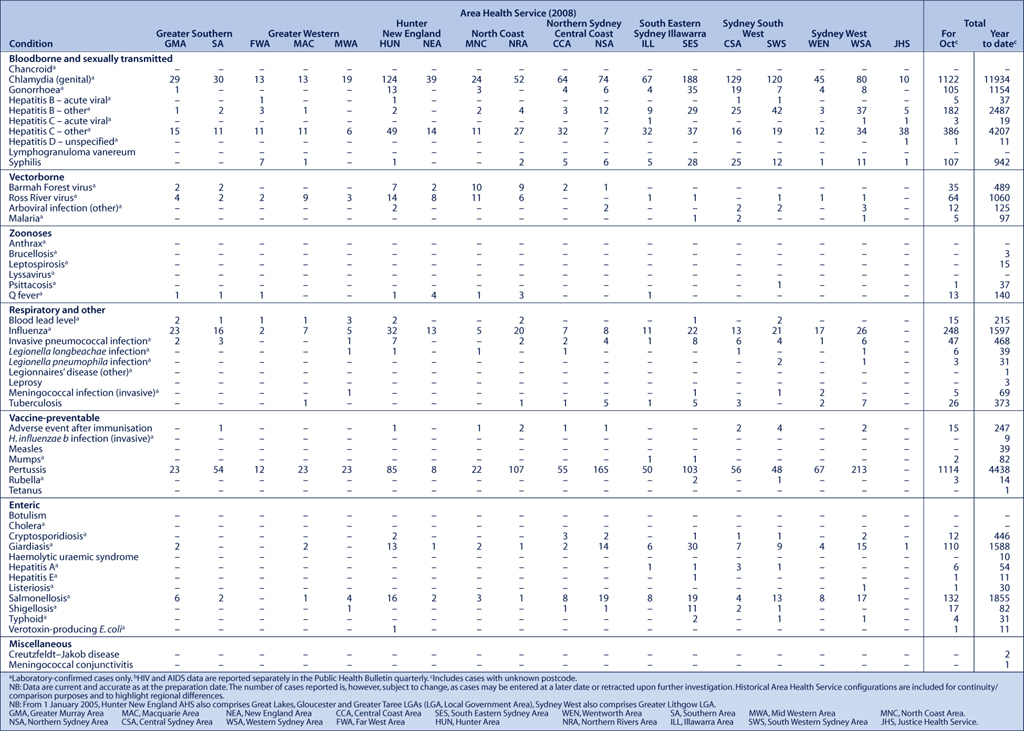
Figure 1 and Tables 1 and 2 show reports of communicable diseases received through to the end of October 2008 in New South Wales (NSW).
|
|
Mumps
Six cases of mumps were notified in September and a further two cases were notified in October, bringing the total number of cases to 82 in NSW this year. This is a significant reduction from 2007, where more than 300 cases were notified. However, as infection often occurs with minimal symptoms, the true number of cases is likely to be higher than reported in all years.
Mumps is a vaccine-preventable disease spread by droplet infection and direct contact with the saliva of people with the infection. Maximum infectiousness occurs from 2 days before to 4 days after onset of illness.
Symptoms include fever, loss of appetite, tiredness and headaches followed by swelling and tenderness of the salivary glands. One or both of the parotid salivary glands (in front of and below the ears) are often affected.
Mumps is usually a more severe illness in people infected after puberty. Complications are uncommon but can include encephalitis, meningitis, hearing loss, orchitis in post-pubertal boys and men, and ovarian inflammation in women.
To help prevent the spread, exclusion of people with mumps from work, school, child care and other settings is currently recommended for up to 9 days from the onset of swelling or until fully recovered, whichever is sooner. Immunisation against mumps takes place with the measles, mumps, rubella (MMR) vaccine, which is given routinely at 12 months and 4 years of age.
Hepatitis D
One case of hepatitis D was notified in September, and a further case was notified in October, bringing the total number of cases to 11 in NSW this year. This is close to the average for recent years.
Hepatitis D is a rare infection that occurs only in people who already have hepatitis B virus (HBV) infection. Its importance lies particularly in the fact that co-infection with both viruses means greater risk of severe liver disease, including severe acute hepatitis, which can progress to chronic disease.
The modes of transmission for hepatitis D are similar to that for hepatitis B: exposure to infected blood and serous body fluids, contaminated needles, syringes or blood- and plasma-product transfusions. Sexual transmission may also occur but is less common than with HBV infection. Perinatal infection is rare. Infection may occur at the same time as a new HBV infection (co-infection) or when a person already infected with HBV develops chronic infection (super-infection).1
There is no vaccine for hepatitis D, however, vaccination against hepatitis B prevents hepatitis D virus infection.
Shigella
An increase was detected in the number of shigellosis cases notified in NSW in September and October. Twelve men, mostly residents of inner Sydney, were notified with Shigella sonnei biotype g infection. A similar increase in Sh. sonnei biotype g was also recently detected in Victoria. These cases shared an unusual antibiotic-resistance pattern, which suggested that all of the cases were epidemiologically related.
Nine of the NSW cases were interviewed using a semi-structured, hypothesis-generating questionnaire. Interviewed cases reported illness lasting typically 6 to 7 days. Three cases required intravenous rehydration and antibiotics were prescribed for seven cases. No cases reported travel either overseas or outside of NSW in the 7 days prior to onset. There were no common food exposures. One case reported contact with another ill person. None of the cases identified recent contact with someone with shigellosis.
All interviewed cases were men who have sex with men. Seven cases reported having sex in the 3 days prior to onset with one to five partners. Two cases attended sex on premises venues. Three cases attended private sex parties and two reported sexual activity at home. Six cases reported oral and anal sex, and four cases reported oro-anal sex.
All isolates were resistant to antibiotic treatment with streptomycin, sulphonamide, tetracycline, trimethoprim and naladixic acid, and had a reduced susceptibility to ciprofloxacin. This was the same resistance pattern as the Victorian isolates.
Alerts were published in Sydney’s gay newspapers, advising people to avoid infection and seek treatment if they become sick. Alerts were faxed to general practitioners in metropolitan Sydney with advice to request stool specimens and test for shigellosis in men who have sex with men who present with diarrhoea.
No epidemiological links were identified between cases. Knowledge of shigellosis, and the transmission of Shigella, was poor and few men identified that some sexual practices could be a risk factor for infection. Further work is recommended with this community to raise awareness of bacterial pathogens and prevention strategies.
All shigellosis infections should be treated for public health reasons as only a small inoculum is required for the infection to be transmitted to another person. Current Australian therapeutic guidelines recommend first-line treatment with norfloxacin, trimethoprim or ampicillin. As ampicillin is no longer available as an oral preparation in Australia, amoxycillin was identified as a suitable alternative for the purposes of treating cases related to this outbreak.
Shigellosis can be prevented by maintaining good general hygiene, including washing hands thoroughly after going to the toilet, after having sex and before eating. People with new onset diarrhoea should avoid having sex while they are unwell and should not prepare food for others.
[1]