The NSW Immunisation Strategy 2008–2011: how are we doing?
Peter B. McIntyre A B E F , David N. Durrheim C and Sue Campbell‐Lloyd D FA National Centre for Immunisation Research and Surveillance,The Children’s Hospital at Westmead
B Sydney Medical School, The University of Sydney
C Hunter New England Area Health Service
D AIDS and Infectious Diseases Branch,NSW Department of Health
E Corresponding author. Email: PeterM@chw.edu.au
F Guest editor of this issue
NSW Public Health Bulletin 21(10) 193-195 https://doi.org/10.1071/NB10069
Published: 18 November 2010
Australian and international experience demonstrates that ongoing monitoring of the delivery of immunisation programs against clear objectives is necessary to maintain the momentum and optimal performance of these programs. With New South Wales (NSW) well into the term of its second Immunisation Strategy, and with the process of re‐developing the National Immunisation Strategy underway, it is timely to take stock.
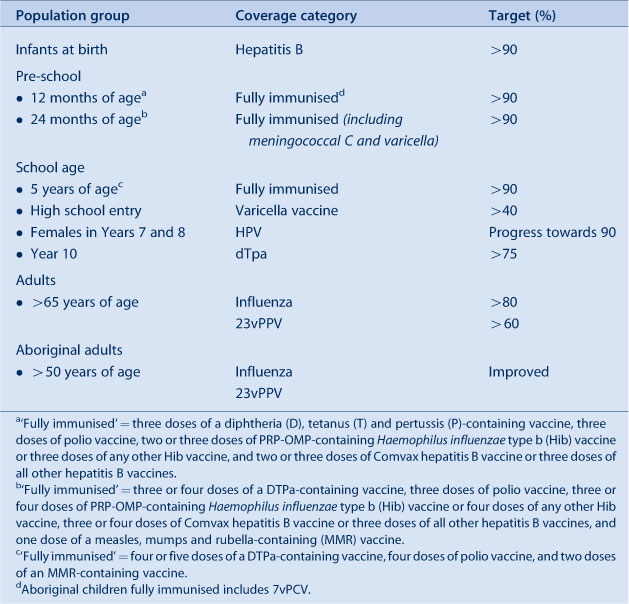
A review of the first NSW Immunisation Strategy (2003–2006) in 2007 found that the NSW Immunisation Program had met its objectives for immunisation coverage (higher than 90% coverage for both Aboriginal and other children at 24 months of age) and had developed the infrastructure to successfully deliver school‐based programs (as demonstrated by programs for meningococcal C conjugate and diphtheria‐tetanus‐pertussis vaccines).1 The focus of the second strategy (2008–2011) includes: timeliness of immunisation (particularly for children aged 4 years); further progress on immunisation coverage for Aboriginal people of all ages; and further development of school‐based programs. It nominates a number of key result areas including achieving coverage targets for specific age groups (Table 1) and priority population subgroups (Aboriginal people, health care workers, under‐immunised children), as well as program enhancements (communication, provider support, vaccine supply, surveillance and reporting).
|
This issue of the NSW Public Health Bulletin serves as a mid‐term report card for the NSW Immunisation Strategy 2008–2011. The intelligence provided will facilitate the contribution of NSW to the development of the new National Immunisation Strategy. To assist readers, at the end of this editorial is a glossary of the abbreviations of the vaccines referred to in this issue (Box 1).
Vaccine‐preventable diseases in NSW
As reported in this issue by Spokes and Gilmour, vaccine‐preventable disease control in NSW is good and in line with Australian national averages. Invasive disease due to Haemophilus influenzae type b, Neisseria meningitidis type C and Streptococcus pneumoniae serotypes included in the 7‐valent pneumococcal conjugate vaccine was rare in 2009.

|
There are two main gaps in vaccine‐preventable disease control: pertussis at all ages; and measles and mumps among adults aged 25–29 years. Epidemic pertussis in 2008 and 2009 and more extensive use of polymerase chain reaction as a diagnostic test in community laboratories combined to greatly increase pertussis reporting.2 However, in contrast to the largest previous epidemic in 1995–1997 when there were six deaths recorded in NSW,3 one death was recorded in 2008–2009. This suggests that the much higher levels of population coverage achieved over the past decade have had a favourable impact on the most severe manifestations of pertussis. Over the next 12 months it will be important to evaluate the impact of the NSW initiative (from the first half of 2009) to encourage earlier receipt of the first dose of pertussis‐containing vaccine at 6 weeks of age and to offer adult‐formulated pertussis vaccine to new parents and other close contacts of infants.
With respect to measles and mumps among 25–29 year‐olds, this age cohort is the most prominent in notifications. These adults have relatively low coverage of the two‐dose measles‐mumps‐rubella (MMR) vaccine as they were too old to be included in the 1998 measles school‐based campaign.4 This age group is also one of the most travelled and contact overseas with measles and mumps heightens their risk of disease. Making MMR vaccine available free of charge to young adults who are planning to travel is an important initiative which should continue, as should promoting public awareness of measles as a travel‐acquired infection.
Immunisation coverage
As reported in this issue by Hull et al., at state level NSW is equal to or better than other Australian jurisdictions for all parameters of childhood immunisation coverage. At an area health service level there are some important pockets of low coverage. This is especially relevant to the potential impact of the introduction of measles, as was recently seen in another low coverage area in Australia, the Sunshine Coast in south‐east Queensland.5 Overall coverage at 2 years of age is lowest in the North Coast Area Health Service, but with substantial variability within that region and notable differences in coverage for individual vaccines. Much of this difference is attributable to conscientious objection, with the North Coast having almost four times the state average (4.9% versus 1.3%). If children with no vaccines recorded are broadly considered to be conscientious objectors (but unregistered as such), then the remaining proportion (when the proportions fully immunised and with no vaccines recorded are subtracted) approximates incompletely immunised children – this latter group is where further initiatives to improve access to and awareness of immunisation are most likely to be beneficial. The incompletely immunised proportion is below 4% in two area health services (Greater Western and Hunter New England) but above 5% in all others, with the highest proportion being in the Northern Sydney Central Coast Area Health Service (5.7%).
The most readily identifiable group of partially immunised and therefore late immunised children is Aboriginal children. At state level, coverage of Aboriginal children is almost equal to other children by 24 months of age but lags by 7% at 12 months of age, with an 11.3% gap in the Sydney South West Area Health Service. It is notable that in the North Coast Area Health Service coverage for Aboriginal children at 12 months of age is higher than for non‐Aboriginal children and remains so at 24 months of age.
Adverse events following immunisation
Recent Australian experience demonstrates the importance and the limitations of routine passive post‐marketing surveillance of adverse events following immunisation in detecting a signal of excess fever and febrile convulsions in young children who had received one of the 2010 seasonal influenza vaccines (post-marketing – the vaccine has been approved by regulatory authorities for marketing). As emphasised in this issue by Mahajan et al., there is also value in providing reassurance to immunisers, parents and vaccine recipients that there is ongoing scrutiny for adverse events following immunisation and that data are made available to the public and immunisation providers on a regular basis. A stable system of adverse events reporting in NSW for over a decade and a solid denominator through the Australian Childhood Immunisation Register allows credible interpretation of trends. Given the importance of optimal management of adverse events following immunisation, evaluation of novel systems for active adverse event detection are certainly worth exploring.6 As illustrated in this issue by Wood, the assessment of suspected adverse events is often complex, so the expansion of clinical and advisory services underway in NSW to create a statewide network of relevant medical sub‐specialists to assist in the assessment of adverse events following immunisation is a very welcome initiative.
School‐based vaccination in NSW
As documented in this issue by Ward et al., the re‐introduction of NSW school‐based vaccination services in 2003 to implement the National Meningococcal C Vaccination Program, leading to the inclusion of all the vaccines recommended by the National Health and Medical Research Council for adolescents, has been a major development and is now well established. Good coverage for students who had not previously received a course of hepatitis B vaccine has been achieved when compared to the administration of vaccines for this age group by general practitioners.7 The program facilitates the rapid introduction of new vaccines and the schedule changes for existing vaccines to address low coverage of particular age cohorts. An example is the recent change from 15 years of age to 12 years of age for the adult‐formulated diphtheria‐tetanus‐pertussis vaccine (dTpa). The extensive range of catch‐up vaccines offered in Intensive English Centres is an important public health initiative to protect these vulnerable students.
Health care worker vaccination
As discussed in this issue by Leask et al., NSW Health introduced a health care worker vaccination policy in 2007 to assist employers to meet their occupational health and safety obligations and their duty of care to staff, clients, students on placement and other users of health services. This international leading policy is unique in that it includes a wide range of vaccines (dTpa, MMR, varicella and hepatitis B) rather than focusing solely on influenza vaccine. Implementation of the policy by universities and area health services has progressed gradually and is now embedded in recruitment strategies.
Conclusion
Progress against the NSW Immunisation Strategy 2008–2011 is encouraging but efforts to maintain and enhance these gains are needed to ensure that NSW residents continue to enjoy the benefits afforded by effective vaccination. The important contributions of vaccinators in general practice, Aboriginal medical services and area health services should be applauded.
[1]
[2] Spokes PJ, Quinn HE, McAnulty JM. Review of the 2008–2009 pertussis epidemic in NSW: notifications and hospitalisations. N S W Public Health Bull 2010; 21(7–8): 167–73.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[3] Brotherton J, McAnulty JM. A pertussis epidemic in NSW: how epidemiology reflects vaccination policy. N S W Public Health Bull 2003; 14(3): 77–81.
| PubMed |

[4] Aratchige PE, McIntyre PB, Quinn HE, Gilbert GL. Recent increases in mumps incidence in Australia: the “forgotten” age group in the 1998 Australian Measles Control Campaign. Med J Aust 2008; 189(8): 434–7.
| PubMed |

[5] Martin N, Foxwell AR. Measles status in Australia, andoutbreaks in the first quarter of 2009. Commun Dis Intell 2009; 33(2): 225–31.
| PubMed |

[6] Davis RL, Kolczak M, Lewis E, Nordin J, Goodman M, Shay DK, et al. Active surveillance of vaccine safety: a system to detect early signs of adverse events. Epidemiology 2005; 16(3): 336–41.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[7] Correll PK, Hayen A, Eyeson‐Annan M. Hepatitis B immunisation in children aged 10–13 years in New South Wales, 2001. N S W Public Health Bull 2003; 14(1–2): 17–20.
| Crossref | GoogleScholarGoogle Scholar | PubMed |


