Communicable Diseases Report, NSW, July and August 2010
Communicable Diseases BranchNSW Department of Health
NSW Public Health Bulletin 21(10) 250-255 https://doi.org/10.1071/NB10070
Published: 18 November 2010
Abstract
For updated information, including data and facts on specific diseases, visit www.health.nsw.gov.au and click on Public Health and then Infectious Diseases. The communicable diseases site is available at: http://www.health.nsw.gov.au/publichealth/infectious/index.asp.
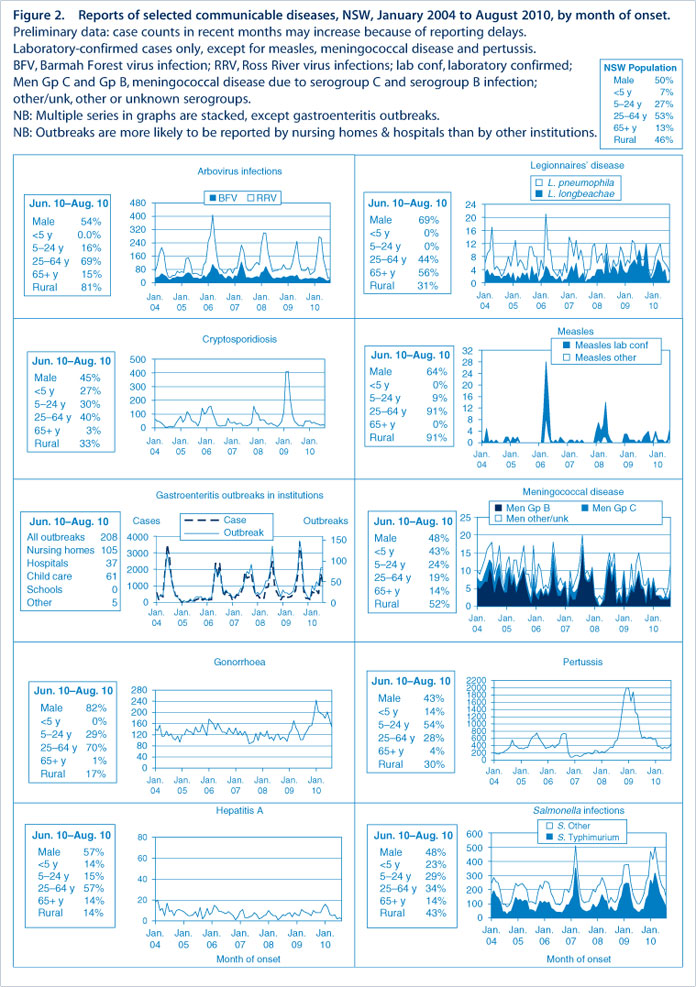
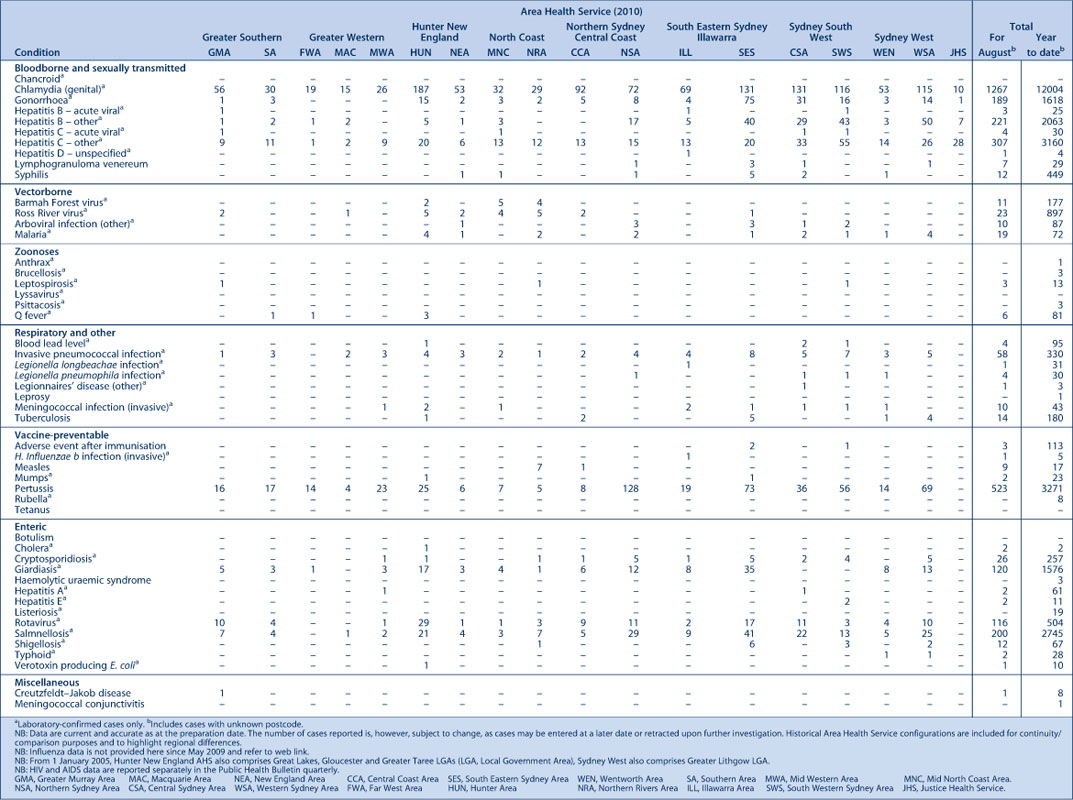
Figure 2 and Tables 1 and 2 show reports of communicable diseases received through to the end of July and August 2010 in New South Wales (NSW).

|
|
Enteric infections
Outbreaks of foodborne disease
Ten outbreaks of suspected foodborne disease were investigated in July and August 2010. In three of these outbreaks (one of which occurred in an aged-care facility) stool specimens tested positive for Salmonella Typhimurium. In one, samples of the fried ice-cream that the affected people had consumed in a restaurant also tested positive for S. Typhimurium. In the other two, environmental samples and food samples tested negative for any pathogens. In the remaining seven outbreaks none of the cases submitted a stool specimen for testing so the causative pathogen could not be identified. Several of these outbreak investigations are ongoing.
Outbreaks of gastroenteritis in institutional settings
One hundred and sixty-seven outbreaks of gastroenteritis in institutions were reported in July and August 2010, affecting 2795 people. Eighty-six outbreaks occurred in aged-care facilities, 45 in child-care centres, 33 in hospitals, one in a military institution and two in other institutions (a physical disability facility and a mental health facility). All outbreaks appeared to have been caused by person-to-person spread of a viral illness. In 60 outbreaks (36%) stool specimens tested positive for norovirus, and in 5 outbreaks (3%) stool specimens tested positive for rotavirus. Test results for several outbreaks may still be pending.
Viral gastroenteritis tends to peak in winter months, when around 15 outbreaks per week are reported.
Gastroenteritis in the community
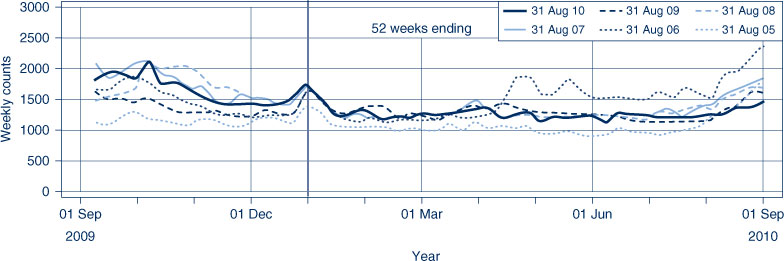
The number of patients presenting with gastrointestinal illness to 56 of the largest emergency departments in NSW increased slightly but remained within the usual range for the time of year (Figure 1).
Respiratory and other infections
Legionnaires’ disease
Nine cases of Legionnaires’ disease were reported in NSW in July and August 2010, including two cases due to Legionella longbeachae and seven cases due to L. pneumophila. For the same period in 2009, 15 cases of L. longbeachae and two of L. pneumophila infection were reported.
Two of the individuals with L. pneumophila reported spending time in the Sydney Olympic Park area during the incubation periods for their illness. Following an environmental investigation of the Sydney Olympic Park area on 28 August, water specimens collected from a cooling tower system in one of the stadiums tested positive for L. pneumophila. The contaminated cooling tower system was closed down until it could be cleaned and disinfected. While this cooling tower system could not be definitively linked to the two cases, NSW Health alerted general practitioners and respiratory doctors by fax, encouraging them to consider the the issue when diagnosing people who had visited the Sydney Olympic Park area during August. The public were also alerted via the media.
Influenza
In July and August 2010, influenza activity in NSW (as measured by the number of people who presented to 56 of the state’s largest emergency departments with influenza-like illness and the number of patients who tested positive for influenza at diagnostic laboratories) was low.
-
There were 220 presentations (1.3 per 1000 presentations) for July and 236 presentations (1.7 per 1000 presentations) for August to 56 of the largest emergency departments in NSW of people with influenza-like illness.
-
There were 33 cases of laboratory-confirmed influenza (including 19 of pandemic (H1N1) 2009) reported in July and 110 (including 83 of pandemic (H1N1) 2009) in August.
-
Ten people with influenza were admitted to hospital intensive care units in July and 11 in August.
For a more detailed report on respiratory activity in NSW see: http://www.health.nsw.gov.au/PublicHealth/Infectious/influenza_reports.asp
Vaccine-preventable diseases
Measles
Eight cases of measles associated with an outbreak on the NSW North Coast were reported in July and August. The index case was an unimmunised student who had acquired the infection overseas. Six of the cases had close contact with this child at school; one further case occurred in a student attending different classes at the school.
The proportion of children who are reported to be fully vaccinated at 5 years of age in some North Coast communities is lower (61–93%) than in other parts of NSW (89–93%).
Three cases of measles were reported on the NSW Central Coast in August. The first case occurred in an unimmunised child who had acquired the infection overseas. Two subsequent cases occurred: one in an unimmunised sibling of the child and the other in a community contact of the child.
As previously reported, many people who were born after 1965 may not be immune to measles because they have neither acquired the measles infection nor received two doses of a measles vaccine. Measles vaccine is now routinely given to infants at 12 months and at 4 years, and this confers long-lasting immunity in 99% of recipients. These recent outbreaks highlight the importance of complete measles immunisation, particularly prior to overseas travel.
Meningococcal disease
Sixteen cases of meningococcal disease were reported in NSW in July and August. The ages of the affected people ranged from 0 to 67 years (six were aged less than 5 years). Six cases were caused by serogroup B, while serogroups C and Y caused one case each. For the remaining eight cases the serogroup was unknown.
Twenty-three confirmed cases and three clinically diagnosed cases were reported in the same period in 2009.
A free vaccine for serogroup C meningococcal disease is available for infants at 12 months of age. Consequently, serogroup C meningococcal disease is now mainly seen in adults and in unimmunised children. In NSW in 2009, 80% of cases of meningococcal disease (where the serogroup was known) were caused by serogroup B, for which there is no vaccine.
Pertussis (whooping cough)
During July and August, 862 cases of pertussis were reported in NSW. This is significantly lower than the number of cases reported for the same period in 2009 (1250 cases), however this total represents an increase in notifications over May and June 2010 when 684 cases were notified in NSW.
A free vaccine is available for infants at 2, 4 and 6 months (the first dose can be given as early as 6 weeks of age) with a booster dose at 4 years (which can be given from 3 years and 6 months of age). Immunisation reduces the risk of infection, however the vaccine does not provide lifelong protection, and re-infection can occur. Because pertussis immunity wanes over time, many older children and adults are susceptible to infection and can be the source of new infections in infants. For a limited time, free pertussis (dTpa) vaccine is available for all new parents, grandparents and any other adults who will regularly care for infants less than 12 months of age. Free vaccine is also provided to Year 7 and Year 10 students as part of the NSW School-based Vaccination Program from 2010.
Haemophilus influenza type b invasive infection
Three cases of Haemophilus influenza type b invasive infection (Hib) were reported in NSW in July and August. One case occurred in an infant too young to be fully immunised, while the other cases occurred in adults. For the same period in 2009, there were no cases of Hib reported in NSW in any age group.
Sexually transmissible infections
Lymphogranuloma venereum
So far this year, 29 cases of lymphogranuloma venereum (LGV) have been reported in NSW, including five cases with onset in July and seven cases with onset in August. Gay men living in inner metropolitan Sydney have been most affected and the majority of cases have been acquired locally. Most patients have presented with moderate to severe proctitis. LGV in this outbreak is being caused by Chlamydia trachomatis serogroup L2b.
LGV is a rare sexually transmitted chlamydial infection that spreads through unprotected vaginal, anal or oral sexual contact, especially if there is trauma to the skin or mucous membranes. Men who have sex with men, especially those that have unprotected anal sex, are at greatest risk. The bacteria that cause LGV are rare types of chlamydia, however LGV infection is a more aggressive disease than common chlamydial infections. The infection is treated with an extended course of antibiotics.
In response to an increased number of cases reported in May, NSW Health issued an alert to general practitioners in inner Sydney. This alert included information on clinical presentation, diagnosis, treatment and public health management (including contact tracing). Since this time, laboratories have reported increased testing requests for LGV. Information about LGV was also included in the gay press.
Co-infection with other sexually transmissible infections occurs frequently in gay men with LGV and a large proportion of cases overseas have been reported to have HIV. The outbreak in NSW is likely to also include a large proportion of HIV positive men. Active case finding is an important part of a comprehensive management plan and this should include notification and assessment of all sexual partners of the index patient from 1 month prior to their first symptoms.