Communicable Diseases Report, NSW, September and October 2011
Communicable Diseases BranchNSW Department of Health
NSW Public Health Bulletin 22(12) 238-243 https://doi.org/10.1071/NB11049
Published: 22 December 2011
| For updated information, including data and facts on specific diseases, visit www.health.nsw.gov.au and click on Public Health and then Infectious Diseases. The communicable diseases site is available at: http://www.health.nsw.gov.au/publichealth/infectious/index.asp. |
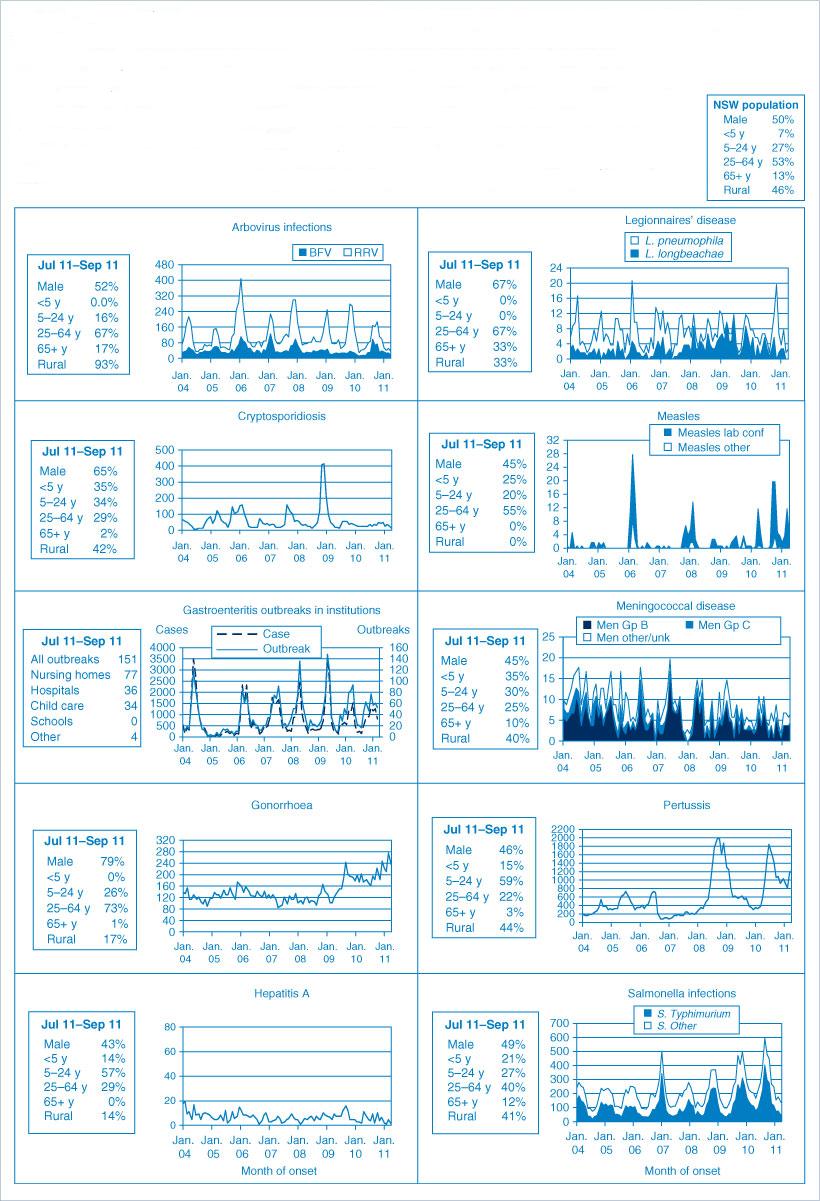
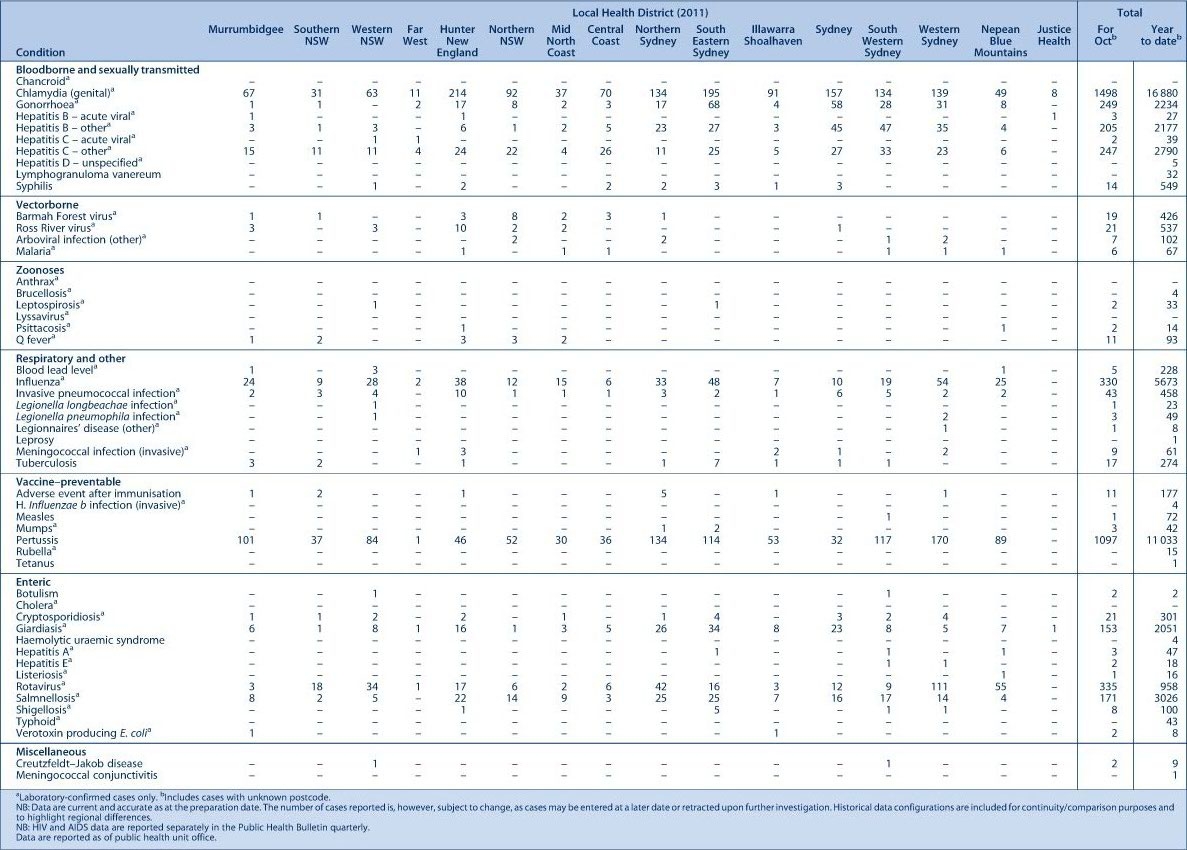
Figure 1 and Tables 1 and 2 show notifications of communicable diseases received in September and October 2011 in New South Wales (NSW).

|
|
Enteric infections
Outbreaks of foodborne disease
Four outbreaks of gastrointestinal disease thought to be due to consumption of contaminated food were reported in September and October 2011. Three outbreaks were identified through complaints to the NSW Food Authority (NSWFA) and one outbreak was identified through reports to a public health unit. For one of these outbreaks, the causative organism was identified as Campylobacter; a pathogen was not identified in the other three outbreaks.
In one outbreak, identified through a complaint about a restaurant to the NSW Food Authority, six people from a group of 20 work colleagues developed diarrhoea 12 hours after eating lunch. The people who became ill ate a chicken curry dish with rice. NSW Food Authority investigated the premises and found that chicken curries were cooked daily, usually stored in a cool room and reheated later. The chicken curry served to this group was likely made two days previously. Bacterial toxins, such as Clostridium perfringens or Bacillus cereus can multiply during slow cooling processes. The restaurant was advised to immediately shorten the cooling step to reduce the opportunity for bacterial growth.
The second outbreak was identified through reports of gastrointestinal illness to a public health unit. Eighty-seven of approximately 500 people who attended a function developed vomiting and diarrhoea 24 hours after eating dinner. The function was catered by a commercial catering business. Just over half of the people (59%) who attended the dinner were surveyed. A poached prawn salad was found to be associated with illness (Odds Ratio = 6.3; Confidence Interval 3.2–13.1). The salad was assembled from pre-prepared products and involved no further cooking steps. As there was no food available to be sampled after the function, it was not possible to identify a specific ingredient as the source of illness, or the point of contamination. Good hygiene was reported by food handlers and the catering manager. No stool samples were submitted by any of the case-patients so the pathogen could not be confirmed in this outbreak, although the clinical picture suggests a viral pathogen.
In the third outbreak, a complaint was made to the NSW Food Authority after two friends became ill with diarrhoea, abdominal pain, nausea and headache, 9 to 10 hours after sharing a meal of Chinese food. Symptoms lasted for approximately 5 days. One case-patient submitted a stool sample that was positive for Campylobacter. The only other possible exposure was another shared breakfast meal, consumed 5 days before illness onset. NSW Food Authority reviewed the database for other complaints about both restaurants, but due to multiple shared exposures and lack of high-risk foods for Campylobacter, site visits were not conducted. The source and vehicle remain unknown, although an incubation period of 5 days and the reported symptoms are consistent with the campylobacteriosis diagnosis.
The fourth outbreak was identified through a complaint about a bakery made to the NSW Food Authority. A group of three people developed abdominal cramps, vomiting and diarrhoea 10 hours after eating Vietnamese pork rolls. This was the only common meal consumed by the three people. The NSW Food Authority inspected the premises and found issues such as the use of raw egg batter, the potential for cross contamination from raw chicken stored in the fridge, and inadequate cleaning and sanitising of food equipment and contact surfaces. Food samples and environmental swabs were taken but no pathogen was identified. However, it was considered that the poor adherence to food safety standards could have led to contamination from raw foods, causing illness. The Food Authority issued an improvement notice the next day in respect to all the defects. Re-inspection of the business premises confirmed that all cleaning, hygiene and food safety defects had been corrected in accordance with the directions of the improvement notice.
Outbreaks of gastroenteritis in institutional settings
In September and October 2011, 65 outbreaks of gastroenteritis in institutions were reported, affecting 898 people. Twenty-nine outbreaks occurred in aged-care facilities, 17 in child-care centres, 17 in hospitals and 2 in other facilities. All these outbreaks appear to have been caused by person-to-person spread of a viral illness. In 42 (65%) outbreaks, one or more stool specimens were collected. In 18 (43%) of these, norovirus was detected. Rotavirus was detected in six (14%) outbreaks (norovirus was also identified in one of these outbreaks). Clostridium difficile was detected in three outbreaks along with norovirus; this finding was thought to be coincidental during a viral gastroenteritis outbreak. In 13 outbreaks, all stool specimens were negative for pathogens. Results for six outbreaks are still outstanding. Stool specimens for laboratory testing were not available for the remaining 23 (35%) outbreaks.
Viral gastroenteritis increases in winter months. Public health units encourage institutions to submit stool specimens from cases for testing during an outbreak to help determine the cause of the outbreak (for further information see Control guidelines for gastrointestinal outbreaks in institutions).
Bloodborne virus
HIV infection
The 2010 annual report on HIV infections in NSW has been published on the NSW Health website (http://www.health.nsw.gov.au/resources/publichealth/infectious/diseases/pdf/new_hiv_2010_summary.pdf). There were 307 people newly diagnosed with HIV infections notified in NSW, which was similar to the number notified in 2009 (n = 329). In 2010, 357 HIV-positive tests were reported from reference laboratories for people that had not been previously diagnosed with HIV infection in NSW. Of these, 50 (14%) were found to have been previously diagnosed with HIV infection elsewhere, or they were not NSW residents. The remaining 307 were NSW residents newly diagnosed with HIV. A total of 282 (92%) were male and the median age at diagnosis was 38 years. Most cases were reported to be homosexually acquired (234; 76%), and the remaining acquisition was identified as heterosexual (50; 16%), injecting drug use (9; 3%), mother-to-child transmission (1; 0.3%) and other or unknown sources (13; 4%). Promoting safer sex practices among males with homosexual exposures and regular testing in this group remain important.
Respiratory infections
Influenza
Influenza activity in NSW, as measured by the number of people who presented to 56 select Emergency Departments with influenza-like illness, and the number of patients who tested positive for influenza at diagnostic laboratories was moderate during September and October 2011. The rate of laboratory-confirmed influenza activity has been declining steadily since activity peaked in mid July 2011.
There were 204 presentations (rate 1.4 per 1000 presentations) for September, and 122 presentations (rate 0.8 per 1000 presentations) for October to select Emergency Departments with influenza-like illness. There were 332 (7%) cases of laboratory-confirmed influenza reported in September; including 143 (43%) influenza A (negative for H1N1 2009) presumed to be influenza A (H3), 150 (45%) influenza B, and the remaining 38 (12%) influenza A H1N1 2009. There were 90 (3%) cases of laboratory-confirmed influenza reported in October, including 46 (51%) influenza A (negative for H1N1 2009) presumed to be influenza A (H3)), 26 (29%) influenza B, and the remaining 18 (20%) influenza A H1N1 2009.
For a more detailed report on respiratory activity in NSW see: http://www.health.nsw.gov.au/PublicHealth/Infectious/influenza_reports.asp.
Vaccine-preventable diseases
Meningococcal disease
Fourteen confirmed cases of meningococcal disease were notified in September and October 2011. Of these, nine cases were due to serogroup B, one case was serogroup C, one case was serogroup Y and the serogroup was unknown for the remaining three cases.
A free vaccine for serogroup C meningococcal disease is available for infants at 12 months of age.1 Consequently, serogroup C disease is now seen mainly in adults and in unimmunised children. In NSW this year, 81% of cases of meningococcal disease where the serogroup was known were caused by serogroup B, for which there is no vaccine. One case of serogroup C disease in an adult was notified this year.
Measles
Seven cases of measles were notified in NSW in September and October 2011. Two case-patients were aged between 0–4 years and the remainder were young adults aged between 15–39 years. One case-patient was reported to have been vaccinated.
Many Australian-born people who are now aged between 20 and 40 years may not have received any, let alone two, doses of measles vaccination required for best protection, and do not have immunity from past infection. Measles mumps and rubella (MMR) vaccine is now routinely given at 12 months of age and again at 4 years (although it can be given from 3½ years of age); two MMR vaccines give long-lasting immunity.
An accurate immunisation history is often difficult to determine in adults who may be unsure of the exact details of the vaccines they received in childhood and do not have written records. There is no whole-of-life immunisation register that can be used to verify the vaccines adults have been given. General practitioners (GPs) are able to provide free MMR vaccine to anyone born after 1966 who has not received two doses of vaccine or who is unsure of his or her vaccination history.
Pertussis (whooping cough)
In September and October 2011, 2400 cases of pertussis were notified in NSW compared to 2443 cases for the same period in 2010. In total, 11 033 cases of pertussis have been reported up to 31 October 2011 compared to 5845 for the same period in 2010. To date in 2011, the highest number of notifications was reported in children aged between 5–9 years (3365 cases), 0–4 years (2030 cases) and young people aged between 10–14 years (1900 cases).
A free vaccine is recommended for infants at 2, 4 and 6 months although the first dose can be given as early as 6 weeks of age. A booster dose is recommended at 4 years but this can be given as early as 3½ years of age.2
Immunisation reduces the risk of infection, however the vaccine does not provide lifelong protection, and re-infection can occur.1 Because pertussis immunity wanes over time, many older children and adults are susceptible to infection and can be the source of new infections in infants.3 For a limited time, NSW Health is providing free pertussis (dTpa) vaccine through GPs to all new parents, grandparents and any other adults who will regularly care for infants less than 12 months of age. Free vaccine boosters are also provided to Year 7 and Year 10 students as part of NSW Health’s School-based Vaccination Program.
References
[1] National Health and Medical Research Council. The Australian Immunisation Handbook. 9th ed. Canberra: Australian Government Department of Health and Ageing; 2008.[2] Australian Technical Group on Immunisation (ATAGI). 41st Meeting: 15–16 October 2009, summary of outcomes. Available from: http://immunise.health.gov.au/internet/immunise/publishing.nsf/Content/E7E989916C4FCAD8CA2576BF007D6B6E/$File/ATAGI-41-bulletin.pdf. (Cited 30 March 2010.)
[3] Wendelboe AM, Njamkepo E, Bourillon A, Floret D, Gaudelus J, Gerber M. Transmission of Bordetella pertussis to young infants. Pediatr Infect Dis J 2007; 26 293–9.
| Transmission of Bordetella pertussis to young infants.Crossref | GoogleScholarGoogle Scholar |