Communicable Diseases Report, NSW, January and February 2012
Communicable Diseases BranchNSW Ministry of Health
NSW Public Health Bulletin 23(4) 94-98 https://doi.org/10.1071/NB12072
Published: 13 June 2012
| For updated information, including data and information on specific diseases, visit www.health.nsw.gov.au and click on Public Health and then Infectious Diseases. The communicable diseases site is available at: http://www.health.nsw.gov.au/publichealth/infectious/index.asp. |
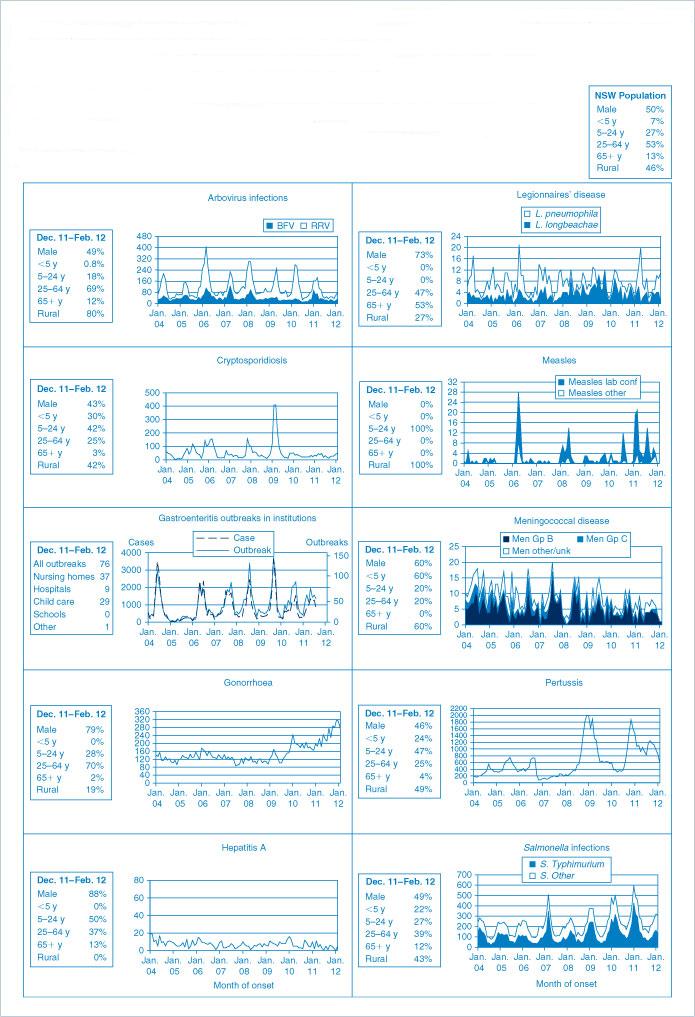
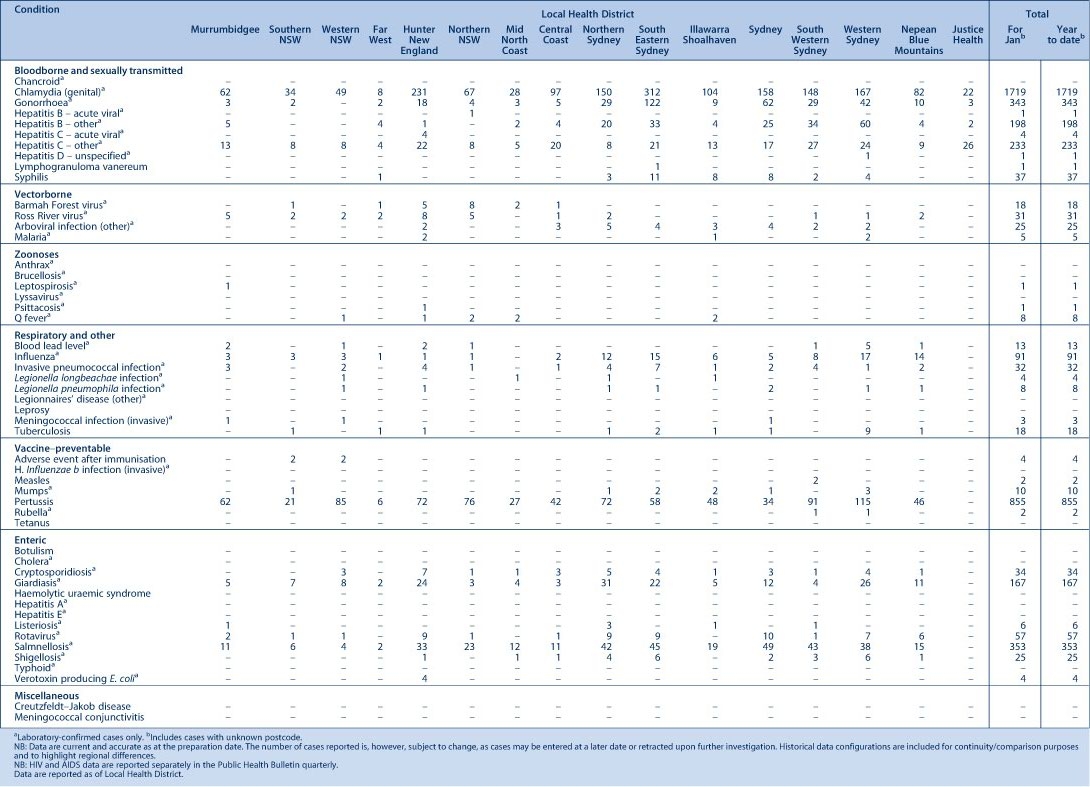
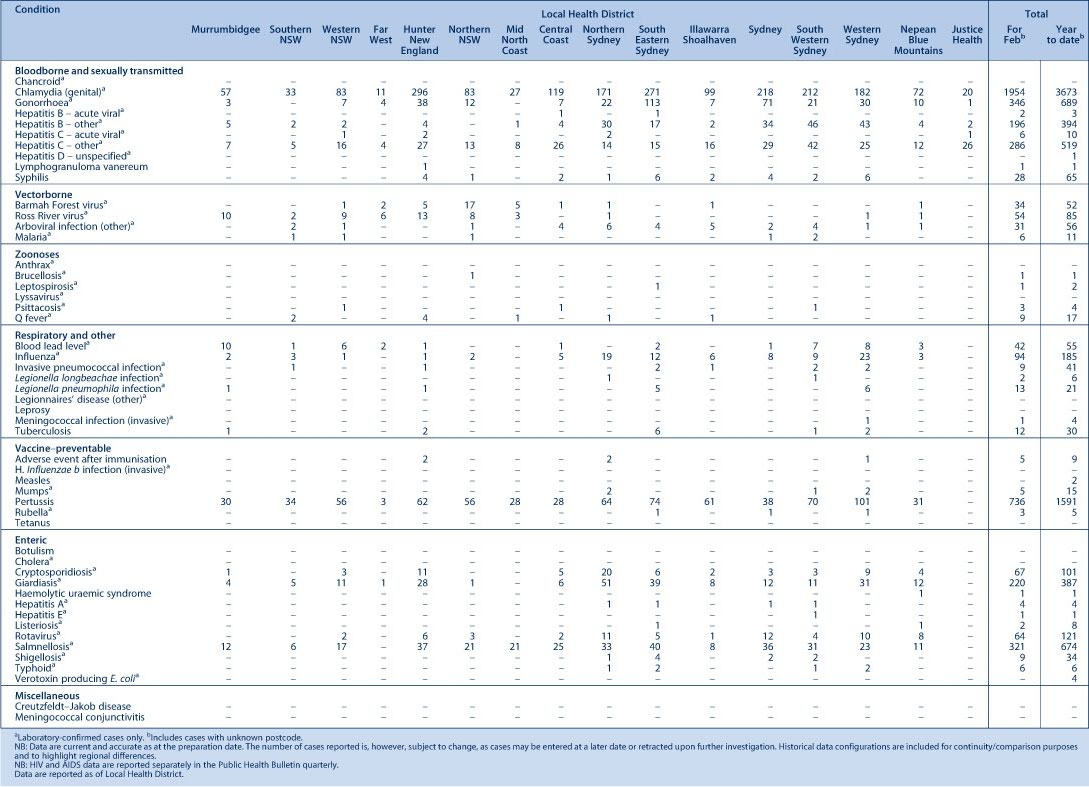
Figure 1 and Tables 1 and 2 show notifications of communicable diseases received in January and February 2012 in New South Wales (NSW).
|
|
Enteric infections
Outbreaks of suspected foodborne disease
Nine outbreaks of gastrointestinal disease, thought to be due to the consumption of contaminated food and which affected a total of 64 people, were reported for January and February 2012. This is half as many outbreaks reported for the same period last year. These outbreaks were linked to restaurants or cafes (7), a private residence (1) and a conference (1). Of the nine outbreaks, five were identified through complaints to the NSW Food Authority, one was identified through an emergency department report to a public health unit, one was reported directly to a public health unit and two were detected through the monitoring of laboratory notifications of Salmonella clustered in time and space. Stool samples were tested in six outbreaks. Salmonella Typhimurium was found to be the cause in four of these outbreaks and Salmonella Give in one.
There were insufficient data to draw conclusions about the likely cause for six outbreaks. For three outbreaks an analysis of the foods consumed showed an association between illness and consumption of partially cooked egg products. In two of these outbreaks the cases exclusively consumed fried ice cream from Chinese restaurants. Fried ice cream is known to be a high-risk food for salmonellosis because the very quick cook time is unlikely to kill any pathogens present in the egg used to coat the ice cream ball. In the other outbreak, the illness was diagnosed in those who had consumed scrambled eggs from a cafe. In this outbreak, eggs were pooled and stored at a temperature where salmonella could multiply. The dishes were then cooked to only a soft scramble, which meant the temperature was not sufficient to kill any Salmonella present.
Outbreaks of gastroenteritis in institutional settings
In January and February 2012, 63 outbreaks of gastroenteritis in institutions were reported, affecting 686 people, a similar number to the same period last year (61 outbreaks). Twenty-seven outbreaks occurred in aged-care facilities, 31 in child-care centres, 4 in hospitals and 1 in a camp setting. All these outbreaks appear to have been caused by person-to-person spread of a viral illness. In 27 (43%) outbreaks one or more stool specimens were collected. In 12 (44%) of these, norovirus was detected. Rotavirus was detected in 3 (11%) outbreaks.
Cryptosporidium was detected in one outbreak along with norovirus; this finding was thought to be coincidental during a viral gastroenteritis outbreak. In nine (33%) outbreaks all stool specimens were negative for pathogens. Results for three outbreaks are still outstanding.
Viral gastroenteritis increases in winter months. Public health units encourage institutions to submit stool specimens from case-patients for testing during an outbreak to help determine the cause of the outbreak (for further information see: Guidelines for the public health management of gastroenteritis outbreaks due to norovirus or suspected viral agents in Australia available at: http://www.health.gov.au/internet/publications/publishing.nsf/Content/cda-cdna-norovirus.htm-l).
Respiratory infections
Influenza
Influenza activity in NSW, as measured by the number of people who presented with influenza-like illness to 56 select emergency departments and the number of patients who tested positive for influenza at diagnostic laboratories, was low during January and February 2012.
In January, there were:
-
67 presentations to emergency departments (rate 0.4 per 1000 presentations)
-
21 cases of laboratory-confirmed influenza (rate 1.4 per 100 samples) including:
-
7 (33%) influenza B
-
6 (29%) influenza A – negative for pH1N1 – presumed to be influenza A (H3N2)
-
4 (19%) influenza A (H3N2)
-
4 (19%) influenza A (pH1N1).
In February, there were:
-
86 presentations to emergency departments (rate 0.4 per 1000 presentations)
-
45 cases of laboratory-confirmed influenza (rate 1.9 per 100 samples)
-
20 (44%) influenza A – negative for pH1N1 – presumed to be influenza A (H3N2)
-
15 (33%) influenza B
-
9 (20%) influenza A (H3N2)
-
1 (2%) influenza A (pH1N1).
Legionnaires’ disease
There were 27 cases of Legionnaires’ disease reported in January and February 2012. Of these, 21 cases were due to Legionella pneumophila and six cases were due to Legionella longbeachae. Despite careful interviews with case-patients for common exposures and a review of the potential sources of infection (including cooling towers), no common environmental sources were identified for these cases.
Legionella bacteria can cause severe pneumonia if aerosolised water or dust that contains the bacteria is inhaled by susceptible people. Some air-conditioning cooling towers have been identified as the source of Legionnaires’ disease outbreaks in the past as they can become contaminated by Legionella bacteria which are then aerosolised. There are requirements for building owners to register their cooling towers with local councils and to maintain cooling towers to minimise the growth of Legionella bacteria in the cooling tower water. For further information, see: http://www.health.nsw.gov.au/factsheets/environmental/legion_control.html.
Vaccine-preventable diseases
Meningococcal disease
Four cases of meningococcal disease were notified in NSW in January and February 2012 (three in January and one in February); the age of the cases ranged from 0 to 50 years and included two cases aged under 5 years. One of these four cases was an adult from regional NSW whose death was notified in this period. All four cases of meningococcal disease were caused by serogroup B, for which there is no vaccine.
The number of cases has decreased from the same period in 2011, when there were 13 cases notified. The ages of these case-patients ranged from 0 to 60 years (five aged under 5 years) and 6 of these cases were caused by serogroup B.
It is recommended that a single dose of vaccine against meningococcal disease be given to all children at the age of 12 months as well as those individuals at high risk of disease. 1
Pertussis (whooping cough)
During January and February 2012, 1591 cases of pertussis were notified in NSW. This number is lower than that reported for the same period in 2011 (2698 cases). Caution should be exercised when interpreting these data because notifications of disease can be delayed.
Immunisation of babies remains an important strategy to provide protection for an age group most at risk of severe illness. A free vaccine administered to infants at 2, 4 and 6 months of age is available. It is currently recommended that the first dose be provided as early as 6 weeks of age and the subsequent booster dose at 3½ to 4 years.
Sexually transmitted infections
Syphilis
There were 65 notifications of infectious syphilis cases during January and February; this number has slightly decreased from the previous period of November and December 2011 with 73 notifications. The majority of notifications from January and February 2012 were in men aged between 20 and 50 years. Of these, notifications among young men aged 20 to 24 years have increased compared to the same period in 2011 (17% in 2012 compared to 3% in 2011).
Syphilis is a highly infectious sexually transmitted disease that is spread through vaginal, anal or oral sex through skin-to-skin contact. Syphilis is highly contagious during the primary and secondary stages of the disease when the sore or rash is present. Those most at risk include men who have sex with men, people with human immunodeficiency virus (HIV) infection, and Aboriginal people living in communities that are remote or have poor access to health services.