Ongoing transmission of tuberculosis in Aboriginal communities in NSW
Sue Devlin A C and Erin Passmore BA North Coast Public Health Unit
B NSW Public Health Officer Training Program, NSW Ministry of Health
C Corresponding author. Email: sue.devlin@ncahs.health.nsw.gov.au
NSW Public Health Bulletin 24(1) 38-42 https://doi.org/10.1071/NB12113
Published: 15 July 2013
Abstract
This report describes the ongoing transmission of tuberculosis in Aboriginal communities in NSW. From October 2000 to July 2012 there were 30 linked cases of tuberculosis diagnosed in Aboriginal people – 22 in the North Coast area of NSW, with a further three cases in Sydney and five in southern Queensland. It is likely that a range of factors have contributed to this ongoing transmission, including delayed diagnosis, the extensive social connections within the communities affected, and the highly mobile living arrangements of many of those affected. Cases have continued to emerge despite implementation of tuberculosis control measures in line with state and international protocols. Tuberculosis control staff are working in partnership with Aboriginal communities to identify and implement appropriate tuberculosis control strategies.
Tuberculosis (TB) is an important public health issue and a leading cause of death worldwide.1 The public health burden of TB is substantial, even in developed countries with comprehensive TB control programs. In Australia, the incidence of TB is low (6.0 cases per 100 000 population in 2009), with the majority of cases occurring in migrants from countries with a high incidence of TB.2 For Aboriginal Australians, the incidence of TB has been declining since 2002 but remains over five times higher than for Australian-born non-Aboriginal people (4.8 versus 0.9 per 100 000 population).2 The persistence of TB in Aboriginal people has been attributed to poor living conditions and malnutrition compounded by chronic diseases and alcohol use.3–5 The aim of this paper is to describe the epidemiology of a cluster of TB cases with ongoing transmission amongst Aboriginal people in New South Wales (NSW), and the public health response.
Methods
This paper presents results up to July 2012, however new cases continue to be identified and the public health response is ongoing.
TB is a notifiable disease under the NSW Public Health Act 2010. The data presented in this paper have been collected as a part of routine TB control procedures implemented in accordance with the Act. The data were obtained from the NSW Notifiable Conditions Information Management System, a statewide database of disease notifications held by NSW Health. Standard TB case definitions are used.6 Clustered cases are defined as: MIRU-linked cases – laboratory-confirmed TB cases with the mycobacterial interspersed repetitive unit (MIRU) pattern 23′3425153322; and epidemiologically-linked cases – clinical TB cases with no TB organism identified but with epidemiological links to a MIRU cluster case. Incidence rates per 100 000 population were calculated using the Australian Bureau of Statistics estimated mid-year NSW populations for 2000–2012, obtained from NSW Health’s Secure Analytics for Population Health Research and Intelligence.
Results
Identification of cases in the cluster
A total of 30 linked cases of TB were identified in the period October 2000–July 2012 (Figure 1). Twenty-six of the 30 cases shared the MIRU pattern for this cluster. The remaining four were clinically diagnosed cases that had strong epidemiological links to the cluster (e.g. child household contacts of cases). One person developed TB twice and was counted twice in the cluster. This person had household contact with several cases following successful completion of directly observed treatment and so was considered a case of reinfection. Most cases (n = 22) were diagnosed on the NSW North Coast (the area covered by the Northern NSW and Mid North Coast Local Health Districts), with a further three cases in Sydney and five in Queensland. The MIRU pattern for this cluster is found almost exclusively in Aboriginal people. Only one non-Aboriginal person in Australia has been identified as having had this MIRU pattern since 2000: an elderly overseas-born woman in Victoria. This woman had no identifiable epidemiological link to the cluster cases, and was therefore excluded from the cluster.
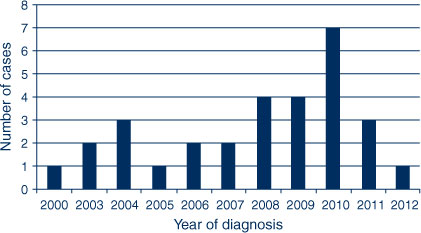
|
The presence of a cluster became evident when several cases of TB were diagnosed through contact tracing in response to an Aboriginal person diagnosed with pulmonary smear-positive TB on the NSW North Coast in 2003. This person was estimated to have been infectious for 4 months prior to diagnosis, and assisted with the contact tracing by disclosing a wide network of family and friends. In 2004, an Aboriginal person in Queensland who was newly diagnosed with TB and a North Coast Aboriginal person who had been diagnosed with TB in 2000 were found to share the same MIRU pattern as the initial case.
MIRU-linked cases continued to emerge despite implementation of TB control measures in line with state and international protocols6,7 and additional community-based screening where possible. Some cases were known contacts of previous cases, however the geographic spread of the disease broadened and the epidemiological links for some cases were not immediately evident.
In 2006 an Aboriginal person diagnosed with MIRU-linked TB in Sydney reported travelling to the North Coast periodically however no epidemiological links with the North Coast cases could be identified. Two further MIRU-linked cases were diagnosed in Sydney: one person diagnosed in 2009 who reported “knowing” the first Sydney case and who had a history of travel to the North Coast; and one person diagnosed in 2012 with no identified connections to the North Coast or any cluster cases. A Queensland person diagnosed with TB in 2006 was MIRU-linked to the cluster. It was subsequently discovered that this person moved in the same social circles as a North Coast person diagnosed in 2005, at the time the North Coast person was infectious. A household sub-cluster with three additional cases emerged around this Queensland case.
The diagnosis in 2010 of a further five adults with TB on the North Coast revealed significant information about the connections between the North Coast cases, their contacts, and their mobility practices and patterns. The North Coast cases diagnosed in 2010 had epidemiological connections with multiple cases in this TB cluster.
Characteristics of the cluster
Twenty-two of the 30 cases (73%) were male; the average age of cases was 33.2 years (Standard Deviation = 15.8) (Figure 2). Most cases (n = 22, 73%) presented with pulmonary smear-positive TB; the remainder presented with pulmonary smear-negative TB and extrapulmonary TB. Cases reported having symptoms of TB for an average of 5 months prior to seeking medical attention or being identified through contact tracing (range 1–13 months). Eight cases (27%) were identified through contact tracing. Four of the 30 cases (13%) were children, all of whom had household contact with an adult with pulmonary TB. This particular MIRU pattern is susceptible to first-line TB antibiotics, and all cases completed treatment. There have been no known deaths due to TB in this cluster.
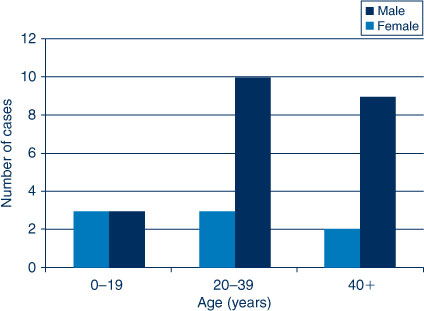
|
Since October 2000, there have been 55 notifications of TB in Aboriginal people in NSW, 25 of which (45%) are part of this cluster. The average annual TB notification rate for Aboriginal people in the North Coast area in the period 2000–2011 was 12.1 notifications per 100 000 population. This rate is elevated compared to Aboriginal people in the rest of NSW (1.7 per 100 000 population), and compared to non-Aboriginal people in both the North Coast area (1.6 notifications per 100 000 population) and the rest of NSW (7.2 notifications per 100 000 population). The increased rate of TB in Aboriginal people in the North Coast area is entirely due to this cluster – of the TB notifications in Aboriginal people in the North Coast area since 2000, all but one case has been linked to this cluster.
The epidemiological links between these cases are complex (Figure 3). Rather than a complete ‘map’ of links between cases, the connections shown in Figure 3 reflect the depth of information disclosed by each case and/or knowledge amassed by the North Coast TB Prevention and Control Team (Team TB) through its work in the field. The understanding of connections between cases evolves over time, and depends on the cultural competence of Team TB to develop mutually trusting and respectful relationships with individuals and communities. As the cluster continues it becomes increasingly difficult to identify patterns of transmission and infection. The cases have extensive overlapping social networks and many cases lived in overcrowded households and were highly mobile during their long infectious period.
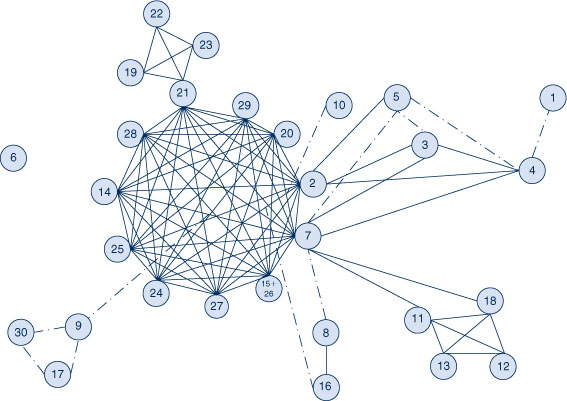
|
Equity aspects of the cluster
This TB cluster represents a health inequity between Aboriginal and non-Aboriginal Australians in NSW. The history of displacement, disempowerment, grief and loss experienced by Aboriginal people continues to impact on their health and wellbeing and the constellation of social factors that contribute to TB are a reflection of the broader health inequities between Aboriginal and non-Aboriginal people. In this TB cluster, social risk factors include transient homelessness, living in crowded houses, unemployment and incarceration. Most of the adult cases in this cluster have a history of only seeking medical care when injured or extremely unwell, and their TB symptoms may have been masked by other health and wellbeing issues such as drug and alcohol use, smoking and depression. Many of the people with TB in this cluster are the most vulnerable individuals within already marginalised communities. For many, daily life challenges and competing health conditions compound their experience of TB and their ability to seek healthcare.
However, the strengths of the Aboriginal people and communities affected by this cluster must be acknowledged. Team TB recognise examples of individual healing; strong families; individual, family and community action; evidence of adults coping, recovering and flourishing. It is a testament to the strength and resilience of the people who have had active TB, and their family and community support system, that despite these life challenges and the burden of shame and stigma, they have all completed treatment and many have made personal sacrifices to benefit the community.
The North Coast TB Team response to the cluster
To identify contacts of people with TB, Team TB utilise an intensive household contact tracing8 approach. This involves having wide-ranging discussions (“yarning”) with the person, family members and others involved with the community to identify social and family networks and places the person visits (e.g. households, congregation areas), then offering screening to the people at these locations. TB screening, including clinical assessment of symptoms, tuberculin skin tests (TSTs) and/or chest X-rays, has been offered widely to the Aboriginal people in North Coast towns. This is in response to the Aboriginal communities’ concern; recognition of the extended social networks and high mobility in Aboriginal communities which result in a high number of close contacts, many of whom can be difficult to identify and/or locate; leads provided through contact tracing; and identification that not all infected people were being reached through contact tracing models. Community-wide screening is also utilised when the community is not aware of the identity of a case as it allows for confidentiality to be maintained. These screening approaches have been developed by Team TB in conjunction with communities and local Aboriginal Health Workers. Early in the public health response to the cluster, ‘concentric circle’ contact tracing was used in line with NSW guidelines,6 however retrospective identification of connections between cases and TST data revealed that with this approach people at risk of infection were not always nominated.
Team TB’s response to the cluster is guided by the principles of cultural respect, equity and partnership with Aboriginal communities9 and community engagement is central to the public health response. In particular, Team TB has invested in the development of cultural competence and awareness sharing with the community (i.e. two-way learning). They have consulted with Aboriginal community groups and leaders, a range of government and non-government service providers, and Aboriginal people affected by TB to develop appropriate response strategies. Team TB participates in a range of activities with communities to facilitate shared ownership of solutions to the ongoing transmission of TB. The recruitment of Aboriginal Health Workers into Team TB has strengthened its capacity to develop and implement strategies that are acceptable to all parties, while being feasible within the broader social and cultural context.
Discussion
This paper describes the only reported instance of ongoing transmission of TB in NSW, the public health response to the cluster, and the rationale for this response.
The limitations of routine TB contact tracing approaches have been documented in the international literature10,11 and are amplified in vulnerable groups such as Aboriginal people.12 In this cluster, cases were identified using a combination of contact tracing and community-wide screening for Aboriginal people. Novel methods of contact tracing that focus on social networks, locations and behavioural factors have been successfully used to examine TB clusters and outbreaks overseas13–16 and their application in Australian Aboriginal communities warrants further investigation.
The uptake of treatment for latent TB infection remains a major ongoing challenge in the response to the cluster. More than 1000 TSTs have been provided as part of screening, and all individuals with latent TB infection are offered preventive treatment. Uptake and completion is high in high-risk child contacts, facilitated by directly observed treatment or support and monitoring by TB nurses. However, many infected adults decline treatment for latent TB infection or fail to complete the 6-month course of isoniazid. This highlights the significant ethical tension between individual autonomy and community benefit.
To date, TB prevention and control activities have concentrated on providing access to clinical services through delivery of primary care focused on early diagnosis and timely and effective treatment. The ongoing transmission suggests closing the gap in TB rates between Aboriginal and non-Aboriginal Australians involves acknowledging that TB is embedded in a complex system17 influenced by contemporary and historical social determinants of health. It is time to consider a comprehensive primary health care approach that addresses the range of social, environmental and structural factors that contribute to TB and ill-health, and those that contribute to good health.18 Team TB is committed to operating on social justice principles with practitioners dedicated to enabling individual clients and communities19 and implementing micro-empowerment strategies (e.g. working with people to build TB management around how and where they live their lives, incorporating social and emotional care into TB management, contributing to community-initiated events and programs for community development, and giving ‘voice’ to people who have been affected by TB).20
Empowerment is a recurrent theme throughout the literature on improving the health and wellbeing of Aboriginal and Torres Strait Islander people. Empowerment is one of the six components of the WHO Stop TB Strategy21 and is incorporated in many TB control programs internationally.22 Furthermore, it is a viable public health strategy23 which can be viewed from two complementary perspectives: empowered communities can control TB and controlling TB can empower communities. It is conceivable that incorporating empowerment into the TB prevention and control model could contribute more to the health of the target group than just the elimination of TB. The challenge is to move from business as usual to develop a deeper understanding of the setting and to explore innovative and novel ways to move from primary care towards primary health care.
Conclusion
The ongoing transmission of TB amongst Aboriginal Australians in NSW suggests closing the gap in TB rates between Aboriginal and non-Aboriginal Australians involves acknowledging that TB is embedded in a complex system influenced by contemporary and historical social determinants of health. An effective response depends on working in partnership with Aboriginal communities to develop strategies for TB control that empower communities and act on these social determinants of health.
Acknowledgments
The public health response to this TB cluster is a collaborative effort. The authors acknowledge the contribution of Aboriginal community members, TB nurses, Aboriginal Health Workers, public health unit staff, clinicians, laboratory scientists, and other government and community organisations in responding to this cluster. The authors also acknowledge the expert guidance provided by the TB Cluster Expert Panel, a subcommittee of the NSW TB Advisory Committee.
References
[1] World Health Organization. Global tuberculosis report 2012. Available at: http://apps.who.int/iris/bitstream/10665/75938/1/9789241564502_eng.pdf (Cited 11 February 2013).[2] Barry C, Waring J, Stapleton R, Konstantinos A;, National Tuberculosis Advisory Committee, for the Communicable Diseases Network Australia Tuberculosis notifications in Australia, 2008 and 2009. Commun Dis Intell 2012; 36 82–94.
[3] Moodie PM. Aboriginal health: Aborigines in Australian society. Canberra: Australian National University Press; 1973.
[4] Abrahams EW. Tuberculosis in Indigenous Australians. Med J Aust 1975; 2 23–7.
| 1223601PubMed |
[5] Robertus LM, Konstantinos A, Hayman NE, Paterson DL. Tuberculosis in the Australian Indigenous population: history, current situation and future challenges. Aust N Z J Public Health 2011; 35 6–9.
| Tuberculosis in the Australian Indigenous population: history, current situation and future challenges.Crossref | GoogleScholarGoogle Scholar | 21299692PubMed |
[6] NSW Health. Control guideline: Tuberculosis. Available at: http://www.health.nsw.gov.au/factsheets/guideline/tuberculosis.html (Cited 28 August 2012).
[7] World Health Organization. Guidelines for treatment of tuberculosis. 4th ed. Geneva: World Health Organization; 2010.
[8] Smart T. HIV and TB in practice for nurses: active TB case finding. HIV & AIDS treatment in practice 2012; 196 2–5.
[9] Aboriginal Services Branch, NSW Department of Community Services, Sydney. Working with Aboriginal people and communities. Available at: http://www.community.nsw.gov.au/docswr/_assets/main/documents/working_with_aboriginal.pdf (Cited 14 February 2013).
[10] Reichler MR, Reves R, Bur S, Thompson V, Mangura BT, Ford J, et al. Evaluation of investigations conducted to detect and prevent transmission of tuberculosis. JAMA 2002; 287 991–5.
| Evaluation of investigations conducted to detect and prevent transmission of tuberculosis.Crossref | GoogleScholarGoogle Scholar | 11866646PubMed |
[11] Marks SM, Taylor Z, Qualls NL, Shrestha-Kuwahara RJ, Wilce MA, Nguyen CH. Outcomes of contact investigations of infectious tuberculosis patients. Am J Respir Crit Care Med 2000; 162 2033–8.
| Outcomes of contact investigations of infectious tuberculosis patients.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BD3M7gt1ymtQ%3D%3D&md5=b46c4756aa8db121145c36049574db66CAS | 11112109PubMed |
[12] Cook VJ, Shah L, Gardy J. Modern contact investigation methods for enhancing tuberculosis control in aboriginal communities. Int J Circumpolar Health 2012; 71 18643
| Modern contact investigation methods for enhancing tuberculosis control in aboriginal communities.Crossref | GoogleScholarGoogle Scholar | 22663943PubMed |
[13] McElroy PD, Rothenberg RB, Varghese R, Woodruff R, Minns GO, Muth SQ, et al. A network-informed approach to investigating a tuberculosis outbreak: implications for enhancing contact investigations. Int J Tuberc Lung Dis 2003; 7 S486–93.
| 1:STN:280:DC%2BD3srps1Srsw%3D%3D&md5=f7d6b0df9b41394f66217ce3302ca6e8CAS | 14677842PubMed |
[14] Fitzpatrick LK, Hardacker JA, Heirendt W, Agerton T, Streicher A, Melnyk H, et al. A preventable outbreak of tuberculosis investigated through an intricate social network. Clin Infect Dis 2001; 33 1801–6.
| A preventable outbreak of tuberculosis investigated through an intricate social network.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BD3MnktVGmsw%3D%3D&md5=5f375ac77fd996661195d91fe80a05e3CAS | 11692291PubMed |
[15] Sterling TR, Thompson D, Stanley RL, McElroy PD, Madison A, Moore K, et al. A multi-state outbreak of tuberculosis among members of a highly mobile social network: implications for tuberculosis elimination. Int J Tuberc Lung Dis 2000; 4 1066–73.
| 1:STN:280:DC%2BD3Mvos1yqtQ%3D%3D&md5=bdac60f426be3079e8ab80f358f002f5CAS | 11092720PubMed |
[16] Cook VJ, Sun SJ, Tapia J, Muth SQ, Arguello DF, Lewis BL, et al. Transmission network analysis in tuberculosis contact investigations. J Infect Dis 2007; 196 1517–27.
| Transmission network analysis in tuberculosis contact investigations.Crossref | GoogleScholarGoogle Scholar | 18008232PubMed |
[17] van Beurden E, Kia A. Wicked problems and health promotion: reflections on learning. Health Promot J Austr 2011; 22 83–4.
| 21819364PubMed |
[18] Keleher H. Why primary health care offers a more comprehensive approach to tackling health inequities than primary care. Aust J Primary Health 2001; 7 57–61.
| Why primary health care offers a more comprehensive approach to tackling health inequities than primary care.Crossref | GoogleScholarGoogle Scholar |
[19] World Health Organization. Ottawa Charter for Health Promotion. Available at: http://www.who.int/healthpromotion/conferences/previous/ottawa/en/ (Cited 16 October 2012).
[20] Tsey K, Whiteside M, Haswell-Elkins M, Bainbridge R, Cadet-James Y, Wilson A. Empowerment and Indigenous Australian health: a synthesis of findings from the Family Wellbeing formative research. Health Soc Care Community 2010; 18 169–79.
| Empowerment and Indigenous Australian health: a synthesis of findings from the Family Wellbeing formative research.Crossref | GoogleScholarGoogle Scholar | 19804554PubMed |
[21] World Health Organization. The Stop TB Strategy. Available at: http://www.who.int/tb/strategy/stop_tb_strategy/en/index.html (Cited 16 October 2012).
[22] World Health Organization and Stop TB Partnership. Empowerment and involvement of tuberculosis patients in tuberculosis control: Documented experiences and interventions. Available at: http://whqlibdoc.who.int/hq/2007/WHO_HTM_STB_2007.39_eng.pdf (Cited 14 February 2013).
[23] Wallerstein N. What is the evidence on effectiveness of empowerment to improve health? Copenhagen: WHO Regional Office for Europe (Health Evidence Network Report); 2006. Available at: http://www.euro.who.int/__data/assets/pdf_file/0010/74656/E88086.pdf (Cited 16 October 2012).

