Communicable Diseases Report, NSW, April–June 2013
Communicable Diseases BranchHealth Protection NSW
NSW Public Health Bulletin 24(3) 143-147 https://doi.org/10.1071/NB13013
Published: 23 December 2013
| For updated information, including data and facts on specific diseases, visit www.health.nsw.gov.au and click on Public Health and then Infectious Diseases. The communicable diseases site is available at: http://www.health.nsw.gov.au/publichealth/infectious/index.asp. |
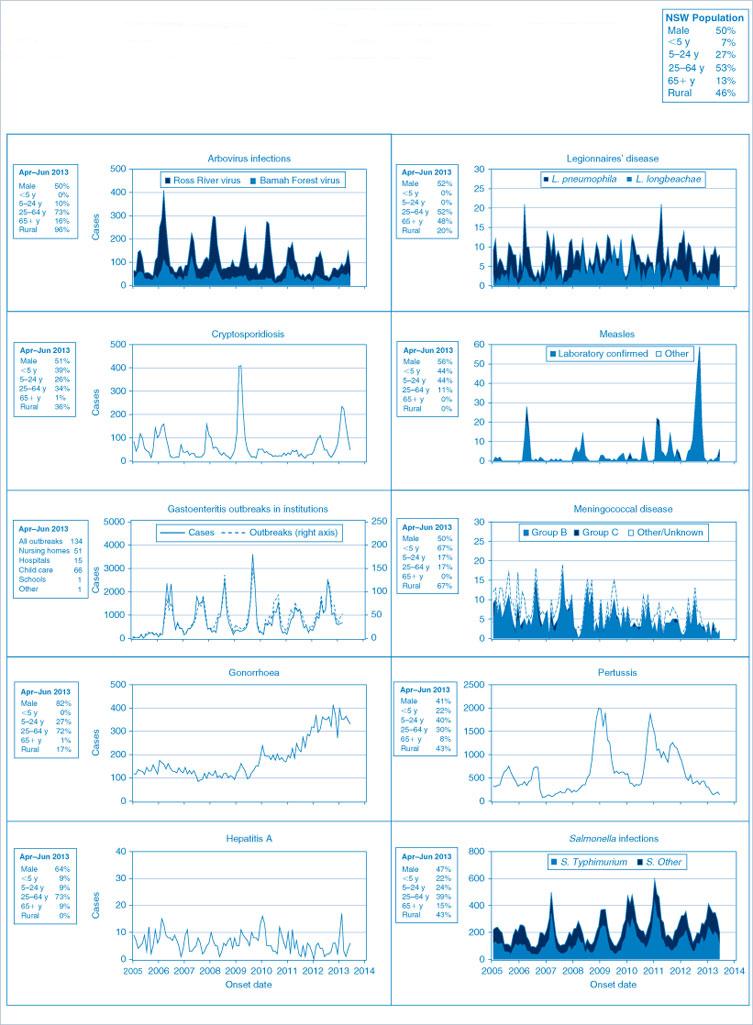
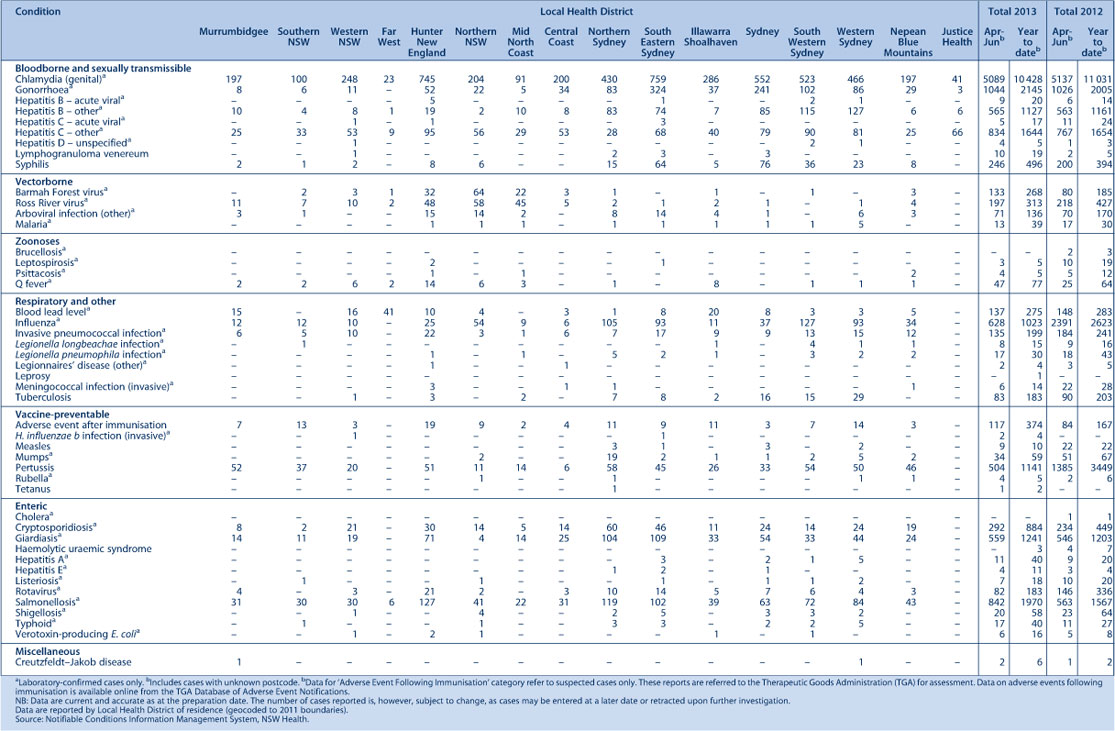
Figure 1 and Table 2 show notifications of communicable diseases with onset between April and June 2013 in New South Wales (NSW).
Enteric infections
Outbreaks of suspected foodborne disease
There were 11 outbreaks of foodborne or suspected foodborne disease investigated by NSW Public Health Units (PHUs) in the second quarter of 2013. Three outbreaks were due to Salmonella Typhimurium, one was due to S. Zanzibar, one was due to Listeria monocytogenes, and one was due to norovirus. The remaining five outbreaks were due to unknown pathogens.
Only three outbreak investigations were able to provide sufficient evidence to identify the source of the infection. The first of these outbreaks was part of a large multi-jurisdictional outbreak of norovirus found in Tasmanian oysters in April 2013. Two groups of people (totalling eight from 10 people) reported vomiting and diarrhoea after eating these oysters in NSW. No specimens were tested but the symptoms were consistent with norovirus and the batches of oysters consumed were those thought to be contaminated in the outbreak. In the second outbreak, a PHU was notified of salmonellosis associated with a dinner party in a private residence in June 2013. Fourteen of the 17 attendees became unwell after eating a meal that contained raw egg béarnaise sauce. In addition, three people who did not attend the dinner party but who consumed leftover food that contained the béarnaise sauce also became unwell. Five of the cases tested positive for S. Typhimurium (MLVA 3-23-23-11-523). The person who cooked the meal, a chef, was provided with information on salmonellosis and the risks of using raw or minimally cooked eggs in food. In the third outbreak, a cluster of L. monocytogenes infections notified within an 8-day period prompted an investigation. All three cases were inpatients in hospitals within the same Local Health District during their incubation period. Food and menu histories revealed that the three cases had consumed profiteroles from the same external commercial supplier on the same day. Products from this supplier were then withdrawn from all NSW hospitals. The NSW Food Authority found that the supplier had previously had a profiterole test positive for Listeria (unspeciated); the positive test had not been reported at the time as it was not a requirement to do so. Two environmental swabs taken from the supplier’s premises tested positive for L. monocytogenes. One of these samples was indistinguishable by MLVA from that found in the three cases. L. innocua was also found in swab samples at the factory site. In consultation with the NSW Food Authority, HealthShare NSW conducted a review of processes for approving suppliers of hospital food, including ensuring Listeria management plans were in place.
Viral gastrointestinal disease
There were 115 reported outbreaks of (suspected) viral gastrointestinal disease in institutions in the second quarter of 2013. Of these, 42 (37%) occurred in aged-care facilities, 56 (49%) occurred in childcare centres, 15 (13%) in hospitals, and one each in a school and a military institution. The outbreaks affected a total of 1612 people.
In 47% (n = 54) of all outbreaks, one or more stool specimens were laboratory tested to identify a possible cause of the outbreak. Norovirus was identified in 31% (n = 17) of these outbreaks. In one outbreak, Salmonella was detected alongside norovirus. Giardia, Cryptosporidium and Clostridium difficile were also each detected in single outbreaks; these were thought to be coincidental findings of pathogens during otherwise viral gastrointestinal outbreaks. Of the 54 outbreaks where one or more stool specimens were tested, 63% (n = 34) of all results were negative for any pathogens.
Respiratory infections
Influenza
Influenza continued to circulate at low levels for most of the second quarter of 2013 although activity rose markedly during June, consistent with the start of the influenza season. There was evidence of co-circulation of influenza A(H1N1)pdm2009, influenza A(H3N2), and influenza B strains. The number of influenza cases notified in this quarter was much lower than for the same period in 2012, which had an earlier start to its influenza season.
For a more detailed report on respiratory activity in NSW see: http://www.health.nsw.gov.au/PublicHealth/Infectious/influenza_reports.asp.
Legionellosis
There were 17 cases of legionellosis due to Legionella pneumophila strains notified in the second quarter of 2013, similar to the number notified in the same period in 2012 (n = 18). There were no links between cases identified, and no likely environmental sources were found. There were also eight cases of legionellosis due to L. longbeachae strains, similar to the same period in 2012 (n = 9).
Vaccine-preventable diseases
Meningococcal disease
Six cases of meningococcal disease were notified in NSW in the second quarter of 2013 (three in April, one in May and two in June), a marked reduction from the 22 notified in the same period in 2012. The age of the cases ranged from 1 to 58 years, with four cases aged less than 5 years. Of the six notifications, five (83%) were due to serogroup B (for which there is no vaccine), and one was not able to be typed.
Immunisation against meningococcal C disease is recommended for all children at the age of 12 months, as well as people at high risk of disease.
Measles
There were nine measles notifications in NSW in the second quarter of 2013, a decline from the 22 reported in the same period in 2012. Cases ranged in age from 1 to 35 years. Five of the cases acquired the infection overseas (from either India, Thailand, Europe or Bali). Two further cases acquired the infection from close contacts of one of the cases returning from Thailand. The remaining two cases acquired the infection locally, however links to known cases were not identified.
Two doses of measles-containing vaccine are recommended for all children at 12 and 18 months age. All young adults planning international travel should ensure they are up to date with their measles vaccinations before they travel.
Pertussis
There were 504 pertussis cases notified in NSW during the second quarter of 2013. This is approximately one-third of the 1385 notifications for the same period in 2012 and represents the lowest number of notifications for a second quarter since the statewide epidemic in 2008. Most cases were in the 0–4 and 5–9-year age groups (n = 109 each), followed by the 10–14-year age group (n = 69).
Direct protection for young infants remains available through free vaccination for pertussis that is administered at 2, 4 and 6 months of age. The first dose can be provided as early as 6 weeks of age with a booster dose at 3½ to 4 years. Whooping cough vaccination is strongly recommended for adults in contact with young babies too young to be vaccinated. Women planning a pregnancy or in their third trimester should receive a whooping cough vaccine on prescription to protect their very young babies.
Sexually transmissible infections and bloodborne viruses
Chlamydia
There were 5089 cases of chlamydia notified in NSW during the second quarter of 2013. This number is 5% lower than the number notified in the first quarter (n = 5339), and similar to the second quarter of 2012 (n = 5137). Thirty-seven percent of the cases in the second quarter of 2013 were young women aged 15–24 years (n = 1875).
Gonorrhoea
There were 1044 cases of gonorrhoea notified during the second quarter of 2013, which is 5% lower than the number notified in the first quarter (n = 1101), and similar to the second quarter of 2012 (n = 1026). Of the 1044 cases, almost half were men aged between 20 and 34 years (n = 508).
Syphilis
There were 246 syphilis notifications in the second quarter of 2013, an increase of 23% from the same period last year (n = 200). Of the 246 syphilis notifications for this quarter, 138 (56%) notifications were classified as infectious syphilis. Thirty-seven percent of the cases in the second quarter of 2013 were men aged between 30 and 44 years (n = 92).
Lymphogranuloma venereum (LGV)
There were 10 cases of LGV in the second quarter of 2013. Although this is much higher than the number notified in the second quarter of 2012 (n = 2), it is the same as the average for the same period over the previous 3 years (n = 10). All cases in the second quarter of 2013 were men aged between 25 and 44 years.
HIV
There were 101 cases of newly diagnosed HIV infection notified in NSW residents during the second quarter of 2013, an increase from the same period in 2012 (n = 84) and from the average for the same period over the previous 4 years (n = 82). Similar to previous years, 80% of infections were reported to be homosexually acquired and 13% were heterosexually acquired (in people not from high HIV prevalence countries). The highest number of notifications was amongst people aged 20–29 years.
In the first half of 2013, more than one-third (39%) of the notifications were reported as recent HIV infection at time of diagnosis (defined as either a negative or indeterminate HIV antibody test or seroconversion illness in the previous 12 months), while 13% were advanced infections (AIDS and/or CD4<200 cells/µL). Of the 179 cases notified, 36% commenced treatment soon after diagnosis.
A summary of HIV notification data for the second quarter of 2013 is available at: http://www.health.nsw.gov.au/endinghiv/Documents/hiv-in-nsw-2nd-quarter-report-2013.pdf
Arboviral infections
Ross River virus
There were 197 cases of Ross River virus infection notified in the second quarter of 2013, a decrease compared with the same period in 2012 (n = 218). Ross River virus notifications were again highest in coastal regions, particularly along the north coast of NSW.
Barmah Forest virus
There were 133 cases of Barmah Forest virus infection notified in NSW in the second quarter of 2013, an increase compared with the same period in 2012 (n = 80). However, there continue to be concerns about false-positive laboratory reports for Barmah Forest Virus and so the figures for 2013 should be interpreted with caution.
Dengue virus
There were 70 cases of dengue virus infection notified in NSW in the second quarter of 2013, similar to the same period in 2012 (n = 72). All cases in the second quarter of 2013 were overseas-acquired infections, with 50% of all cases believed to have acquired dengue virus infection in Indonesia, followed by Thailand (19% of notified cases).
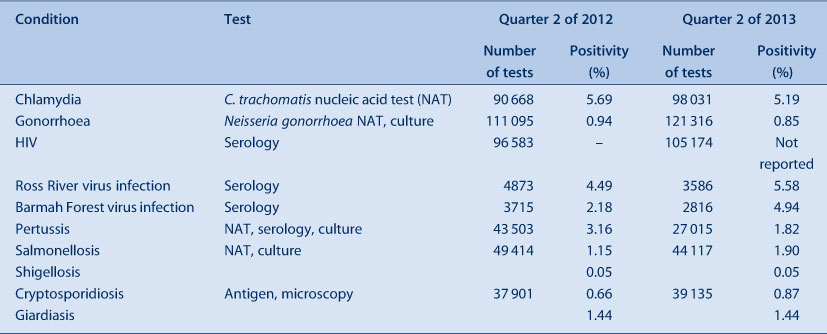
NSW Denominator Data Project
Notifications of positive laboratory results for notifiable conditions provide information about the number of new cases of disease. Data on the level of testing is useful to indicate whether an apparent increase in notification may be due to increased testing.
The NSW Denominator Data Project commenced in January 2012 to collect the total number of tests performed per month (the denominator data) for 10 selected notifiable conditions for which the testing rate might impact the notification rate. Data provided each month from 14 public and private laboratories in NSW are collated to give monthly aggregated data per condition. No demographic information is provided.
The positivity rate for the second quarter of 2013 ranged from 0.05% (shigellosis) to 5.6% (Ross River virus) (Table 1). Overall, the postivity rates were similar for the second quarter in 2013 as for the same period in 2012 – with the exception of Barmah Forest virus (up to 4.9% from 2.2% in 2012) and pertussis (down to 1.8% from 3.2% in 2012). Notifications for chlamydia and gonorrhoea were correlated with testing, while incidence of enteric conditions suggests that seasonal factors rather than testing patterns influence notification rates.
|
|