3. Methods
NSW Public Health Bulletin 21(1) 11-15 https://doi.org/10.1071/NB10S03
Published: 24 June 2010
Data sources
The NSW Midwives Data Collection
The NSW Midwives Data Collection (MDC) is a population-based surveillance system covering all births in NSW public and private hospitals, as well as home births. It encompasses all live births, and stillbirths of at least 20 weeks gestation or at least 400 g birth weight.
The MDC relies on the attending midwife or doctor to complete a notification form when a birth occurs. The form, a copy of which is shown in Appendix 4, includes demographical items and items on maternal health, the pregnancy, labour, birth and perinatal outcomes. Completed forms are sent to the Data Collections and Reporting Unit in the Demand and Performance Evaluation Branch of the NSW Department of Health, where they are compiled into the MDC database.
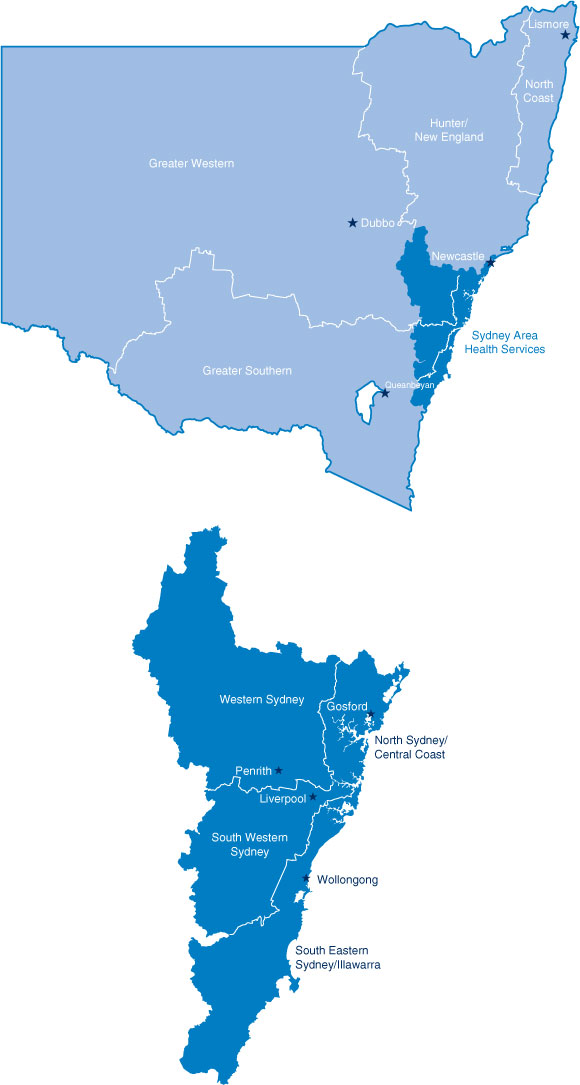
Sixty-nine percent of MDC notifications are received electronically from hospital obstetric information systems. These notifications are received by disk or email and replace the submission of the record on paper. There are several source systems that generate the MDC data. The largest source is the ObstetriX database, which supplies 41.2% of all MDC records and covers Northern Sydney and Central Coast Area Health Service, South Eastern Sydney and Illawarra Area Health Service, Sydney West Area Health Service, and some hospitals in Hunter and New England Area Health Service. The following systems also supply records to the MDC: Cerner (Sydney South West Area Health Service), 18.1%; Meditech, which supplies data for three Ramsay Private Hospitals (North Shore Private Hospital, Westmead Private Hospital and St George Private Hospital), 6.1%; Sydney Adventist Hospital database, 2.3%; and Newcastle Private Hospital database, 2.0%. A map of NSW health areas is shown in Figure A.
|
The MDC receives notifications of women whose usual place of residence is outside NSW but who give birth in NSW. However, the MDC does not receive notifications of births outside NSW to women usually resident in NSW.
The NSW Register of Congenital Conditions
The NSW Register of Congenital Conditions, formerly known as the Birth Defects Register, is a population-based surveillance system established to monitor congenital conditions detected during pregnancy or at birth, or diagnosed in infants up to 1 year of age. The Register was established in 1990 and, under the NSW Public Health Act 1991, from 1 January 1998, doctors, hospitals and laboratories have been required to notify congenital conditions detected during pregnancy, at birth, or up to 1 year of life. The Register is administered by the Centre for Epidemiology and Research of the NSW Department of Health.
There are three types of conditions that are reported to the Register:
-
Conditions that affect the growth, development and health of the baby and that are present before birth, such as cleft lip, dislocated hip and problems with the development of the heart, lungs or other organs
-
Conditions due to changes in the number of the baby’s chromosomes, such as Down Syndrome
-
Four conditions due to changes in the baby’s inherited genetic information: cystic fibrosis, phenylketonuria, congenital hypothyroidism and thalassaemia major.
The activities of the Register include the following: annual publication of information on congenital conditions in NSW; provision of information to area health services to assist in service planning and monitoring of child health, and investigation of specific issues; provision of information in response to specific requests from the public, health professionals, and other government departments; and provision of data to the Australian Institute of Health and Welfare (AIHW) National Perinatal Statistics Unit (NPSU) for monitoring of congenital conditions at a national level, and incorporation into the NPSU’s Congenital Anomalies in Australia Reports. The NPSU is also responsible for providing Australian information on congenital conditions to the International Clearinghouse for Birth Defects Monitoring Systems, a non-governmental organisation of the World Health Organization.
Sources of notifications to the Register include the MDC, specialist paediatric hospitals, cytogenetic laboratories and individual health-care providers. The Register is supported by an advisory committee, comprising a panel of clinical experts representing the following specialities: genetics, dysmorphology, neonatology, obstetrics and gynaecology, midwifery, bioethics and epidemiology; and a community representative from the Association of Genetic Support of Australasia.
Data for research purposes may be provided in the following two formats: aggregate information similar to that contained in this report, and data concerning individuals with identifying information removed. All requests for data should be submitted in writing to the Director, Centre for Epidemiology and Research. Requests for data concerning individuals for sufficiently important research purposes will be referred to the NSW Population and Health Services Research Ethics Committee. Procedures for release of personal information are described in the Department’s Policy Directive PD2006-077 Data Collections – Disclosure of unit record data held for research or management of health services which is available on the NSW Department of Health’s website at www.health.nsw.gov.au.
The NSW Admitted Patient Data Collection
For this report, data from the NSW Admitted Patient Data Collection (APDC) for public and private hospitals in NSW were linked to MDC data to produce information on postnatal length of stay in NSW hospitals, and mother’s health insurance status. Approval for the linkage was obtained from the NSW Population and Health Services Research Ethics Committee. Record linkage was carried out by the Centre for Health Record Linkage (www.cherel.org.au).
The APDC covers demographic and episode-related data for every inpatient that is separated from any public, private and repatriation hospital, private day-procedure centre, or public nursing home in NSW. Separation can result from discharge, transfer, death or change in service category. The APDC is maintained by the Data Collections and Reporting Unit in the Demand and Performance Evaluation Branch of the NSW Department of Health.
NSW Maternal and Perinatal Committee
The NSW Maternal and Perinatal Committee is a quality-assurance committee established under the NSW Health Administration Act 1982, and is privileged under the Act to carry out confidential reviews of both maternal and perinatal deaths. Members are appointed by the Minister for Health.
The Committee reviews each maternal death to identify any possible avoidable factors and to determine whether the death was related to pregnancy (or its management) or whether it was incidental. The Committee also reviews perinatal deaths among live-born babies, and stillbirths of at least 20 weeks gestation or at least 400 g birth weight. The information obtained from these reviews assists in the development of policies aimed at improving the health of mothers and newborns in NSW. Information considered by the Committee is confidential.
Method for estimating level of reporting of maternal Aboriginality
The Aboriginality of the mother, rather than the baby, is reported to the MDC, although mother’s Aboriginality is frequently used as a proxy measure for the baby’s Aboriginality. Maternal Aboriginality was used for this analysis. The number of births reported to Torres Strait Islander mothers is quite small in NSW. Aboriginal and Torres Straight Islander mothers were therefore combined for this analysis. For ease of reference, ‘Aboriginal’ is used to refer to both Aboriginal and Torres Strait Islander mothers.
Records of births reported to the MDC were linked to birth registration records of the NSW Registry of Births, Deaths and Marriages for births occurring in the 3-year period 2004–2006. Record linkage was carried out at the Centre for Health Record Linkage (www.cherel.org.au). The overall linkage rate was 93.9% of MDC records and 98.5% of birth registration records.
Capture–recapture methods are used to adjust estimates of counts to reflect ascertainment level or undercounting. Capture–recapture was carried out using the method described by McCarty et al.1 Analysis was carried out using SAS version 9.1.3. Analyses concerning geographical location were based on health area of residence as reported to the MDC.
Definitions
Aboriginal or Torres Strait Islander
Women who identify themselves to be of Australian Aboriginal or Torres Strait Islander heritage.
Apgar score
A numerical scoring system routinely administered 1 and 5 min after birth to evaluate the condition of the baby. The score ranges from 0 to 10 (10 being perfect). It takes account of the following five physical signs, each of which is assigned a component score of 0, 1 or 2: heart rate, respiration, muscle tone, reflexes and colour.
Augmentation
Artificial rupture of the membranes or use of oxytocic drugs after spontaneous onset of labour.
Birth weight
The newborn infant’s first bare weight in grams. Low birth weight: birth weight less than 2500 g. Very low birth weight: birth weight less than 1500 g. Extremely low birth weight: birth weight less than 1000 g.
Caesarean section
Birth of the fetus through an abdominal incision. Elective caesarean section: a caesarean section (planned or unplanned) performed before the onset of labour. Emergency caesarean section: a caesarean section performed after the onset of labour, whether or not the onset of labour was spontaneous.
Confinement
Refers to a woman having given birth. In a multiple pregnancy, one confinement will result in more than one birth.
Epidural
Injection of analgesic agent outside the dura mater which covers the spinal canal; includes lumbar, spinal and epidural anaesthetics.
Episiotomy
An incision of the perineum and vagina to enlarge the vulval orifice.
Gestational age
The duration of pregnancy in completed weeks from the first day of the last normal menstrual period. Where accurate information on the date of the last menstrual period is not available, a clinical estimate of gestational age may be obtained from ultrasound during the first half of pregnancy or by examination of the newborn infant. The ‘best estimate’ is used in this report.
Induction of labour
Oxytocics–prostaglandins: the initiation of labour by the use of oxytocic agents, prostaglandins, or their derivatives (oral, intravaginal or intravenous).
ARM only: the initiation of labour by artificial rupture of membranes.
Oxytocics–prostaglandins and ARM: both medical and surgical induction as defined above (combined medical and surgical induction).
Live birth
The complete expulsion or extraction from its mother of a baby of at least 400 g or 20 weeks gestation who, after being born, breathes or shows any evidence of life such as a heartbeat.
Neonatal death
The death of a live-born infant within 28 days of birth.
Neonatal mortality rate
The number of neonatal deaths per 1000 live births.
Parity
The total number of live births and stillbirths of the mother before the pregnancy or birth under consideration.
Perinatal death
A stillbirth or neonatal death.
Perinatal mortality rate
The number of perinatal deaths (stillbirths and neonatal deaths) per 1000 total births in a year (live births and stillbirths combined).
Perineal status
1st degree tear: a perineal graze–laceration–tear involving: the fourchette, hymen, labia, skin, vagina, or vulva.
2nd degree tear: a perineal laceration or tear involving the pelvic floor or perineal muscles or vaginal muscles.
3rd degree tear: a perineal laceration–tear involving the anal sphincter or rectovaginal septum.
4th degree tear: a third degree perineal laceration or tear which also involves the anal mucosa or rectal mucosa.
Plurality
The number of fetuses or babies from the pregnancy. On this basis, pregnancy may be classified as single or multiple.
Premature infant
An infant born before 37 completed weeks gestation.
Spontaneous abortion
The spontaneous expulsion of a fetus of less than 20 weeks gestation and less than 400 g birth weight.
Stillbirth
The complete expulsion or extraction from its mother of a product of conception of at least 20 weeks gestation or 400 g birth weight who did not, at any time after birth, breathe, or show any evidence of life such as a heartbeat.
Termination of pregnancy
A procedure intentionally performed to terminate a pregnancy before 20 completed weeks gestation.
Explanatory notes
Breastfeeding
From 2007, the MDC has collected information on infant feeding at the time of discharge from hospital (or discharge from care for home births) for all infants born in NSW. Infant feeding is reported via the following three tick-box categories: breastfeeding, expressed breastmilk and infant formula. More than one type of feeding may be reported by ticking multiple boxes. In this report, infant feeding is classified into the following three categories: full breastfeeding, which includes babies who were reported to be breastfed or to be receiving expressed breast milk and no infant formula; any breastfeeding, which includes babies who were reported to be receiving breast milk and infant formula; and no breastfeeding.
Rates of congenital conditions
The Register of Congenital Conditions collects data pertaining to congenital conditions, regardless of the outcome of pregnancy. This includes notifications of live births, stillbirths, terminations of pregnancy and spontaneous abortions. Rates are calculated using births (that is, live births and stillbirths) as the denominator, because denominator populations for pregnancies of less than 20 weeks gestation are unknown. The numerators are described in the relevant sections.
The source of denominator population data on births is the MDC. The MDC was selected because its definitions are consistent with those applied by the Register of Congenital Conditions.
Differences in rates of conditions published by the Register of Congenital Conditions compared with interstate registers may be due to differences in coding practices, in categories of conditions included in each register and differences in the upper age limit for notification of cases.
Place of residence of mother
The mother’s usual residence was the basis for coding to statistical local areas and NSW health areas.
Labour
The category labour – spontaneous with oxytocics–prostaglandins was used where labour was augmented with artificial rupture of membranes as well as oxytocics or prostaglandins.
Level of obstetric hospitals
Level 1: local maternity service (no births); postnatal, only for women with normal outcomes.
Level 2: small maternity services; normal-risk pregnancy and births only. Staffed by general practitioners and midwives.
Level 3: country district and smaller metropolitan services; care for mothers and infants at normal–selected moderate-risk pregnancies and births. Full resuscitation and theatre facilities available. Rostered obstetricians, resident medical staff and midwives. Accredited general practitioners and specialist anaesthetist on call. Has Level 2b neonatal care.
Level 4: regional referral–metropolitan district services; birth and care for mothers and/or babies with moderate risk factors. Obstetricians and paediatrician available 24 hours a day, 7 days a week. Rostered resident medical staff, specialist anaesthetist on call. Has Level 2b neonatal care.
Level 5: regional referral–metropolitan services; care for mothers and infants known to be at high risk. Able to cope with complications arising from these risk factors. Has Level 2a neonatal care.
Level 6: (tertiary)–specialist obstetric services (supra regional). All functions – normal, moderate and high-risk births. Has Level 3 neonatal intensive care.
Type of birth
The ‘vaginal breech’ category covers all forms of vaginal breech birth, including forceps to the after-coming head.
Perinatal mortality rate
Perinatal deaths include deaths reported to the MDC only. As the MDC form is completed at discharge or transfer of the baby, deaths occurring after this time may not be reported to the MDC. Birth and perinatal-death registration data held by the Australian Bureau of Statistics (ABS) give the most complete ascertainment of perinatal deaths for calculation of rates.
[1] McCarty DJ, Tull ES, Moy CS, Kwoh CK, LaPorte RE. Ascertainment corrected rates: applications of capture–recapture methods. Int J Epidemiol 1993; 22(3): 559–565.
| Crossref | GoogleScholarGoogle Scholar |



