Pandemic (H1N1) 2009 influenza in NSW
Sarah V. Thackway A and Jeremy M. McAnulty B CA Centre for Epidemiology and Research, NSW Department of Health
B Communicable Diseases Branch, NSW Department of Health
C Corresponding author. Email: jmcan@doh.health.nsw.gov.au
NSW Public Health Bulletin 21(2) 1-3 https://doi.org/10.1071/NB10001
Published: 8 April 2010
In 2009, New South Wales (NSW) Health launched its most intensive public health surveillance, investigation and containment effort in living memory. This unprecedented effort was in response to something that had been planned for and feared for many years: an outbreak of a new strain of influenza to which the world’s population had no immunity, with the potential to cause disease, death and disruption on a massive scale.
NSW Health, along with other Australian health authorities and government agencies, had been preparing, with renewed earnest, for such a pandemic since the SARS outbreak of 2002–03. That outbreak had highlighted the potential immense health, social and economic consequences that an emerging infectious disease can cause within a country. Among the plans developed to manage a pandemic were the national plan, Australian Health Management Plan for Pandemic Human Influenza,1 and the NSW plans, the NSW Health Interim Influenza Pandemic Action Plan, 20052 and the New South Wales Human Influenza Pandemic Plan, 2006.3 Several national and state-wide exercises had been held to test and improve these plans and had strengthened the interactions among the various agencies involved in their delivery.4,5
Following initial reports of a deadly outbreak of a novel form of influenza in Mexico, and linked cases in the United States of America in April 2009,6 the World Health Organization issued warnings that a pandemic was likely.7 Nations around the world began to prepare for the inevitable spread of the virus.
The three phases of response
In late April 2009, on the same weekend that the initial reports emerged of outbreaks spreading to North America, Australian health authorities began activating their pandemic plans which include discrete phases of response (aligned with the WHO pandemic phases). The initial phase, the DELAY phase, was initiated in an attempt to delay the novel virus entering Australia. Multiple urgent teleconferences refined the surveillance, preparedness and response procedures. Communiqués were issued to health workers and the media about the known risk and what precautions to take, public health emergency operation centres were activated across the country and public health units moved to high alert. A surge capacity workforce was identified and prepared.
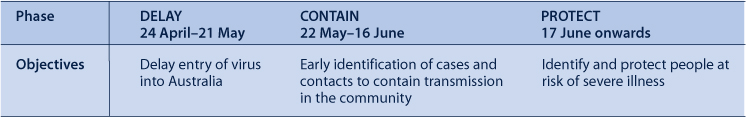
By May 2009 the first cases of H1N1 influenza started to be reported in NSW. On the 22 May as the virus began to spread within the community, NSW Health moved to the CONTAIN phase of a pandemic, where the focus was directed towards early identification of cases and contacts in an attempt to limit transmission in the community. By the 17 June, community-wide transmission of the virus was reported and NSW moved to the PROTECT phase that concentrated resources on identifying and protecting people at risk of severe illness. Table 1 summarises the three phases of pandemic preparations in NSW in 2009.
|
Measuring the affect of the pandemic in NSW
By the time the pandemic eased at the end of August 2009, 1214 people with pandemic (H1N1) 2009 infection had been hospitalised (17.2 per 100 000 population), 225 had been admitted to intensive care (3.2 per 100 000), and 48 had died (0.7 per 100 000). The pandemic affected children aged 0–4 years and adults aged 50–54 years the most; with the highest hospitalisation rates and the highest rates of intensive care admission in these age groups respectively.
The NSW hospital system was hit hard with overall presentations to emergency departments being 6% higher than the previous year, and presentations for influenza-like illness 736% higher. In response, NSW hospitals opened 1300 influenza clinics, an average of 20 each day. By the end of August, these clinics had triaged 9307 people, an average of 145 people a day, and dispensed 2226 courses of antiviral medications.
During this time large numbers of tests for respiratory viruses were performed at NSW public laboratories. At the peak of the pandemic 10% of these tests were positive for influenza A and 82% of those were positive for pandemic (H1N1) 2009 influenza.
Some people experienced severe respiratory symptoms with 225 people admitted to intensive care units in NSW. At the peak of the pandemic in late July suspected cases and confirmed cases of pandemic (H1N1) 2009 influenza accounted for 32% of the available intensive care unit bed capacity in NSW. An unexpectedly high number of people (30, 16% of intensive care unit admissions) required extra corporeal membrane oxygenation (ECMO) therapy. This treatment is viewed as a last resort therapy when critically ill patients are no longer responding to conventional ventilation support. NSW was able to respond to the sudden and increased requirement for ECMO having launched in May 2009 the NSW ECMO Medical Retrieval Service. This program provides a tertiary referral service that sends clinical teams to the referring hospital to stabilise a patient on ECMO before the patient is transferred to a tertiary centre for care.
However despite the surge in emergency department presentations and intensive care unit admissions, available data suggest that the overall mortality from influenza and pneumonia in 2009 was similar to recent influenza seasons. The majority of people who died had underlying chronic conditions. This pattern of mortality requires further exploration.
This special issue on pandemic H1N1 (2009) influenza
The articles contained in this special issue of the Bulletin describe how NSW was affected by the pandemic and how the public health services responded to the challenge. Spokes et al. describe the incident control system initiated by NSW Department of Health and how public health actions changed as the pandemic moved through the three response phases. Binns et al. describe how public health units responded, in particular during the DELAY and CONTAIN phases, to limit the widespread community transmission of the virus. This experience is illustrated by a number of case studies including the surge capacity required to manage the passengers and crew of a large cruise ship on which cases were identified. Weston and Truman illustrate the extent and speed of the public health response through a case study of a clinic that was established in a primary school after a case was identified. Churches et al. examine the fundamental role that surveillance plays during public health emergencies, like the pandemic, to inform decision making. The objectives of surveillance varied for each phase of the response and consequently various sources and types of surveillance information were required reflecting the need for surveillance systems to be flexible to allow for rapid modification when needed. Adamson et al. provide an overview of the public health laboratory response during the pandemic and reflect on the contribution of a co-ordinated, online specimen tracking and results reporting system. Totaro provides insight into how the some of the sickest patients were managed by intensive care units, including the use of ECMO. Rudge and Massey discuss working with Aboriginal communities to face the threats posed by influenza. Fizzell et al. outline the implementation of the pandemic (H1N1) 2009 influenza vaccination program in NSW. To sum up the NSW experience, Booy and Dwyer provide a personal commentary on the pandemic and reflect on lessons learned from the past.
These authors provide valuable insights into the NSW response and the lessons learned that will guide the future management of influenza, and in particular pandemic influenza. The 2009 pandemic and our response to it placed the health system under strain, because of the extent of resources required even for a mild form of influenza. The strong networks and sharing of resources within the health system enabled a more efficient response. Such networks should continue to be strengthened in NSW, Australia and internationally.
Through these authors, the NSW Public Health Network, their colleagues in clinical operations and critical care, laboratory staff, scientists and practitioners, we have gained evidence and invaluable insights into how to enhance our response to influenza, yet much remains unknown. We know pandemic (H1N1) 2009 influenza will return to NSW, almost certainly by next winter, but we do not know exactly when; we know the 2009 influenza season was associated with high levels of morbidity but we do not know the scale of the impact in 2010; we know we have the methods to prevent infection through immunisation and infection control but we do not know how to ensure compliance by the population. While we seek to answer these and many other questions, we need to incorporate the evidence we have already gathered into our planning and preparedness for the next pandemic.
[1]
[2]
[3]
[4] Craig AT, Armstrong PK. Exercise Paton: a simulation exercise to test New South Wales emergency departments’ response to pandemic influenza. CDI 2007; 31(3): 310–3.
| PubMed | (Accessed 9 December 2009.)
[7]

