Evaluation of the NSW Management Policy to Reduce Fall Injury Among Older People, 2003–2007: implications for policy development
Wendy L. Watson A C and Rebecca J. Mitchell A BA NSW Injury Risk Management Research Centre, The University of New South Wales
B Department of Aviation, The University of New South Wales
C Corresponding author. Email: w.watson@unsw.edu.au
NSW Public Health Bulletin 22(4) 69-72 https://doi.org/10.1071/NB10003
Published: 2 June 2011
Abstract
Aim: To retrospectively evaluate the NSW Management Policy to Reduce Fall Injury Among Older People, 2003–2007. Methods: The process evaluation was conducted by interviewing stakeholders regarding the implementation of the Policy. A document review was also undertaken to identify activities and initiatives undertaken during the implementation process. Results: Key achievements in the implementation of the Policy and significant early events, decisions and contextual factors which acted as barriers to the implementation were identified. Results included the: identification of the need for the prioritisation of evidence-based interventions; application of consistent best practice guidelines for implementing falls prevention strategies in the community; and development of an evaluation and monitoring framework concurrent with the development of policy. Conclusion: Subsequent policy initiatives must be strategically focused and coordinated if future activities are to have a significant impact on the increasing burden of fall-related injury.
The NSW Management Policy to Reduce Fall Injury Among Older People, 2003–20071 (the Policy) was developed to address the increasing burden of fall-related injury on the New South Wales (NSW) health system. The launch of the Policy by NSW Health in 2004 gave priority to the prevention of falls across all settings (i.e. community residents, acute care and residential aged care) in NSW. NSW Health committed $8.5 million to fund the implementation of the Policy during the 2003–2007 period. The Policy was developed following extensive consultation across the health sector, including consultation with non-government organisations.
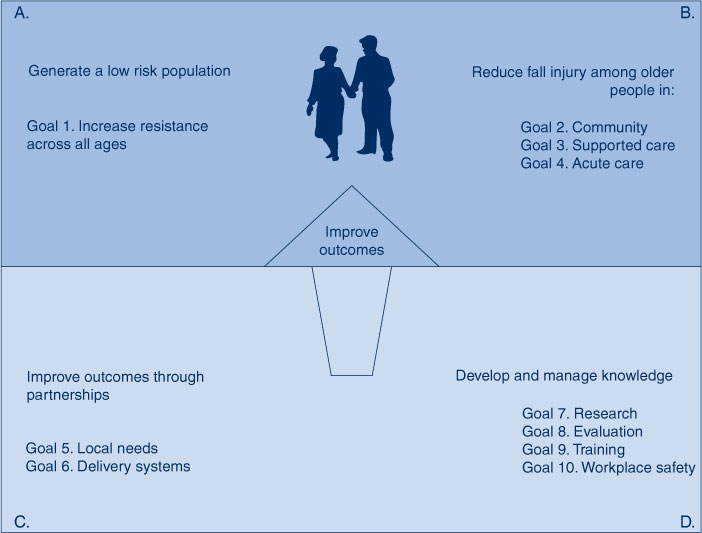
The Policy focused on developing a comprehensive, long-term approach to fall-related injury reduction by addressing the risk to older persons both before and when they are at their greatest risk, as well as in the major settings in which they spend their time. The key areas and goals of the Policy are shown in Figure 1. The Policy formed part of Healthy People 2005,2 a NSW Department of Health public health initiative, as well as the NSW Chronic Disease Prevention Strategy.3 While essentially a health policy, it also identifies roles for other sectors and organisations in reducing the risk of falls and fall-related injuries in the older population.
A number of positions were created under the umbrella of the NSW Falls Prevention Program to support the implementation of the Policy across the state. These included: a State Leader, based at the Clinical Excellence Commission, to coordinate the implementation of the Policy at a statewide level; and Area Falls Prevention Coordinators, appointed in each of the eight former NSW area health services (AHSs), to assist in area-wide planning and implementation.
The aim of this evaluation was to provide information describing the successes and challenges of the implementation phase of the Policy, including: an overview of progress on the implementation of the Policy; identification of any gaps in progress; and information to inform future policy directions. This paper describes the process evaluation of the Policy implementation.
Methods
Views of key informants and other stakeholders were obtained on: the implementation of the Policy; barriers and challenges to progress; and the ways that structures and processes created in response to the Policy might be altered to enhance its impact and influence.
Information for the process evaluation was obtained from key informant interviews. These were conducted face-to-face with each AHS Area Falls Prevention Coordinator and, where possible, their manager; senior and middle-level staff in the NSW Department of Health’s Centre for Health Advancement; and the state leader of the NSW Falls Prevention Program. Other informants including AHS health promotion managers and other stakeholders in the AHSs completed by email a self-administered version of the key informant interview. Information about activities and initiatives was obtained from a document review of meeting notes and progress reports produced at both the AHS and state level.
Results
A total of 24 of 33 invited respondents participated in the consultation (72.7% response rate). Of these interviewees, 16 (66.7%) participated in face-to-face interviews, and eight (33.3%) responded by email to the same questions in a self-administered survey. Three state-level personnel and all the Area Falls Prevention Coordinators completed face-to-face interviews, as did some of their line managers and a health promotion officer. Five of the Area Health Promotion Managers invited to participate in the survey responded to the self-administered questionnaire by email. Others who responded by email included chairs of area-level fall prevention sub-committees and a health promotion officer.
Interviews with key informants and the document review identified a number of important achievements in the implementation of the Policy. These were the:
-
recruitment of an experienced program director to the role of state falls leader and a strong, skilled team of AHS falls coordinators
-
establishment of AHS implementation plans and governance structures
-
strengthening of the NSW Falls Network through additional funding support
-
support for research to provide evidence to inform falls prevention policy and practice
-
significant progress in the implementation of falls prevention policy, guidelines and interventions in the acute care setting
-
development of innovative falls prevention programs to address the challenges created by a lack of workforce capacity
-
significant achievements in developing local policy within AHSs.
Respondents acknowledged that the Policy was large and complex to implement and that implementation could have been assisted by the development of a statewide, coordinated implementation strategy. The lack of a statewide strategy resulted in the implementation planning and development phases taking longer than expected. Respondents identified that progress with Policy implementation was also hampered due to contextual factors including:
-
organisational and leadership changes at both the AHS and state level
-
the need for a clear distinction between the roles of the Clinical Excellence Commission and the NSW Department of Health in relation to the governance of the Policy
-
the absence of prioritisation of interventions identified in the Policy for implementation in AHSs
-
a lack of standardised resources (e.g. best practice guidelines, standard screening and assessment tools) and the absence of a timetable for Policy implementation
-
the need to build new stakeholder relationships across three different settings (i.e. community, acute and residential care)
-
the absence of workforce capacity, particularly in the community setting (e.g. allied health staff and physical activity leaders) to implement prevention programs
-
a lack of evidence-based guidelines for community falls prevention.
Overall, respondents believed that in relation to the falls policy there was a strong need for:
-
executive support within AHSs for policy implementation
-
a formal support structure for area falls coordinators who were coordinating programs across several different settings
-
the development of process and impact indicators to monitor short- to medium-term implementation goals
-
identification of culturally appropriate strategies and resources for falls prevention in consultation with indigenous and culturally and linguistically diverse populations.
Discussion
There is a compelling imperative to reduce the rate of fall-related injury among older people in all settings given the rapidly ageing population. This process evaluation identified that much has been achieved during the formative phase of the implementation of the Policy in NSW. Structures, relationships and processes are now in place, at both the state and AHS level, to support future capacity building and the sustainability of many fall injury prevention programs.
The evaluation identified that progress has been made in the implementation of the Policy and in the introduction of guidelines and interventions, largely in the acute care setting. However, the great majority of injurious falls occur in the community and in residential aged care and there is a need to concentrate future falls prevention policy and activities in these settings.
While there is a need to reduce the immediate fall risk of older persons in the community, there is also a need to take a longer-term public health approach to generating a future low fall-risk population. The foundation of this proactive approach lies in the promotion and maintenance of lifelong healthy diet and exercise. A recent systematic review of the perceptions of enablers and barriers to the participation of older people in falls prevention interventions4 has shown that participation in, and adherence to, physical activity programs is more likely among those with a history of exercise.5–7 Further, the ‘habit’ of exercise was the strongest predictor of future physical activity.8
Any decisions about the composition of an optimal portfolio of evidence-based fall injury interventions for community residents should take into account the threshold of investment required to impact on the rate of fall-related injury. This decision will be assisted by research that identifies the different cost-effectiveness thresholds of falls interventions at the population level for NSW.9
In light of the findings of this evaluation, consideration needs to be given to a number of issues to inform future policy directions. These include the:
-
development of a statewide, coordinated approach to falls prevention which prioritises evidence-based interventions and includes an implementation plan and reporting milestones
-
need for consistent best practice guidelines that provide details on implementing fall injury prevention strategies in the community; the publication of national community falls prevention guidelines by the Australian Commission on Safety and Quality in Health Care10 since the completion of this evaluation study provides a solid foundation for the development of the new state falls management plan
-
need to clearly define the areas of responsibility for falls prevention across the community, acute and residential age care sectors
-
recognition of the diversity of the older population and the need for the development of population-level interventions for healthy older people, along with targeted activities to address the varying degrees of risk within frailer groups
-
clear definition of roles and responsibilities for the implementation of the falls management policy between NSW Department of Health, the Clinical Excellence Commission and AHSs
-
creation of a concurrent evaluation framework and a reporting framework that incorporates achievable performance indicators without imposing an onerous data collection load on staff
-
development of supporting, standardised resources in conjunction with future policies
-
identification of specific funding allocations for falls prevention activities at the AHS level by the NSW Department of Health and a requirement for AHSs to report annually on their own contribution to falls prevention activities in each of the three settings.
Conclusion
Although much has been achieved during the formative phase of the implementation of the NSW Management Policy to Reduce Fall Injury Among Older People, 2003–2007, subsequent policy initiatives must be strategically focused and coordinated if future activities are to have a significant impact on the increasing burden of falls injury. This study identified a number of actions that will assist future policy development in this area.
Acknowledgments
W Watson was supported by the NSW Department of Health. R Mitchell was partially supported by the NSW Department of Health and by an Australian Research Council-linkage post-doctoral fellowship (LP0990057).
The authors would like to thank all the NSW Health staff who participated in the evaluation, in particular the staff of the NSW Falls Prevention Program, at both the state and area health service levels. The members of the NSW Falls Policy Evaluation Advisory Committee are also acknowledged and thanked for their input over the course of the evaluation and for providing feedback on drafts of the evaluation report.
References
[1] NSW Department of Health. NSW Management Policy to Reduce Fall Injury Among Older People, 2003–2007. Available from: http://www.health.nsw.gov.au/policies/PD/2005/pdf/PD2005_353.pdf (Cited 13 January 2011.)[2] NSW Department of Health. Healthy People 2005: New Directions for Public Health in New South Wales. Available from: http://www.health.nsw.gov.au/pubs/2000/pdf/public2005.pdf (Cited 13 January 2011.)
[3] NSW Department of Health. NSW Chronic Disease Prevention Strategy 2003–2007. Available from: http://www.health.nsw.gov.au/pubs/2003/pdf/chronic_disease.pdf (Cited 13 January 2011.)
[4] Bunn F, Dickinson A, Barnett-Page E, McInnes E, Horton K. A systematic review of older people's perceptions of facilitators and barriers to participation in falls prevention interventions. Ageing Soc 2008; 28 449–72.
| A systematic review of older people's perceptions of facilitators and barriers to participation in falls prevention interventions.Crossref | GoogleScholarGoogle Scholar |
[5] Resnick B. A prediction model of aerobic exercise in older adults living in a continuing-care retirement community. J Aging Health 2001; 13 287–310.
| A prediction model of aerobic exercise in older adults living in a continuing-care retirement community.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DC%2BD38%2Fmt1Cgtg%3D%3D&md5=c639ae49d2c5c73d46d6e87452cfec3cCAS | 11787516PubMed |
[6] Resnick B, Spellbring AM. Understanding what motivates older adults to exercise. J Gerontol Nurs 2000; 26 34–42..
| 1:STN:280:DC%2BD3M7itVSkuw%3D%3D&md5=7cf3bbeb2e094687d3b05ce1ed13c08eCAS | 11111629PubMed |
[7] Stead M, Wimbush E, Eadie D, Teer P. A qualitative study of older people’s perceptions of ageing and exercise: the implications for exercise. Health Educ J 1997; 56 3–16.
| A qualitative study of older people’s perceptions of ageing and exercise: the implications for exercise.Crossref | GoogleScholarGoogle Scholar |
[8] Rejeski WJ, Brawley LR, Ettinger W, Morgan T, Thompson C. Compliance to exercise therapy in older particpants with knee osteoarthritis: implications for treating disability. Med Sci Sports Exerc 1997; 29 977–85.
| Compliance to exercise therapy in older particpants with knee osteoarthritis: implications for treating disability.Crossref | GoogleScholarGoogle Scholar | 1:STN:280:DyaK2svhsVSktQ%3D%3D&md5=0fafd19136b895bf6423f4826d0827cfCAS | 9268953PubMed |
[9] Church J, Goodall S, Norman R, Haas M. An economic evaluation of community and residential aged care falls prevention strategies in NSW. NSW Public Health Bull 2011; 22(3–4): 60–68
[10] Australian Commission on Safety and Quality in Health Care. Preventing Falls and Harm From Falls in Older People: Best Practice Guidelines for Australian Community Care. Commonwealth of Australia: Canberra; 2009. Available from: http://www.health.gov.au/internet/safety/publishing.nsf/Content/com-pubs_FallsGuidelines/$File/30456-Guidelines-COMM.PDF (Cited 13 January 2011.)