Improving the health of sex workers in NSW: maintaining success
Basil Donovan A B E , Christine Harcourt A , Sandra Egger C and Christopher K. Fairley DA National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales
B The Sydney Sexual Health Centre, Sydney Hospital
C Faculty of Law, The University of New South Wales
D School of Population Health, The University of Melbourne and Melbourne Sexual Health Centre, Alfred Hospital, Melbourne
E Corresponding author. Email: bdonovan@nchecr.unsw.edu.au
NSW Public Health Bulletin 21(4) 74-77 https://doi.org/10.1071/NB10013
Published: 27 May 2010
Abstract
NSW has a diverse sex industry that is limited in its size by modest demand. There is no evidence that decriminalisation in 1995 increased the frequency of commercial sex in NSW. Though the largest sector, female brothels, is now mainly staffed by Asian women, condom use for vaginal and anal sex exceeds 99% and sexually transmissible infection rates are at historic lows. These gains are attributable to the long-term support of the NSW Department of Health in collaboration with the community-based Sex Workers Outreach Project and sexual health services, facilitated by the removal of criminal sanctions without the expense and access barriers of licensing systems.
Just a generation ago sex work in New South Wales (NSW) had been criminalised for many years, linking the sex industry to criminal subcultures and fuelling corrupt behaviour.1 In Sydney, both community-based2 and clinic-based3 studies of brothel workers reported rates of sexually transmissible infections that were comparable to many resource-poor countries. And acquired immune deficiency syndrome (AIDS) was looming. This article describes how the NSW Department of Health in collaboration with the community-based Sex Workers Outreach Project and sexual health services in the area health services have worked to improve the health of sex-workers in NSW and thereby minimise the potential public health threat posed by commercial sex.
Community responses
Sex workers had begun to organise themselves from around 1981, and in 1983 they formed the first Australian Prostitutes Collective (APC). By 1986 the APC was the first community-based sex-worker organisation in Australia, and possibly the first such community-based organisation in the world, to receive government funding. This funding enabled the APC to mobilise and manage teams of volunteers to provide peer education and support services to sex workers throughout NSW for the first time.4
Though the Australian Prostitutes Collective dissolved in 1989, the NSW Department of Health recognised the highly-effective public health model that the Collective had pioneered. The Department was quick to assist the foundation of a new organisation, the Sex Workers Outreach Project (SWOP) in 1990, which is administered by the AIDS Council of NSW. As one of the few truly community-based sex worker organisations remaining in Australia, SWOP enjoys the trust of every part of the NSW sex industry and has unique access to virtually every establishment and a close working relationship with public health services.5
Policy responses
NSW took its first steps toward reform of the laws affecting sex workers in 1979 in the context of the reform of public order offences and ‘victimless’ crimes that was promised by the Wran opposition in 1976. However prostitution laws were deeply embedded into the statutes, so it was not until The Disorderly Houses (Amendment) Act in 1995 that all forms of adult sex work were effectively decriminalised.6 Remarkably, by 1997 a survey of the most vulnerable of NSW sex workers, drug-affected street workers, found an uncomfortable relationship between the workers and police but no evidence of corruption.7
Decriminalisation of sex work enabled NSW to become a global leader in other policy areas, including the first published work-place standards for brothels8 and accreditation of the formal training of peer educators toward a diploma in community education.
In response to HIV/AIDS, direct intervention by the then Commonwealth Health Minister, Dr Neal Blewett, resulted in sex workers’ screening consultations for sexually transmissible infections (but not the pathology testing) being rebated by Medicare after 1985. Because they were usually anonymous, HIV tests were free of charge. As sex workers’ main risk of other sexually transmissible infections now stems from their non-commercial sexual behaviour,9 Medicare’s persistent policy of not rebating testing for sexually transmissible infections for this group is questionable. In practice the policy is rarely enforced and about half of Sydney female brothel-based sex workers access the private sector for testing for sexually transmissible infections.
With the removal of the criminal laws, brothels effectively became subject to planning laws that are administered by local governments. This remains a problem in NSW as many local politicians believe that their constituents want them to refuse development applications for brothels. Moreover, local governments have not been provided with any resources to administer brothels to ensure that proper occupational health and safety standards are being met. In a recent survey of local councils in Sydney development applications were not being approved at a rate sufficient to keep up with demand.
Health service responses
From the beginning of the 1990s, NSW Health adopted a policy that every area health service in the state should provide a free and confidential specialist sexual health service, and sex workers were among the key populations that were to be targeted. Within sexual health services sex workers receive periodic testing for sexually transmissible infections (depending on their individual level of risk), hepatitis vaccination, and culture-specific health education including instruction in the use of condoms and strategies for negotiating with clients that are reluctant to use condoms. In addition, the advent of Medicare in 1984 enabled the general population to access general practitioners for sexually transmissible infection testing and care: this greatly relieved the clinical burden and enabled sexual health services to move toward a proactive population health approach with an emphasis on health education.
Challenges
Injecting drug use
A majority of street-based sex workers and a minority of indoor sex workers in NSW report injecting illicit drugs.7 Due to the sustained success of the NSW harm reduction policy around drug use (see article by Wodak and Maher in this issue), sex workers have been largely spared exposure to HIV through contaminated injecting equipment, eliminating them as a potential ‘bridging’ population for HIV transmission between drug users and the general population.10 SWOP, sexual health services, and the Kirketon Road Centre, Sydney, have been active participants in the needle and syringe program from the outset.
Asian migrant sex workers
From the late 1980s, Sydney brothels witnessed a substantial influx of women from east and south-east Asian countries. Many were indebted to agents, few were competent in English, most were unable to consistently require their clients to use condoms, and the prevalence of sexually transmissible infections was unacceptably high. As most were from Thailand, they were also beginning to present with HIV infection.11
In response, the NSW Department of Health provided funding and an alliance between the Department, the Sydney Sexual Health Centre and SWOP developed the Multicultural Health Promotion Program that was launched in 1991. The Program employed staff that was proficient in Thai and, later, Mandarin and Korean. Educational resources, including videos and instructive comic books in appropriate languages, were distributed on outreach to Asian brothels and in clinics. Well-attended Asian language clinics were established in several sexual health services around Sydney, with a focus on health education.11
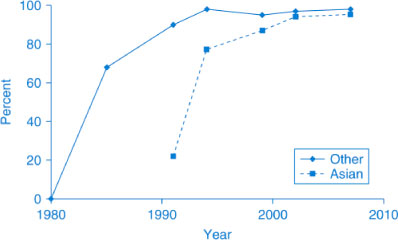
The Multicultural Health Promotion Program has been successful. Condom use by the Asian women is now similar to resident sex workers (Figure 1) and the prevalence of sexually transmissible infections is at an historic low; for example, the incidence of gonorrhoea has fallen from 440 per 100 woman years in 1980–19812 to 0.24 per 100 woman years in 2004–200612 among brothel-based workers in Sydney. Less than 1% of these women arrive with HIV infection and to date there are no documented cases of HIV transmission to or from these women resulting from their work in Australia.10
|
As Asian women now constitute the majority of the women working in Sydney’s brothels13 the Program remains important. Over time, at presentation to a clinic, this group of women has been older, better educated and more proficient in English, and they are increasingly working in Australia with legitimate student visas or resident status. Few have worked as sex workers before they came to Australia. Long ago these women effectively displaced the market for the higher-risk ‘trafficked’ women of the 1990s, and they are more in control of their working lives.14
Male sex workers
Surveillance of male sex workers is more difficult. They are a smaller part of the sex industry and rely more on electronic communication with clients (mobile phones and the internet) that has replaced conventional worksites (brothels) (anecdotal evidence suggests that the female sex industry is developing in a similar way). In a community-based cohort of gay men in Sydney, one in five men reported having been paid for sex at some time and, for one in 20 of these men, this had occurred in the previous six months. However, for more than half the men, this had only been on one or two occasions.15 Although condom use by clients of male sex workers was high, male sex workers were more likely to practise unsafe sex with non-paying partners and more likely to use illicit drugs than female brothel workers and non-sex-working homosexual men. In a clinical setting in Sydney, male sex workers were less likely to be HIV positive and more likely to report sex with women than non-sex-working men who have sex with men.16 The vulnerability of male sex workers to sexually transmissible infections and HIV (and their potential for onward transmission) appeared to be more related to their non-commercial sex or injecting behaviours than their paid sexual behaviour.15,16
Transgender sex workers
Six of 48 (12.5%) street-based sex workers in a NSW state-wide survey were transgendered; most of these street workers were working in inner Sydney. While transgender street workers were somewhat less likely to be drug dependent than their female counterparts they had fewer alternative employment options.7 Outreach health promotion officers also report occasional transgender workers in female brothels. As almost half of transgendered people have a history of sex work resulting from limited employment alternatives,17 services dealing with this population are experienced in dealing with this issue. From the outset, SWOP has addressed the special issues raised by male and transgendered sex work that typically extend beyond immediate STI/HIV risk.
Clients of sex workers
Australian men are among the least frequent consumers of commercial sexual services in the world. In a large representative national survey in 2001–2002, 2.3% of NSW men reported paying for sex in the last year, similar to the national average,18 and less than half the rate reported by New Zealand men before that country decriminalised sex work.19 Such a low proportion means that commercial sex would be unlikely to sustain a widespread heterosexual HIV epidemic in Australia and that decriminalisation has not resulted in an increase in the incidence of sex work. Clinic-based and population-based studies determined that the male clients of female sex workers reported more sexual partners than other men and they were more likely to report having injected drugs.18,20
Conclusion
NSW maintains highly effective programs that have minimised the public health threat posed by commercial sex. The NSW Department of Health has worked co-operatively with SWOP for over 20 years aided by a decriminalised legal climate without the unnecessary expense21 and access barriers22 created by regulation. However, the NSW sex industry turns over half of its workforce every year13 so the potential for rapid change and the need for ongoing health promotion programs are not diminished.
Acknowledgment
The Law and Sexworker Health (LASH) study was funded by the NHMRC Project Grant no. 352437.
[1]
[2] Donovan B. Gonorrhoea in a Sydney house of prostitution. Med J Aust 1984; 140 268–71.
| PubMed | CAS | (Cited 02 March 2010.)
[11] O’Connor CC, Berry G, Rohrsheim R, Donovan B. Sexual health and condom use among local and international sex workers in Sydney. Genitourin Med 1996; 72 47–51.
| PubMed | CAS |

[12]
[13]
[14] Pell C, Pell C, Dabbhadatta J, Harcourt C, Tribe K, O’Connor CC. Demographic, migration status, and work-related changes in Asian female sex workers surveyed in Sydney, 1993 and 2003. Aust N Z J Public Health 2006; 30 157–62.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[15] Prestage G, Mao L, Jin F, Grulich AE, Kaldor JM, Kippax S. Sex work and risk behaviour among HIV-negative men. AIDS Care 2007; 19 931–4.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[16] Estcourt CS, Marks C, Rohrsheim R, Johnson AM, Donovan B, Mindel A. HIV, sexually transmitted infections, and risk behaviours in male commercial sex workers in Sydney. Sex Transm Infect 2000; 76 294–8.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[17]
[18] Rissel CE, Richters J, Grulich AE, de Visser RO, Smith AMA. Sex in Australia: experiences of commercial sex in a representative sample of adults. Aust N Z J Public Health 2003; 27 191–7.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[19] Paul C, Dickson N, Davis P, Yee RL, Chetwynd J, McMillan N. Heterosexual behaviour and HIV risk in New Zealand: data from a national survey. Aust J Public Health 1995; 19 13–8.
| PubMed | CAS |

[20] Coughlan E, Mindel A, Estcourt CS. Male clients of female commercial sex workers: HIV, STDs and risk behaviour. Int J STD AIDS 2001; 12 665–9.
| Crossref | GoogleScholarGoogle Scholar | PubMed | CAS |

[21] Wilson DP, Heymer K-J, Anderson J, O’Connor J, Harcourt C, Donovan B. Sex workers can be screened too often: a cost-effectiveness analysis in Victoria, Australia. Sex Transm Infect 2010; 86 117–25.
| PubMed |

[22] Chen MY, Donovan B, Harcourt C, Morton A, Moss L, Wallis S, et al. Estimating the number of unlicensed brothels operating in Melbourne. Aust N Z J Public Health 2010; 34 67–71.
| Crossref | GoogleScholarGoogle Scholar | CAS |


