Chronic disease and climate change: understanding co-benefits and their policy implications
Anthony G. Capon A B E and Chris E. Rissel C DA National Centre for Epidemiology and Population Health, The Australian National University
B Faculty of the Built Environment, The University of New South Wales
C Health Promotion Service, Sydney South West Area Health Service
D School of Public Health, University of Sydney
E Corresponding author. Email: tony.capon@anu.edu.au
NSW Public Health Bulletin 21(6) 109-113 https://doi.org/10.1071/NB10032
Published: 16 July 2010
Abstract
Chronic disease and climate change are major public policy challenges facing governments around the world. An improved understanding of the relationship between chronic disease and climate change should enable improved policy formulation to support both human health and the health of the planet. Chronic disease and climate change are both unintended consequences of our way of life, and are attributable in part to the ready availability of inexpensive fossil fuel energy. There are co-benefits for health from actions to address climate change. For example, substituting physical activity and a vegetable-rich diet for motor vehicle transport and a meat-rich diet is both good for health and good for the planet. We should encourage ways of living that use less carbon as these can be healthy ways of living, for both individuals and society. Quantitative modelling of co-benefits should inform policy responses.
Chronic diseases are by far the leading cause of death in the world and their impact is steadily growing.1 Australia is no exception.2 Despite a currently increasing life expectancy, our country is in the grip of an epidemic of chronic disease; for example during 2006 obesity overtook tobacco smoking as the leading risk factor for disease burden in Western Australia.3 We can anticipate similar transitions in all Australian States. The interplay between physical and mental health, and the links between chronic disease and depression, warrant integrated approaches to the prevention of physical and mental health problems.
At the same time, Australia’s per capita greenhouse gas emissions are the highest of any OECD (Organisation for Economic Co-operation and Development) country and among the highest in the world.4 Greenhouse gas emissions contribute to climate change which effects health in a number of ways.5,6 Climate change was recently described in the Lancet as the biggest global health threat of the 21st century.7
Chronic disease and climate change both demand strong public policy responses. The case for aligning policy responses to climate change and public health was cogently argued in the recent series of papers in the Lancet on health and climate change.8 The authors reported research on the ancillary health effects of policies to reduce greenhouse gas emissions in the transport, food, housing and energy sectors. This special issue of the Bulletin presents some Australian perspectives on the co-benefits for health from action to mitigate climate change in association with the Australian Academy of Science’s 2010 Fenner Conference on the Environment which addressed this theme (see abstract of keynote address on page 114).
The concept of co-benefits
A co-benefit is an additional benefit arising from an action that is undertaken for a different principal purpose.9 Putative co-benefits from action on climate change (i.e. additional benefits beyond greenhouse gas reductions) include reduced air pollution, increased levels of physical activity, a healthier diet, improved energy security through a more diverse energy supply and less dependency on oil, a reduction in traffic congestion, and new employment opportunities. In other sectors, this approach to co-benefits is sometimes referred to as a ‘no-regrets approach’ because, even in the absence of a need to act on climate change, there are already strong arguments for many of the proposed actions.
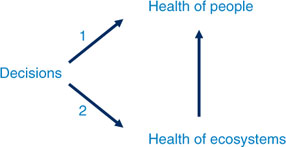
Figure 1 is a diagrammatic representation of the concept of co-benefits for health. Decisions made by individuals, governments and industry have potential direct human health impacts (1) via pathways including nutrition and level of physical activity, and indirect human health impacts (2) via the health of ecosystems (e.g. climate change). It follows that there can be co-benefits for health from actions to address climate change. For clarity, the arrows are presented as uni-directional, however there are relationships in both directions.10
|
Understanding current human situations
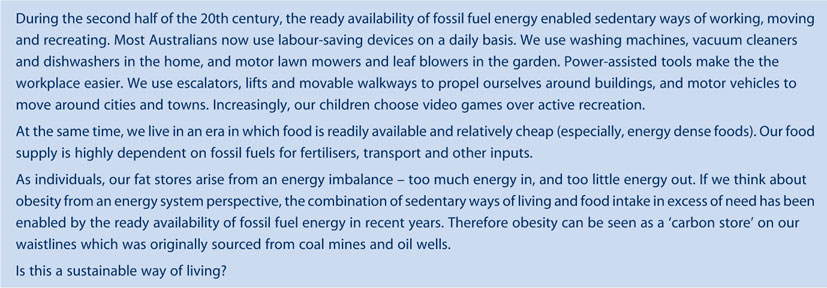
There is value in understanding epidemics of chronic disease from an evolutionary perspective. Human beings are now living in very different ways than our hunter-gatherer ancestors did. The evolutionary health principle postulates that if an animal’s environment changes in a significant way, then it is likely that the animal will be less well adapted to the new conditions and will consequently show signs of physiological or behavioural maladjustment.11 From an evolutionary perspective, chronic disease can be seen to substantially arise from human maladaptation to the current ready availability of fossil fuel energy (Box 1). Further information about this perspective has been presented in two special issues of the NSW Public Health Bulletin on Cities, Sustainability and Health in 2007 (Vol. 18 Issue 3–4 and Issue 11–12) (available at: http://www.publish.csiro.au/issue/4094.htm).
|
The papers in this issue
The papers in this issue of the Bulletin build on the Lancet’s Health and Climate Change Series12 and present Australian perspectives on co-benefits for health from action on climate change. Giles-Corti and colleagues explore the theme of urban land transport addressed by Woodcock et al.13 This paper considers the co-benefits of investing in active transportation, with a focus on policy options to optimise societal objectives aimed at creating healthy, socially and environmentally sustainable communities.
Friel, consistent with the Lancet article on food and agriculture,14 describes the relationship between food security, chronic disease and climate change. She demonstrates how a key climate change mitigation policy – the reduction of greenhouse gas emissions from the agriculture sector through a reduction in consumption of animal source foods – can improve food security and reduce the levels of cardiovascular diseases and some cancers.
Dennekamp and Carey describe the increasing evidence that air pollution contributes to an unacceptable burden of chronic disease and premature mortality, particularly from cardiovascular and respiratory causes. They argue that the action now required to mitigate climate change also has the potential co-benefit of improving air quality and reducing the incidence of chronic disease. Unsurprisingly, they highlight fossil fuel combustion, primarily from motor vehicles and energy generation, as being at the heart of both climate and health-related problems.15
Berry and colleagues, taking a focus on Aboriginal wellbeing and its strong relation to connectedness to traditional country, argue that public health policy must build on Aboriginal people’s determination to care for country, traditional knowledge, formidable resilience and self-determination. They posit that Aboriginal-initiated natural resource management directed at climate change adaption supports caring for land and country with mental health, social and emotional wellbeing co-benefits.
Thompson, Whitehead and Capon describe a new research and workforce development program focused on health and the built environment, recently established in the Faculty of the Built Environment at The University of NSW, with funding from the NSW Department of Health. The NSW Healthy Built Environments Program will foster cross-disciplinary research, deliver education and workforce development, and advocate for health as a primary consideration in built environment decision making. This program will employ an understanding of the co-benefits for health from action on climate change in the framing of research projects, education and advocacy.
Implications for policy and practice
There is increasing recognition that strategies to mitigate climate change can have substantial benefits for both health and climate protection, and that these mitigation strategies are both cost-effective and socially attractive.16 A Win-Win-Win approach (Box 2), based on the concepts of the triple bottom line,17 and also known as ‘people, planet, profit’ or ‘the three pillars’, captures an expanded spectrum of values and criteria for measuring organisational (and societal) success – economic, ecological and social.

|

|
Some climate change strategies may look appealing, but are not the whole solution. An example is electric cars. While electric cars do not directly produce emissions, drivers are still sedentary and don’t have the health advantages of active travel. Further, if vehicles remain the same size, and take up the same amount of space, then it will make no difference to traffic congestion problems (which are estimated to cost Australia $64 million a year). If, as is likely, the electricity used in electric cars comes from coal-fired power plants, then the net effect on greenhouse gas emissions may be negative. Increasing active urban travel, and discouraging private motor vehicle use, will provide larger health benefits than policies focusing on lower emission motor vehicles.13
An understanding of co-benefits for health from action on climate change should inform policy responses to both chronic disease and climate change. Quantitative modelling of these co-benefits from an Australian perspective, including economic modelling, should be an urgent priority, preferably in advance of national decision making about carbon regulation. An understanding of co-benefits could assist prioritisation of policy interventions in the health sector and other relevant sectors (e.g. transport, energy, agriculture). Potential for unintended consequences for health, and health equity, should be carefully weighed.
An understanding of co-benefits may also have direct implications for clinical practice. For example, a diabetes education consultation for a patient with early diabetes could include information about building active forms of travel into daily life. To be effective, this will require health workers to work with other sectors (e.g. urban and transport planning) to reduce barriers to healthy ways of living.
The take home message about co-benefits is that low carbon ways of living are healthy ways of living. Health workers and health systems should promote this positive message.
Acknowledgment
AG Capon receives research funding from the National Climate Change Adaptation Research Facility, the CSIRO Flagship Collaboration Fund, and from an NHMRC Australia Fellowship award to Professor AJ McMichael.
[1]
[2]
[3] Hoad V, Somerford P, Katzenellenbogen J. High body mass index overtakes tobacco as the leading independent risk factor contributing to disease burden in Western Australia. Aust N Z J Public Health 2010; 34 214–5.
| Crossref | GoogleScholarGoogle Scholar | (Accessed 6 April 2010.)
[10]
[11]
[12] Horton R. The climate dividend. Lancet 2009; 374 1869–70.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[13] Woodcock J, Edwards P, Tonne C, Armstrong BG, Ashiru O, Banister D, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: urban land transport. Lancet 2009; 374 1930–43.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[14] Friel S, Dangour AD, Garnett T, Lock K, Chalabi Z, Roberts I, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: food and agriculture. Lancet 2009; 374 2016–25.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[15] Smith KR, Jerrett M, Anderson HR, Burnett RT, Stone V, Derwent R, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: health implications of short-lived greenhouse pollutants. Lancet 2009; 374 2091–103.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[16] Haines A, McMichael AJ, Smith KR, Roberts I, Woodcock J, Markandya A, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. Lancet 2009; 374 2104–14.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[17] Elkington J. Towards the sustainable corporation: Win-win-win business strategies for sustainable development. Calif Manage Rev 1994; 36(2): 90–100.

[18] Rissel CE. Active travel: a climate change mitigation strategy with co-benefits for health. NSW Pub Health Bull 2009; 20 10–3.
| Crossref | GoogleScholarGoogle Scholar |


