Measles in NSW, 2002–2011
Alexander Rosewell A B , Tracie Reinten-Reynolds A and Paula J. Spokes AA Health Protection NSW
B Corresponding author. Email: arosw@doh.health.nsw.gov.au
NSW Public Health Bulletin 23(10) 201-207 https://doi.org/10.1071/NB12085
Published: 12 December 2012
Abstract
Measles has been eliminated in NSW for more than a decade; however outbreaks associated with international travel do occur. This EpiReview describes the epidemiology of measles in NSW from 2002–2011. A total of 281 cases of measles were notified during the period, an average annual notification rate of 0.41 notifications per 100 000 population (range: 0.06–1.25). There were 139 hospitalisations recorded with a measles diagnosis in the 10-year reporting period, corresponding to a rate of 0.20 hospitalisations per 100 000 population. Of the 80 measles virus specimens genotyped, five genotypes were identified: D9 (38%), D8 (24%), D4 (16%), D5 (14%) with H1 identified less frequently (9%). No single genotype was associated with local transmission across successive years. To sustain good measles control, children should be vaccinated against measles on time through routine childhood immunisation, and all young adults who travel internationally should be vaccinated. Clinician awareness remains important in the early identification and control of measles to avoid further transmission during outbreaks and to enable the timely implementation of public health measures.
Measles is an acute and highly contagious viral disease that is currently the most important cause of vaccine-preventable death globally.1 Measles is rare in Australia with low rates of hospitalisation and death.2 Measles is transmitted by airborne particles, droplets or fomites and humans are the only host of the measles virus. Common symptoms of measles include fever, rash, cough, coryza, conjunctivitis, diarrhoea and loss of appetite. Complications include ear infections, pneumonia, convulsions, croup, encephalitis and death. A milder illness is sometimes seen in vaccinated individuals,3 and severe disease tends to occur in infants and malnourished persons.1 Sub-acute sclerosing panencephalitis is a rare, delayed, fatal complication of measles virus infection.
In Australia, measles-mumps-rubella (MMR) vaccines are scheduled as two doses for all children: the first at 12 months and the second at 4 years of age.4 In 2013, the inclusion of measles-mumps-rubella-varicella vaccine (MMR-V) on the childhood immunisation schedule will bring forward the second measles dose to 18 months from 4 years.5 In addition, documented immunity to measles has been a mandatory requirement for new health care workers in New South Wales (NSW) since 2007. In NSW, the percentage of children immunised with at least one dose of MMR at 2 years of age is 93.9%,6 with some variation across local health districts (LHDs) and Aboriginal communities.7 People at highest risk of measles infection include: infants aged less than 1 year (who are too young to be vaccinated); children aged 1–4 years who have received only a single dose of vaccine, especially if received late; and those born in the late 1960s to mid 1980s (who were neither infected with measles, nor vaccinated against it).8
Multiple lines of evidence suggest measles elimination (the absence of endemic measles transmission) has been achieved in Australia since 1999.9 Contributing to this was the high population immunity achieved during the measles control campaign (1998) and maintained through high vaccination rates among children.9 High vaccination coverage is required for each new birth cohort to maintain measles elimination: at least 95% for a single dose and at least 90% for two doses.4
However, outbreaks do occur in NSW and are generally linked to case-patients who acquired their illness overseas. Further transmission has historically been contained to non-immune direct contacts and contained within one to two generations of transmission. The number of chains of transmission from imported case-patients is directly related to the pool of susceptible people in the population. At the time of publication the largest measles outbreak in more than a decade was being investigated across metropolitan Sydney affecting infants too young to be vaccinated and some population groups with apparent low vaccination coverage.
An objective of measles surveillance is the timely detection of all cases10 to enable the identification and implementation of public health measures to limit the spread of infection. Control strategies include protection of contacts through administration of vaccine or normal human immunoglobulin, active case finding, exclusion and isolation.11 Measles surveillance also enables the epidemiological monitoring of the disease to inform prevention strategies. In this report we describe measles epidemiology in NSW from January 2002 to December 2011.
Methods
Notification and hospitalisation data were used to describe trends in measles epidemiology in NSW.
Notifications
During this period, doctors, hospitals and laboratories were required to notify all measles cases to their local public health unit (PHU) under the NSW Public Health Act 1991*. Measles cases were defined according to National Case Definitions. The case definitions remained constant during the reporting period. A ‘confirmed’ case requires laboratory definitive or clinical and epidemiological evidence, a ‘probable’ case requires clinical and laboratory suggestive evidence, and a ‘suspected’ case requires clinical evidence alone.12 In this report, a person with an illness that meets the case definition is called a case-patient.
On receipt of a notification, a public health unit surveillance officer determines whether or not the notification meets the definition of a case of measles, and if so, enters data gathered on each notified case into the NSW Notifiable Conditions Information Management System (NCIMS). Vaccination status is collected by these officers and, where possible, validated using the Australian Childhood Immunisation Register (since 1996) or other forms of evidence. We analysed the NCIMS notification data for measles cases with onset dates during the 10-year period from January 2002 to December 2011. Average annual case notification rates were calculated using annual mid-year population estimates from the Australian Bureau of Statistics (ABS).
Genotyping is generally performed in defined circumstances to support public health investigations. Sequencing and genotyping is routinely performed by the Victorian Infectious Diseases Reference Laboratory. Genotyping involves the amplification of part of the N (nucleocapsid) gene, and genotype classification is based on nucleic acid sequencing of the polymerase chain reaction products using established methods.13
Hospitalisations
Measles hospitalisation data was obtained from the Admitted Patient Data Collection for NSW residents with an ICD-10-AM diagnosis code of B05 (measles) admitted between July 2001 and June 2011. Hospitalisation rates were calculated using annual end-year population estimates from the ABS.
Results
Notifications
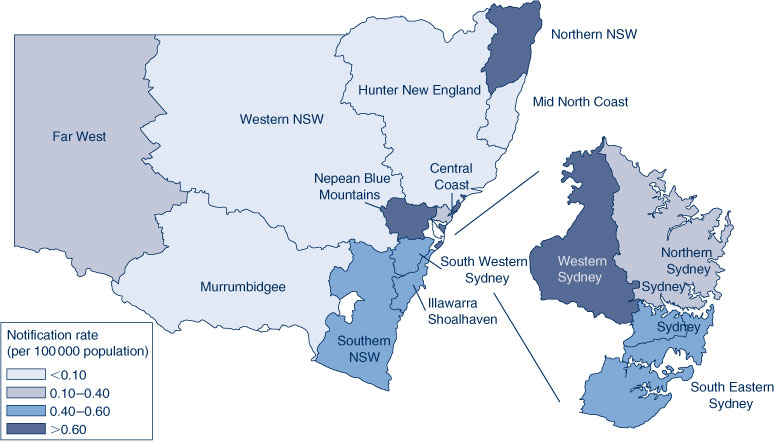
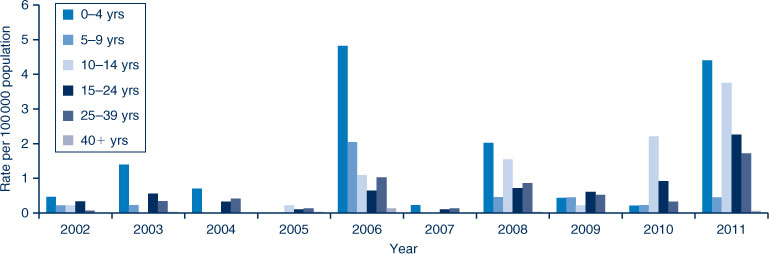
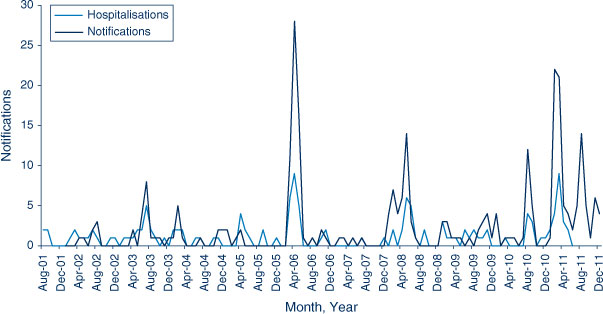
During the 10-year reporting period, 281 cases of measles were notified at an average annual notification rate of 0.41 per 100 000 population (range: 0.06–1.25). Of the 281 cases of measles, 247 (88%) were laboratory confirmed, with no trend in the annual case confirmation rates identified (range: 80–100%). There were case notifications every year, with as many as 90 reported in 2011 and as few as four in 2007; 2011 was also the first year in the study period when cases were reported every month (Figure 1). The highest average annual case notification rate in this period was in Northern NSW LHD (0.71 per 100 000 population) and the lowest was in Western NSW LHD (0.04 per 100 000 population) (Figure 2). In total, 145 of the measles case-patients (52%) were male, with annual fluctuations (range: 40–75%). There were 66 measles case-patients who were children aged under 5 years (24% of all measles cases) (Figure 3), of which 21 (7% of all measles case-patients) were infants aged under 1 year. Measles case notification rates were highest in the under 5-year age group (1.49 per 100 000 population) followed by 10–14-year olds (0.92 per 100 000 population) and 15–19-year olds (0.82 per 100 000 population). Notification rates for case-patients less than 5 years of age peaked in 2006 at 4.81 per 100 000 population (35% of 2006 cases) and were lowest in 2005 (n = 0). During this period, the majority of case-patients (n = 274, 98%) were among those born during or since 1966. Since then, measles has been less common and people were unlikely to have been exposed to the illness as a child.
|
The completeness of reporting Aboriginal status for measles cases improved during the reporting period, with an average annual completeness of 92% (range: 78–100%). There were 11 case-patients identified as Aboriginal people (rate 0.72 per 100 000 population), which was almost double that of non-Aboriginal people (Rate Ratio = 1.80; 95% CI 0.27–12.11). Nearly all (n = 10) of these cases occurred in 2011 and were distributed across three LHDs: South Eastern Sydney, Illawarra Shoalhaven and Western Sydney. In 2011, case notification rates were significantly higher for Aboriginal people compared to non-Aboriginal people (6.03 and 1.14 per 100 000, respectively).
Of the 281 cases, 145 (52%) had not been vaccinated, 72 (26%) had unknown vaccination status, while 62 (22%) reported being partially and two fully vaccinated. Of the 217 without evidence of vaccination, 21 were too young to vaccinate (less than 1 year old), 31 were aged between 1 and 4 years, and 165 were aged over 4 years. Of the notifications in children aged 18 months to 4 years, 20 (77%) had not been vaccinated or had unknown vaccination status.
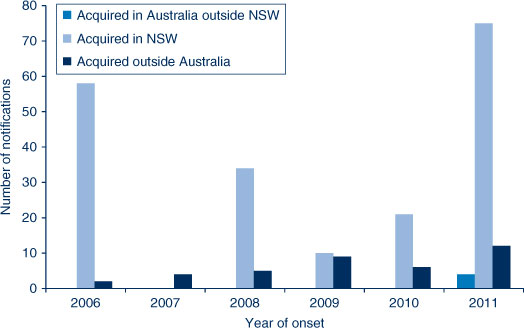
During the period, measles outbreaks were associated with infectious residents returning from international travel and infecting unimmunised people upon their return. Affected groups included high school students, culturally and linguistically diverse groups, prisoners, a faith-based group, infants too young to be immunised, children in child care, as well as visitors to general practices and emergency departments.3,14–18 There were 38 case-patients who acquired measles outside of Australia; one was in a visitor from overseas, the remainder were NSW residents returning from overseas travel (Figure 4). The median age of case-patients who acquired their infection overseas was 19 years (range: 6 months–41 years). The geographic origin of most of these imported measles cases were from the Asia Pacific and European regions.
|
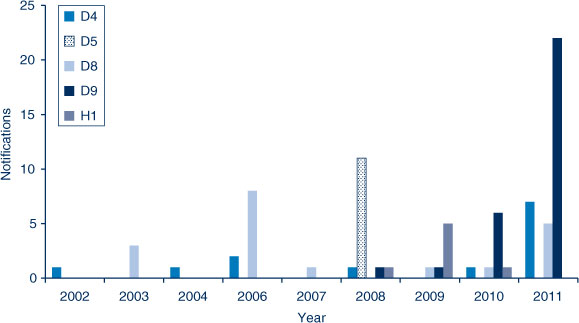
Internationally, there are eight different clades and 24 subclades of measles viruses referred to as genotypes.19 During the reporting period, 80 (28%) measles case-patients had specimens genotyped: 30 were found to be D9 (38%), 19 were D8 (24%), 13 were D4 (16%), 11 were D5 (14%) with H1 identified less frequently (9%) (Figure 5). No single genotype was identified in a large number of successive years, with the largest annual diversity of genotypes being four in 2008 and 2010, then three in 2009 and 2011, with fewer in other years.
|
Hospitalisations
There were 139 hospitalisations recorded with a measles diagnosis in the 10-year reporting period, corresponding to a rate of 0.20 hospitalisations per 100 000 population. There were 54 measles hospitalisations reported in children aged under 5 years (39% of all measles hospitalisations), of which 21 were aged under 1 year. Hospitalisation rates in the under 5-year age group peaked in 2005–2006 at 2.08 per 100 000 (38% of 2005–2006 measles hospitalisations) and were lowest in 2004–2005 (n = 1). Hospitalisation rates were highest in those aged under 5 years (1.22 per 100 000 population) followed by 30–34-year olds (0.44 per 100 000) and 25–29-year olds (0.33 per 100 000). There were seven hospitalisations recorded with a diagnosis of measles in those aged over 65 years (in the same period, there were no measles notifications in this age group). There were seven Aboriginal people hospitalised with measles in the 10-year period (5% of all measles hospitalisations), associated with a hospitalisation rate of 0.46 per 100 000 population. Aboriginal people had a 2.4 (95% CI 0.2–25.5) times greater yearly measles hospitalisation rate than non-Aboriginal people in NSW between 2001–2002 and 2010–2011. Measles with complications were reported in 25 cases (18%); encephalitis was reported in two cases, one in 2003–2004 and the other in 2010–2011; and measles complicated by pneumonia was recorded in 10 cases.
Discussion
Measles has generally been well controlled in NSW over the past decade. However, outbreaks of limited duration have occurred. For example, in 2006 an outbreak affecting more than 40 case-patients was found to be associated with a national tour of a spiritual leader. The public health investigation found that some members of the tour group were likely to have been infected with measles prior to their arrival in Australia.17 Further transmission occurred in families members associated with the tour group.
Outside of the occasional outbreak, there have been low numbers of measles cases notified. In addition, cases have been found to have various genotypes identified during the period with no indigenous measles strain identified during the last decade. Sequencing and genotyping are powerful molecular tools to support epidemiological investigations and to assist countries to adhere to elimination criteria.13 Access to genotyping information for measles cases is important to demonstrate the interruption of circulating virus strains and identify new importations of the measles virus.
The average annual case notification rate during the 10-year period dropped markedly compared to the previous report for the period 1991–2000 (from 10.4 to 0.41 per 100 000 population).20 Case notification rates differed by geographic area and were highest in the LHD with the lowest vaccination coverage.21 The 0–4-year old age group had the highest notification rates, and within this age group most case patients were aged between 18 months and 4 years. We found that 52% of all case patients had not received any doses of measles-containing vaccine. Some of the unvaccinated case-patients were due or overdue for measles-containing vaccine, which is supported by a detailed analysis of cases notified in 2011.13 This highlights the importance of timely childhood vaccination. The introduction of MMR-V vaccine and bringing forward the timing of the second measles dose may further reduce disease burden among 0–4-year olds.
Under-immunised population groups that are susceptible to measles remain a feature of outbreaks, including: prisoners, culturally and linguistically diverse groups, as well as persons who object to the vaccination of their children. As with previous national reports,22,23 measles case notification rates and hospitalisation rates were almost double for Aboriginal people during the overall reporting period but was not found to be statistically significant. However in 2011, this differential increased, and Aboriginal persons had statistically significantly higher measles notification rates.
Measles surveillance systems will not always identify every case of disease,13,24 as evidenced by the retrospective identification of measles index cases in emergency department outbreaks13,25,26 and through analysis of the hospitalisation data that identified possible case-patients that were not notified. Diagnostic or coding errors would most likely explain the additional measles hospitalisations identified among persons aged 65 years and over that were not notified. This misclassification may contribute to an overestimation of measles hospitalisations. Strategies for enhancing clinician awareness of measles are important for early diagnosis and have been successfully implemented at the LHD level in NSW.27
Despite the successes in regional and global measles control since 2000,28,29 unvaccinated young international travellers remain at risk of infection (and a potential source of infection for unimmunised contacts), as demonstrated by the international travel history among index case-patients identified in NSW clusters during the reporting period. As with other countries where measles has been eliminated, importations have been found to reflect travel destinations rather than global measles incidence.30 In the context of steadily increasing short term international departures from NSW during the reporting period, which reached the highest on record in 2011,31 the current targeting of this group with communication interventions by health authorities would appear relevant. The median age of imported measles cases indicates that international travellers of school age should also be targeted, as evidenced by the outbreaks among school groups returning from overseas trips and in schools subsequent to student travel to affected areas.
Conclusion
Vaccination remains the only available protection against measles and is highly effective. Several challenges remain for NSW to maintain good measles control. All children should be vaccinated against measles on time through routine childhood immunisation. Identifying inadequately vaccinated children at the time of school entry could provide a fail-safe mechanism to increase immunisation coverage to the levels required to sustain control over the long-term. All young adults who travel internationally should be vaccinated. Continued effort is required to improve vaccination coverage among under-immunised populations; including prisoners, culturally and linguistically diverse communities and Aboriginal communities. Clinician awareness remains important in the early identification and control of measles to avoid outbreaks, and to enable the timely implementation of public health measures.
Acknowledgments
We acknowledge those who have notified cases of measles as well as the surveillance officers in public health units who manage NCIMS data. We also recognise the crucial work of laboratories performing measles diagnosis and are extremely grateful to the Victorian Infectious Diseases Reference Laboratory for performing sequencing and genotyping of specimens.
References
[1] Moss WJ, Griffin DE. Measles. Lancet 2012; 379 153–64.| Measles.Crossref | GoogleScholarGoogle Scholar |
[2] Chiu C, Dey A, Wang H, Menzies R, Deeks S, Mahajan D, et al. Vaccine preventable diseases in Australia, 2005 to 2007. Commun Dis Intell 2010; 34 S1–167.
[3] Sheppeard V, Forssman B, Ferson MJ, Moreira C, Campbell-Lloyd S, Dwyer DE, et al. Vaccine failures and vaccine effectiveness in children during measles outbreaks in New South Wales, March-May 2006. Commun Dis Intell 2009; 33 21–6.
[4] National Health and Medical Research Council. The Australian Immunisation Handbook. 9th ed. Canberra: Australian Government Department of Health and Ageing; 2008.
[5] Australian Government Department of Health and Ageing. Immunise Australia Program. Available at: http://www.immunise.health.gov.au/ (Cited October 2012).
[6] National Centre for Immunisation Research and Surveillance. Vaccination. National vaccination coverage estimates. Available at: http://www.ncirs.edu.au/immunisation/coverage/estimates/index.php (Cited October 2012).
[7] Macartney KK, Durrheim DN. NSW immunisation performance: continuing progress but no room for complacency. N S W Public Health Bull 2011; 22 169–70.
| NSW immunisation performance: continuing progress but no room for complacency.Crossref | GoogleScholarGoogle Scholar |
[8] Gidding HF, Gilbert GL. Measles immunity in young Australian adults. Commun Dis Intell 2001; 25 133–6.
[9] Heywood AE, Gidding HF, Riddell MA, McIntyre PB, MacIntyre CR, Kelly HA. Elimination of endemic measles transmission in Australia. Bull World Health Organ 2009; 87 64–71.
| Elimination of endemic measles transmission in Australia.Crossref | GoogleScholarGoogle Scholar |
[10] Heath T, Burgess M, McIntyre P, Catton M. The national measles surveillance strategy. The National Centre for Disease Control Measles Elimination Advisory Committee. Commun Dis Intell 1999; 23 41–50.
[11] NSW Ministry of Health. Measles response protocol. Available at: http://www.health.nsw.gov.au/factsheets/guideline/measles.html (Cited October 2012).
[12] Australian Government Department of Health and Ageing Communicable Diseases Network Australia. Measles case definition. Available at: http://www.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-nndss-casedefs-cd_measl.htm (Cited October 2012).
[13] Jayamaha J, Binns PL, Fennell M, Ferson MJ, Newton P, Tran T, et al. Laboratory diagnosis, molecular characteristics, epidemiological and clinical features of an outbreak of measles in a low incidence population in Australia. J Clin Virol 2012; 54 168–73.
| Laboratory diagnosis, molecular characteristics, epidemiological and clinical features of an outbreak of measles in a low incidence population in Australia.Crossref | GoogleScholarGoogle Scholar |
[14] Spokes PJ, Gilmour RE. NSW Annual Vaccine-Preventable Disease Report, 2010. N S W Public Health Bull 2011; 22 171–8.
[15] Spokes PJ, Gilmour RE. NSW Annual Vaccine-Preventable Disease Report, 2009. N S W Public Health Bull 2010; 221 197–209.
[16] Communicable Diseases Report, NSW, January and February 2008. N S W Public Health Bull 2008; 19 78
[17] Communicable Diseases Report, NSW, March and April 2006. N S W Public Health Bull 2006; 17 88–94.
| Communicable Diseases Report, NSW, March and April 2006.Crossref | GoogleScholarGoogle Scholar |
[18] Communicable Diseases Report, NSW, for May 2003. N S W Public Health Bull 2003; 14 151–8.
[19] Measles virus nomenclature update: 2012. Wkly Epidemiol Rec 2012; 87 73–81.
[20] Brotherton J. EpiReview: Measles in NSW, 1991–2000. N S W Public Health Bull 2001; 12 200–4.
| EpiReview: Measles in NSW, 1991–2000.Crossref | GoogleScholarGoogle Scholar |
[21] Hull B, Dey A, Campbell-Lloyd S, Menzies RI, McIntyre PB. NSW Annual Immunisation Coverage Report, 2010. N S W Public Health Bull 2011; 22 179–95.
| NSW Annual Immunisation Coverage Report, 2010.Crossref | GoogleScholarGoogle Scholar |
[22] Menzies R, Turnour C, Chiu C, McIntyre P. Vaccine preventable diseases and vaccination coverage in Aboriginal and Torres Strait Islander people, Australia 2003 to 2006. Commun Dis Intell 2008; 32 S2–67.
[23] Menzies R, McIntyre P, Beard F. Vaccine preventable diseases and vaccination coverage in Aboriginal and Torres Strait Islander people, Australia, 1999 to 2002. Commun Dis Intell 2004; 28 S1–45.
[24] Measles – United States. 2011. MMWR 2012; 61(15): 253–7. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6115a1.htm?s_cid=mm6115a1_e (Cited October 2012).
[25] Bowen AC, Ferson MJ, Palasanthiran P. Consequences of an unrecognized measles exposure in an emergency department. Emerg Med Australas 2009; 21 491–6.
| Consequences of an unrecognized measles exposure in an emergency department.Crossref | GoogleScholarGoogle Scholar |
[26] Hope K, Boyd R, Conaty S, Maywood P. Measles transmission in health care waiting rooms: implications for public health response. Western Pacific Surveillance and Reponse Journal (in press).
[27] Kohlhagen JK, Massey PD, Durrheim DN. Meeting measles elimination indicators: surveillance performance in a regional area of Australia. Western Pacific Surveillance and Response Journal 2011; 2, e1–e1.
[28] Medicine NL. of Progress Towards the 2012 Measles Elimination Goal in WHO’s Western Pacific Region, 1990–2008. Relevé épidémiologique hebdomadaire/Section d’hygiène du Secrétariat de la Société des Nations = Weekly epidemiological record/Health Section of the Secretariat of the League of Nations 2009; 84, 271–9.
[29] Progress in global measles control, 2000–2010. Wkly Epidemiol Rec 2012; 87 45–52.
[30] Rota PA, Rota JS, Redd SB, Papania MJ, Bellini WJ. Genetic analysis of measles viruses isolated in the United States between 1989 and 2001: absence of an endemic genotype since 1994. J Infect Dis 2004; 189 S160–4.
| Genetic analysis of measles viruses isolated in the United States between 1989 and 2001: absence of an endemic genotype since 1994.Crossref | GoogleScholarGoogle Scholar |
[31] Australian Bureau of Statistics 3401.0 – Overseas Arrivals and Departures, Australia, Dec 2011 Media release: Short-term resident departures reach all time high. (2012). Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Previousproducts/3401.0Media%20Release1Dec%202011?opendocument&tabname%Summary&prodno=3401.0&issue=Dec%202011&num=&view= (Cited October 2012).
* The Public Health Act 2010 (NSW) (http://www.health.nsw.gov.au/phact/)
The Public Health Act 2010 (NSW) was passed by the NSW Parliament in December 2010 and commenced on 1 September 2012. The Public Health Regulation 2012 was approved in July 2012 and commenced, along with the Public Health Act 2010 (NSW), on 1 September 2012. The objectives of the Regulation are to support the smooth operation of the Act. The Act carries over many of the provisions of the Public Health Act 1991 (NSW) while also including a range of new provisions.