#TheHealthYouthWant: a qualitative analysis of a global crowdsourcing open call for innovative ideas to promote adolescent health and well-being in countries with a high HIV burden
Takhona G. Hlatshwako A , Ifeoma Obionu B , Yang Zhao C , Kelechi Chima
A , Ifeoma Obionu B , Yang Zhao C , Kelechi Chima  D , Brian Ahimbisibwe E , Chisom Obiezu-Umeh F , Eleanor Namusoke Magongo G , Onyekachukwu Anikamadu H , Oliver Ezechi I J , Dorian Ho K , Yusha Tao L , Susan Vorkoper M , Rachel Sturke N , Juliet lwelunmor O , Damilola Walker P # and Joseph D. Tucker
D , Brian Ahimbisibwe E , Chisom Obiezu-Umeh F , Eleanor Namusoke Magongo G , Onyekachukwu Anikamadu H , Oliver Ezechi I J , Dorian Ho K , Yusha Tao L , Susan Vorkoper M , Rachel Sturke N , Juliet lwelunmor O , Damilola Walker P # and Joseph D. Tucker  C Q # *
C Q # *
A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
# Joint senior authors
Handling Editor: Tiffany Renee Phillips
Abstract
Improving adolescent health and well-being is a key policy priority in countries with a high HIV burden, because adolescents have lower rates of treatment coverage, viral load suppression and survival compared with others. This study aimed to identify innovative ideas from young people (aged 10–30 years) on how adolescent health and well-being can be improved in communities most affected by HIV.
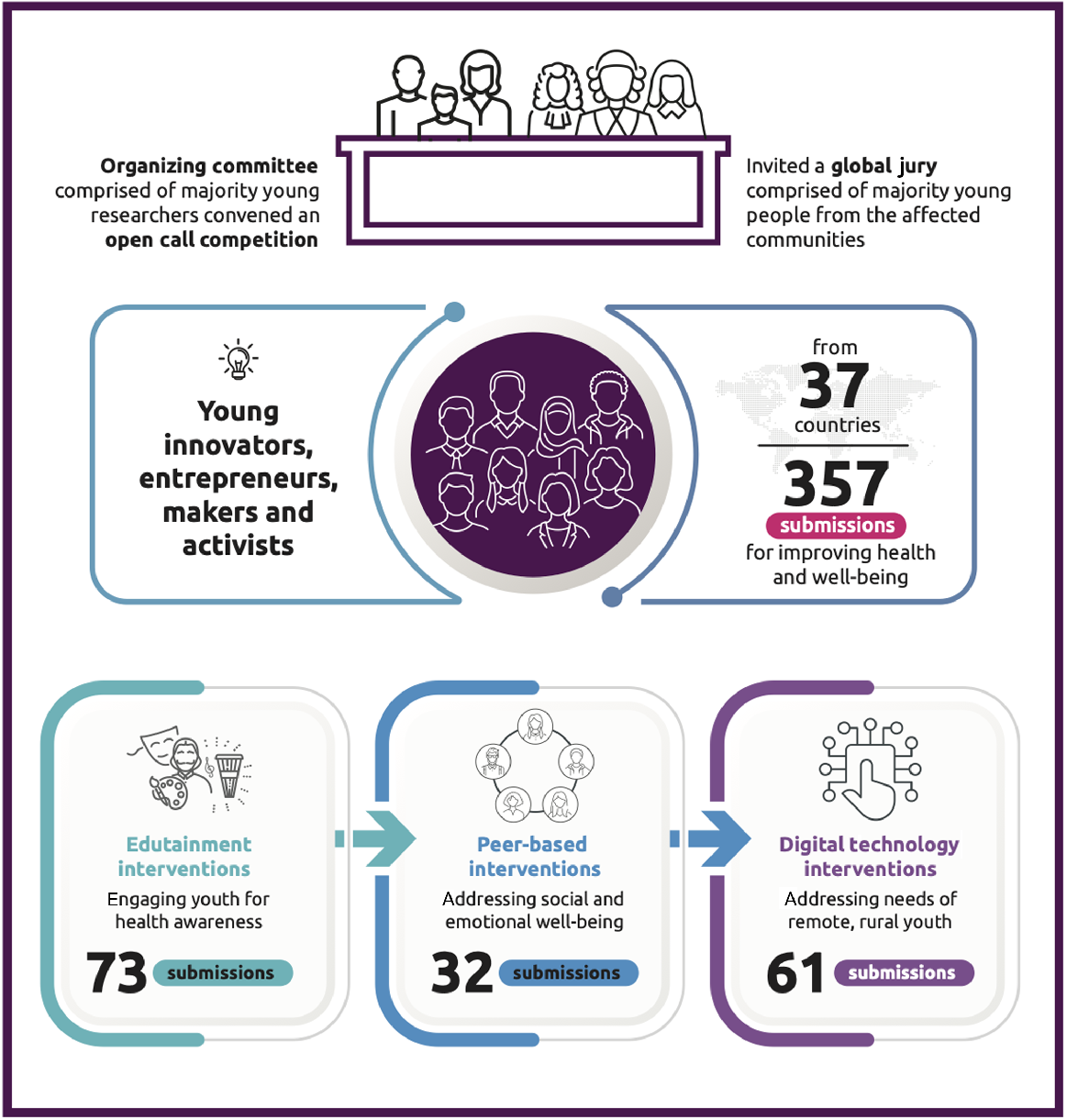
We organized a global crowdsourcing open call for ideas from young people on how to improve adolescent HIV outcomes and well-being in countries with a high HIV burden. At least three independent judges assessed each submission based on prespecified criteria. We then conducted a thematic analysis of eligible submissions to identify key themes to inform HIV programming and policy.
We received 357 submissions from 37 countries. Of 107 eligible submissions, 91 (85%) described new ideas. Seventy-one (66%) participants were aged 20–30 years, and 30 (28%) were aged 10–19 years. Major themes suggested that edutainment interventions linking entertainment and education could increase adolescent uptake of HIV services. Digital interventions adapted for analog cellphone users (e.g. unstructured supplemental service delivery) could increase the reach of HIV information and engage remote, rural participants. Peer-based interventions could improve feelings of social inclusion among adolescents.
Adolescents and young people in countries with a high HIV burden can create innovative and feasible ideas for improving health and well-being. Exceptional ideas were presented to senior leadership at UNICEF/WHO/UNAIDS as part of a multi-sectoral HIV strategic planning exercise.
Keywords: AIDS, crowdsourcing, global health, HIV, low-and-middle-income countries, open call, qualitative study, sexual and reproductive health.
Introduction
Over 1000 young people acquire HIV daily, and the number of adolescents (aged 10–19 years) who are living with or at risk for HIV is growing.1 Adolescents with HIV have lower treatment coverage, worse viral load suppression and higher mortality compared with other age groups.2 Adolescents in high HIV burden countries are not only confronted by HIV, but also face a wider set of vital problems (i.e. climate crises, food insecurity and economic development challenges)3 that have been referred to as polycrises.4 It is estimated that >48 million young people are growing up in contexts where the most intense of these challenges co-occur.5
Improving adolescent health outcomes amidst the polycrisis requires greater adolescent involvement in shaping health programs and policies. Notably, these crises can hinder adolescents’ access to health programs. Therefore, gathering input from adolescents themselves is crucial to understanding how health programs can be made more accessible and beneficial for them. WHO and UN guidance have recommended greater participation of adolescents in shaping adolescent health and well-being programs, especially in low- and middle-income countries.6 However, despite these calls for greater adolescent engagement in shaping health programs,7,8 few adolescents are involved in HIV research, policy and program development.9 A scoping review of youth engagement in HIV prevention studies found that 88% of intervention studies had minimal or no youth engagement.10 Barriers to youth engagement included a lack of training opportunities and capacity building for young people, parental concerns about participating in HIV research, HIV-related stigma, and adult perceptions of young people’s capacity to engage in research.10
In response to this research gap, a youth-led partnership organized a global crowdsourcing open call to engage young people to share innovative ideas on how to improve adolescent health and well-being in high HIV burden countries. Crowdsourcing is the process of having a group of people solve all or part of a problem, and then sharing the crowdsourced solutions with the community.11 An open call is an approach to crowdsourcing that provides a structured framework to solicit ideas from the public. Crowdsourcing is an increasingly used innovative approach for engaging young people in health research and interventions.12 We used a crowdsourcing open call to engage young people and solicit ideas on how to improve adolescent health outcomes in countries with a high burden of HIV. This study aimed to analyze the ideas received through the open call, and then describe overarching themes that can be used to inform HIV program development and policymaking.
Methods
Crowdsourcing open call
A partnership with representatives from UNICEF, WHO, UNAIDS, the Special Programme for Research and Training in Tropical Diseases, For Youth by Youth (4YBY), and Social Entrepreneurship to Spur Health brought together a youth-led group to organize a global crowdsourcing open call in 2023 called ‘#TheHealthYouthWant.’ Following the Special Programme for Research and Training in Tropical Diseases Crowdsourcing in Health and Health Research Practical Guide, the open call included the following steps: forming a youth-led organizing committee, engaging young people to share their ideas; evaluating ideas based on prespecified criteria; recognizing exceptional finalists; and sharing the ideas.11 We used youth participatory action research as a conceptual approach13 to inform the development of the open call. Participatory action research focuses on encouraging participation from key stakeholders, and then using these experiences to catalyze action and research.14 This conceptual approach has been widely used in sexual and reproductive health research,15,16 survey development,17,18 and open innovation.19 In our approach, we used an open call to involve the very stakeholders whose health we seek to improve: adolescents and youth. The open call formed part of a larger multi-sectoral collaboration called the Blueprint Collaborative, which aims to identify actionable steps to improve adolescent health and well-being in high HIV burden countries.
The organizing committee distributed the open call for entries through social media (Instagram, WhatsApp, LinkedIn), email and webinars. The open call solicited submissions from 30 June to 31 July 2023. Young people were invited to provide a brief description (<500 words) or a short video (3 min) answering one of the following challenge questions: ‘How might we totally and fundamentally reimagine organizing our healthcare systems and societies to support adolescent health and well-being in countries that have a high burden of HIV?’ or ‘How might we develop solutions that can support and strengthen adolescent health and well-being in the future, taking into account current and possible threats, such as conflict and pandemics, and current trends, like climate change, rising inequality, migration, urbanization and digitalization?’. The open call had four categories to guide submissions: innovations for health; innovations that promote adolescent-centered processes, systems and policies; innovations for behavioral change related to health; and ‘surprise us’ innovations. The final category was intended for submissions that did not fit clearly into the other categories, but still addressed the main challenge questions. The challenge questions and submission formats were deliberately open-ended to encourage innovation and creativity.
Geographical scope
Participants were asked to focus their idea on the following high HIV burden countries: Brazil, Cameroon, Côte d’Ivoire, the Democratic Republic of Congo, Ethiopia, Kenya, Malawi, Mozambique, Nigeria, Philippines, South Africa, Tanzania, Uganda, Zambia and Zimbabwe. These countries were selected because they account for 75% of the adolescent HIV burden. However, the open call was open to all young people, regardless of geography or location. We chose this inclusive approach to ensure a diverse range of ideas and perspectives, including from youngpeople who have migrated from their country of origin.
Eligibility for participation
The open call solicited ideas from young people to submit ideas on their own or as part of a team. Individuals older than 19 years were encouraged to participate as a member of a team. All teams had to include at least one adolescent, and team leaders could not be older than 30 years. All participants younger than 18 years were required to obtain parental consent before participating in the open call. Participants were allowed to submit ideas in any UN language (English, Arabic, Chinese, French, Spanish, Portuguese or Russian) using an online submission form or via email.
Evaluation of submissions
All submissions were screened for eligibility. A panel of judges rated each submission on a 1–10 scale (1 as worst, 10 as best), and each submission was evaluated by three independent judges. The panel of judges included health research professionals, organizational representatives and youth activists. Pre-specified scoring criteria included clarity of description, relevance, novelty, feasibility, scalability, sustainability, and promotion of equity and fairness (Supplementary material Table S1). Twelve people whose ideas were top-scoring ideas across each category were designated semi-finalists and invited to pitch their ideas to an independent panel of judges. The panelists declared eight finalists (four winners and four runners-up), and their ideas were referred for deliberations by a global collaborative convened to define how adolescent HIV programs might be delivered differently in the future (the Blueprint Collaborative). Evidence and weighting of the effectiveness of these interventions were assessed in a complementary systematic review.20 Finalists and runners-up of the open call received cash prizes (US$1500 for finalists and US$500 for runners-up). Additionally, their ideas were presented to senior leadership at UNICEF/WHO/UNAIDS as part of a multi-sectoral HIV strategic planning exercise aimed at improving adolescent health and well-being.
Data analysis
We conducted a thematic analysis of all eligible submissions to the open call (n = 107). The thematic analysis included several stages: developing a codebook, conducting line-by-line coding of text submissions and video transcriptions; identifying descriptive themes; and generating analytic themes.21 A codebook was developed to classify the submissions into descriptive themes. The codebook was developed using an inductive approach, which involved iteratively identifying ideas that emerged most frequently in the data and characterizing these ideas into categories. Two coders then tested the codebook against a handful of submissions, then made revisions and resolved discrepancies before moving to the stage of complete coding. Each of the two coders reviewed a selection of the submissions. All submissions were then characterized using the codebook, and overarching categories were closely examined to identify analytic themes. Descriptive statistics were used to summarize the characteristics of the primary participants who were listed on the open call submission form (team leads) and their submissions. All analyses were conducted using Excel.
Youth engagement
Young people were involved at every stage of this study from inception to dissemination of results. Four youth researchers served as co-leads of the open call organizing committee and analysis working group. The co-leads were compensated with a small honorarium for their time. All youth researchers in the organizing committee were nationals of low- and middle-income countries. The members of the organizing committee helped to publicize the open call through their networks and hosted informational webinar sessions. Youth were also involved as judges of the open call submissions and pitch evaluators. The judges were also compensated with a small honorarium for their time. Two youth researchers analyzed the findings of the open call and wrote up the results.
Results
We received 357 submissions from 37 countries, and 107 submissions were deemed eligible by the judges (Table 1). Of the eligible submissions, 89 (83%) were from the African region, which covers most of the high HIV burden countries identified in the call for submissions. Sixty-two (57%) of the team leads identified as female, whereas 36 (34%) identified as male. Six (6%) participants did not disclose their age, 30 (28%) were aged between 10 and 19 years, and 71 (66%) were aged between 20 and 30 years. Ninety-three (87%) submissions described an implementation platform or location (e.g. digital platform, school etc.) for their intervention. Ninety-one (85%) submissions suggested new ideas for improving adolescent health and well-being, whereas 16 (15%) submissions described ideas that had already been implemented. Twenty (19%) submissions received a mean score of ≥7 out of 10.
| Characteristic of submission | n (%) | |
|---|---|---|
| Submission type | ||
| Individual | 57 (53) | |
| Team | 43 (40) | |
| Not stated | 7 (7) | |
| Age of individual/team lead | ||
| 10–19 years | 30 (28) | |
| 20–30 years | 71 (66) | |
| Not stated | 6 (6) | |
| Region | ||
| Africa | 89 (83) | |
| Asia | 2 (2) | |
| North America | 2 (2) | |
| Europe | 1 (1) | |
| Middle East | 2 (2) | |
| Not stated | 11 (10) | |
| Sex | ||
| Male | 36 (34) | |
| Female | 61 (57) | |
| Not stated/preferred not to say | 10 (9) | |
| Education | ||
| No formal education | 10 (9) | |
| High school | 57 (53) | |
| Bachelor’s degree | 25 (23) | |
| Master’s degree | 5 (5) | |
| Doctoral degree | 3 (3) | |
| Not stated | 7 (7) | |
| Sexual orientation | ||
| Heterosexual | 82 (77) | |
| Bisexual | 7 (6) | |
| Gay or lesbian | 3 (3) | |
| Not stated/preferred not to say | 15 (14) | |
| Submission category | ||
| Digital and social innovations for health | 28 (26) | |
| Digital and social innovations that promote adolescent-centered processes, systems, and policies | 23 (22) | |
| Social and behavioral innovations | 41 (38) | |
| Surprise us | 10 (9) | |
| Not stated | 5 (5) | |
| Intervention locationA | ||
| School | 20 | |
| Health facility | 22 | |
| Social or community venue | 17 | |
| Digital or online | 46 | |
| Other | 15 | |
| Submission score (out of 10) | ||
| ≥7.0e | 20 (19) | |
| <7.0 | 87 (81) | |
Analytic themes from the submissions were organized into three categories: intervention types (Fig. 1), intervention facilitators and intervention barriers. Select quotations describing the intervention types are described in Table 2.
| Intervention type | Themes | Examples of interventions | Areas for youth involvement | |
|---|---|---|---|---|
| Edutainment interventions | Creative/artistic | ‘The [intervention] band is a band for young people both infected and affected with HIV/AIDs (YPLHIV) who believe that they have great talent and potential, and they can use their talents to create a positive impact in the society through edutainment. This band will increase awareness about HIV/AIDs, Reproductive health issues, sexuality, rights, self-awareness and influence policies as well as improving on the livelihoods of YPLHIV through edutainment.’ ‘By engaging young people in artistic and creative events, this can help to break down barriers and promote open and honest discussions about sexual health and rights.’ | – Serving as creative directors – Social media marketing | |
| HIV and health awareness | ‘This digital magazine would serve as a valuable resource, providing information on various aspects of adolescent health, including mental health, contraceptive options, pre-exposure prophylaxis (PrEP),anti-retroviral (ARV) treatment and directories of local services.’ ‘My innovation is focused on increasing awareness of AIDS and demolishing myths and misconceptions spread in the communities about HIV, many people (including me) grew up with false information about the disease. … The innovation will influence religions’ leaders to speak about the disease and causes while breaking the taboo revolving around HIV, because people in these regions tend to be more affected by religious speech than any other speech.’ | – Serving as editors of awareness materials | ||
| Training | ‘[The intervention will] train healthcare professionals and community health workers in adolescent health, mental health support and the use of advanced medical technologies.’ ‘Promoting attitude and behaviour change as well as continuous learning among healthcare workers (HCWs), teachers and parents towards adolescents living with HIV using Massive Open Online Courses (MOOC). The courses will be anchored on adolescent responsive, sensitive and friendly skills.’ | – Developing training materials – Giving feedback | ||
| Peer-based interventions | Peer support | ‘The peers offer peer support and peer counseling in a unique way – blending lived experience and training, and they are supported by specialists for referral, supervision and training.’ | – Being peer counselors – Creating peer referral networks | |
| Peer leadership | ‘Peer-led environments play a vital role in creating comfortable spaces for adolescents. As such, the centers will focus on training adolescents as peer leaders, responsible for overseeing youth-centrerd HIV care systems.’ | – Serving on organizational boards | ||
| Youth-led collaborative networks | ‘By organizing local events and workshops, young people can share their experiences, knowledge and strategies for HIV prevention.’ | – Serving on organizing committees | ||
| Digital interventions | Social media | ‘[The intervention] seeks to reimagine the role of social media platforms as a tool for fostering adherence, empowerment and support for young LGBTQIA individuals living with HIV.’ ‘The innovative solution of launching an SRHR magazine on WhatsApp, coupled with collaboration with local radio stations, community health events and school visits, can effectively promote adolescent health and well-being in rural areas most affected by HIV.’ ‘[The intervention] seeks to reimagine the role of social media platforms as a tool for fostering adherence, empowerment and support for young LGBTQIA individuals living with HIV. Through a dedicated mobile application, [The intervention] will create a safe and inclusive digital space where users can access tailored resources, engage with peers and receive expert guidance on HIV treatment adherence.’ | – Being ‘social media influencers’ for sexual and reproductive health – Content creation | |
| Mobile phone apps and interventions | ‘The app will offer gamified challenges to its users, from which they can receive certificates, awards or tokens. Users who have a sufficient quantity of tokens can exchange them for the Pro version of the app. The app also offers exclusive one-on-one consultations with experienced professionals and experts.’ ‘A fun way to fight HIV stigma is to join gamified events and scholarship. ..You can also earn points and rewards on the virtual platform by learning, getting tested and following treatment plans. This will make you feel proud and motivated to take care of your health.’ ‘Social networking and gaming platforms can discretely provide health education. Features like virtually simulated conversations about condom use negotiations could build skills.’ ‘The use of these [SMS] alerts can be applied to spreading information and awareness, including, but not limited to, climate change, pandemics, pollution and other key global threats.’ | – Spearheading app development Giving feedback on app functions | ||
| Artificial intelligence (AI)/virtual reality (VR)/chatbots | ‘An AI-powered chatbot for adolescents who have been exposed to potential sources of HIV infection: this tool can provide guidance within the short prophylactic period for adolescents exposed to HIV. Unlike the article-based information center, the AI tool can hold a conversation to answer specific user questions and point them in the right direction, drawing on data from the central information center.’ ‘Through virtual reality, viewers can explore the artworks in a dynamic and engaging way, transcending physical limitations and expanding the reach of the exhibition beyond a specific location.’ | – Training artificial intelligence – Serving as end-user testers |
Intervention types
There were three main types of interventions identified through the thematic analysis: edutainment interventions (n = 73), digital interventions (n = 61) and peer-based interventions (n = 32). Some thematic categories overlapped with one another. As such, these three categories describe the primary theme underpinning each intervention.
Seventy-three interventions focused on edutainment interventions to promote HIV awareness and health among young people. Edutainment refers to the combination of education and entertainment to improve adolescent knowledge about sexual and reproductive health (SRH) in an engaging manner. These interventions utilized creative mediums preferred by young people, such as art exhibitions, theater and drama, to deliver sex education and improve uptake of HIV services. Other interventions included digital campaigns about LGBTQIA+ adolescent health and digital graphic magazines to promote self-learning among adolescents. Some edutainment interventions leveraged interactive radio call-in programs and other forms of mass media to engage a wider audience of young people, particularly youth in rural areas. A few interventions focused on training educators and healthcare workers to deliver comprehensive sexuality education through participatory methods. Overall, these interventions aimed to improve knowledge of SRH through engaging mediums that would specifically appeal to young people.
Sixty-one submissions described leveraging digital technology, such as artificial intelligence, chatbots, virtual reality, mobile health apps, telehealth and social media, to promote health and well-being among adolescents. For instance, one submission proposed using open-source artificial intelligence technology to promote access to adolescent-friendly information on HIV, SRH and mental health. Other ideas included developing chatbots to provide adolescents with real-time responses to health-related concerns. For example, a chatbot could provide an in-depth explanation of how to use a condom. Ideas within this theme also included locally-optimized virtual HIV information centers (e.g. websites) providing details on proximate HIV testing services, vetted HIV prevention materials and local sites providing HIV pre-exposure prophylaxis. Other interventions utilized virtual reality for therapeutic experiences aimed at improving mental health. Overall, digital technology was leveraged to increase the reach and utility of HIV interventions while enabling ease of use. To mitigate the digital divide, some interventions described using unstructured supplemental service delivery (USSD) to deliver the same intervention to people without access to the Internet. USSD allows users of mobile phones to access services in real-time by dialing a specific code, which is particularly useful in areas where Internet access is limited.
Thirty-two submissions described using peer-based networks to improve social and emotional well-being among adolescents. These interventions included school-based clubs created to provide a holistic approach to adolescent health and well-being, including mental health support. Ideas within this theme suggested training peer counselors to provide SRH education and psychosocial support, particularly to adolescents living with HIV. These ideas suggested establishing peer-to-peer support networks for decentralized adolescent HIV education, anti-stigma support groups and HIV resource navigation. These interventions additionally enhanced adolescent accountability in pursuing healthy behaviors and seeking care. Other interventions described youth-led collaborative networks where schools and communities unite to organize local events and workshops that support peer-to-peer knowledge sharing. Participatory elements were also mentioned, such as music, spoken word or storytelling. Overall, these ideas focused on enhancing social inclusion for adolescents while promoting health and well-being.
Intervention facilitators
Several intervention facilitators were identified in the thematic analysis. These were characteristics of the submissions (implicit or explicit) that enabled the intervention to deliver the intended outcomes, expand its reach and increase the involvement of participants over time.
Community engagement, which involved the participation and collaboration of community members in problem-solving, emerged as a key intervention facilitator (n = 53). This included establishing learning spaces to share HIV knowledge among community members, as well as the sharing of ideas to combat HIV stigma. Other submissions described organizing community events to raise awareness of HIV services and encourage community involvement in engaging young people to make use of them. Embedding HIV services within the community through temporary testing sites, mobile clinics and counseling tents could increase access to HIV services and reduce stigma. Other submissions described youth-led innovations as an important facilitator of HIV interventions. This occurred through the allure of an intervention being ‘for young people, by young people,’ which increases its attractiveness among communities of young people. At the core of this intervention facilitator was the recognition that social inclusion was important for creating feelings of belonging and importance among young people, which in turn helped to facilitate help-seeking behaviors among them.
Another key facilitator was tailoring interventions to suit young people (n = 42). Tailoring was defined as modifying HIV interventions to center the specific health needs of young people and ensure that they were accessible to any young person who needed them. Almost half of the submissions described tailoring the intervention to be youth-friendly through creating warm, non-judgmental and welcoming spaces for young people. Other submissions described scenarios where young people could directly deliver the intervention themselves or train health workers to deliver the intervention in a youth-friendly manner. A major concern expressed by adolescents was openly seeking HIV care, because it is often associated with stigma. Tailoring interventions to address these concerns was an important facilitator of improved youth involvement in HIV services.
Additionally, several submissions described leveraging collective intelligence to improve the effectiveness of interventions (n = 36). Collective intelligence leverages community wisdom from young people to solve a problem. These approaches included community-led monitoring, open calls, designathons and other crowdsourcing approaches.11,22 Some methods that were employed under this theme included co-creating interventions with young people to ensure that services were appropriate and engaging. We defined co-creation as the intentional collaboration between several stakeholders such that each stakeholder has meaningful ownership over the intervention. Co-created interventions helped to ensure that young people were involved as creators of interventions and not merely recipients. Other submissions described incorporating feedback mechanisms to collect youth opinions for improving the intervention. Digital platforms collected feedback through ratings and user opinions, which were then used to generate data to improve the platform. Overall, collective intelligence emerged as an important mechanism for encouraging participation and retention of adolescents and youth.
Another intervention facilitator that emerged from the analysis was privacy protection (n = 12). This facilitator was particularly important within digital interventions. These ideas included providing adolescents with options to access care and services virtually, such as through telemedicine/telehealth. For those without access to the Internet, options included utilizing USSD or SMS. USSD interventions allowed users to place orders for health products, such as self-testing kits, while protecting their privacy. Other options included anonymously interacting with service providers through SMS. Such modifications helped to facilitate higher engagement with the intervention among adolescents, because adolescents had less fear about their identity or HIV status being revealed to family and friends. This seemed particularly relevant for young people living in areas with high levels of HIV stigma, because they were often concerned about discrimination related to seeking HIV services. Submissions under this theme emphasized prioritizing the privacy of young people to encourage more help-seeking behaviours in relation to HIV services.
Finally, several submissions described methods of incentivizing adolescents to engage with HIV interventions (n = 9). These incentives were mostly financial or material. Such ideas proposed leveraging incentives to influence behavior change and promote the utilization of healthcare services among adolescents. Such (often mobile-based) applications were designed to reward adolescents for using health services and engaging in health promotion activities. For instance, these ideas suggested that for every healthcare visit or participation in SRH educational campaigns, adolescents would receive points on their mobile app that could be redeemed to purchase health and well-being products, as well as other desired items at selected shopping malls or grocery stores. Such gamification techniques were attractive to young people and helped facilitate sustained engagement over time.
Intervention barriers
Submissions to the open call highlighted the challenges faced by adolescents living with HIV and the negative experiences they encountered while seeking health care. These challenges included community stigma; biased treatment from healthcare professionals; cultural, social and religious barriers; and limited access to accurate health information, often worsened by the digital divide. Thirty-eight submissions identified combating stigma as a primary motivation or objective for their intervention. Other submissions expressed concern with either conservative or non-existent access to comprehensive sexuality education by young people, thus limiting their knowledge of essential health information. These barriers, some influenced by cultural and religious factors affecting how sex and sexuality are addressed at home and in school, underscored the need to combat stigma and provide adolescent-centred resources to improve sexual health knowledge and promote the overall well-being of adolescents living with HIV.
Discussion
Our study demonstrates how adolescents and young people in countries with a high burden of HIV can generate creative, feasible, and innovative strategies for improving health and well-being. Our findings indicate that digital interventions, such as USSD and chatbots, are attractive to young people. Integration of these digital approaches with evidence-based interventions may increase adolescent engagement. Moreover, interventions that leverage edutainment and peer-based networks emerged as prominent among young people. Our study expands the literature by presenting perspectives directly from young people in high HIV burden countries, demonstrating strong youth leadership across the entire project, and directly informing the Blueprint Collaborative. Implementation of these interventions will require multi-sectoral investment.
Our data suggest that edutainment interventions improve HIV/SRH awareness among adolescents. These submissions are an indication that young people desire to learn more about SRH and HIV in ways that are engaging to them. Unlike traditional sexuality education programs,23 edutainment interventions incorporate art, drama, music and other creative mediums that are more attractive to young people, and inherently require more active participation in their delivery. Importantly, qualitative data related to sex education programs in high HIV burden countries have been sparse.23 This study provides qualitative evidence of the need for more creative approaches to sex education. Creative mediums, such as art and music, help make important knowledge regarding sexual health more digestible for young people. These mediums also present an opportunity for them to reflect and test their knowledge when communicating it to others; that is, through acting in a play. The young people in our study also view these interventions as potential income-generating activities and opportunities for social empowerment.
Digital interventions emerged as a cross-cutting key theme in the ideas submitted by young people in our study. However, young people also emphasized the importance of exploring solutions that do not rely on the Internet, as there is still a substantial number of households in high HIV burden countries that do not have Internet access. Suggested alternatives included USSD and SMS services accessible on regular mobile phones, which are more accessible in these regions than the Internet.24 In particular, USSD services could be leveraged for increasing access to HIV services and information in remote areas, such as where to find the nearest testing center, which has been effectively used in other settings.25,26 Other interventions that utilized Internet chatbots described making adaptations for USSD-enabled chatbots that could also answer questions in real-time, which would increase the reach of health information to a much wider audience.27
Our data suggest that many adolescents and young people can develop and be engaged in peer-based interventions, especially in school and community settings. This aligns with a substantial evidence-base supporting peer-based HIV interventions.28,29 Young people suggested expanding the reach of these interventions through youth-led collaborative networks that bring various schools and communities together. This could be a powerful way of bridging knowledge gaps between communities, sharing resources and decreasing HIV stigma. Furthermore, young people’s appreciation of the psychosocial and emotional support provided by peer counselors is indicative of the increasing need to focus on mental health in HIV programming. Embedding mental health support in existing peer networks may circumvent the general stigma associated with mental health interventions in certain contexts.30
We also received a few submissions that touched on other themes highlighted in our challenge questions, such as pandemics and climate change, as well as other issues related to sustainability. For instance, some submissions described ways of adapting their existing intervention to be climate-sensitive through limiting single-use materials for HIV campaigns and using digital materials wherever possible. Other interventions explored questions of long-term sustainability of interventions, and described exploring financing mechanisms through grants and donations, whereas others described collaborations with government institutions to expand the reach and longevity of their interventions. These submissions demonstrated that young people were cognizant and concerned about larger contextual factors that relate to program success and sustainability of HIV interventions addressing adolescent health and well-being.
There were some limitations of this study that may offer directions for future research. First, only 28% of eligible submissions were from adolescents alone (although adolescents may have been part of a team). Nonetheless, many young people (aged 20–30 years) have important insights about the adolescent experience, especially those who are only a few years removed from this phase of life. Further research may benefit from incorporating approaches to encourage more adolescent involvement in research, such as having adolescent ambassadors involved in research planning and execution. Second, we used online methods to solicit ideas, and this excluded a large number of adolescents without online access. We mitigated this risk by encouraging adolescents to share the open call through in-person networks to reach more people who may not have access to the Internet. We encouraged team-based submissions to enhance collaboration between participants of various backgrounds, particularly those with and without the Internet, and those above and at the adolescent age.
The findings of our study have a few important implications for HIV research and policy. First, our study captures young people’s experiences, needs and concerns related to HIV programming, which indicate gaps for more focused research and policymaking. For instance, there is a need to prioritize adolescent privacy in HIV services and programs to encourage greater participation from adolescents, particularly in high-stigma communities. Although some of the interventions submitted to the open call have been previously implemented in various HIV responses (such as sex education and peer counseling), their re-emergence in our open call demonstrates the need to constantly improve and tailor these existing interventions to specific populations and contexts. Young people brought forth innovative ways that can be used to make these interventions work better for adolescents, such as using more creative and accessible mediums to enhance SRH learning, and expanding digital interventions to rural participants through USSD. Overall, our study demonstrates the need for greater youth engagement in the creation of adolescent health programs and policies to ensure improved outcomes.
Conclusion
Overall, our study garnered substantive engagement from young people around the world, particularly those in high HIV burden countries. Submissions to our open call offered several ideas on how adolescent health and well-being can be re-imagined to better suit the needs of young people. These ideas highlighted adolescents’ appreciation of innovations, such as USSD, artificial intelligence, collective intelligence and incentivization, as emerging opportunities with programmatic import. Many of the young people’s ideas identified in this open call could directly be integrated into research and policymaking for adolescent health improvement.
Conflicts of interest
Joseph Tucker is a co-Editor-in-Chief for Sexual Health, but was not involved in the peer review or decision-making process for this paper. The authors declare no conflicts of interest. The content is solely the responsibility of the authors, and does not necessarily represent the official views of the US Department of Health and Human Services and the National Institutes of Health.
Declaration of funding
UNICEF, the Adolescent HIV Prevention and Treatment Implementation Science Alliance, and the US National Institute of Health (NIAID K24AI143471, 1UG1HD113156).
Author contributions
DW, EM and JT conceived the study, and provided overall guidance and supervision. TH and IO drafted the original manuscript. Subsequent revisions and editing were conducted by JT, DW, KC, YZ, JI, OA, DH, IO, SV, RS, OE and TH. Data curation was conducted by IO. The formal analysis was conducted by TH and YZ. Project administration duties were shared among IO, CU, BA, KC, TH and YT. Funding for the study was acquired by JT. All authors revised and approved the manuscript for submission.
Acknowledgements
We are grateful for the support of the Special Programme for Research and Training in Tropical Diseases, 4YBY, and Social Entrepreneurship to Spur Health in the organization and dissemination of the open call. We are also grateful to Donald Waruhanga, Doreen Moraa, Guncha Annageldiyeva, Mengmeng Jia, Munnira Katongole, Nyasha Phanisha Sithole, Ucheoma Nwaozuru, Safaa Garelnabi, Sharaf Boborakhimov, Sophie Arseneault, Tinashe Tufurwadvo and Cindy Amazia for serving as the global jury for the open call. We are additionally thankful to Misheck Zulu for summarizing this work in a visual abstract. We also thank the larger UNICEF/WHO/UNAIDS Blueprint Collaborative for bringing together a youth-led group to spearhead this work. Finally, we specially thank all the participants of the open call for their participation.
References
1 Benevides R, Logan J, Patel P. Introduction to the youth HIV prevention supplement. AIDS Educ Prev 2023; 35(Supplement A): 1-3.
| Crossref | Google Scholar |
2 Enane LA, Davies M-A, Leroy V, et al. Traversing the cascade: urgent research priorities for implementing the ‘treat all’ strategy for children and adolescents living with HIV in sub-Saharan Africa. J Virus Erad 2018; 4(Supp 2): 40-6.
| Crossref | Google Scholar | PubMed |
3 UNICEF. Prospects for children in the polycrisis: a 2023 global outlook. United Nations Children’s Fund; 2023. Available at https://www.unicef.org/globalinsight/media/3001/file/UNICEF-Innocenti-Prospects-for-Children-Global-Outlook-2023.pdf
5 UNICEF. Humanitarian action for children 2017. United Nations Children’s Fund; 2017. Available at https://www.unicef.org/reports/humanitarian-action-children-2017-overview
6 WHO. Global accelerated action for the health of adolescents (AA-HA!) – second edition. 2023. Available at https://www.who.int/publications/i/item/9789240081765
8 World Health Organization. WHO youth engagement. 2023. Available at https://www.who.int/initiatives/who-youth-engagement#:~:text=Engaging%20young%20people%20in%20global,to%20join%20a%20youth%20organization
9 Wilson O. A rapid evidence review of young people’s involvement in health research. London: Wellcome; 2020. Available at https://cms.wellcome.org/sites/default/files/2021-02/a-rapid-evidence-review-of-young-peoples-involvement-in-health-research.pdf
10 Asuquo SE, Tahlil KM, Muessig KE, et al. Youth engagement in HIV prevention intervention research in sub-Saharan Africa: a scoping review. J Int AIDS Soc 2021; 24(2): e25666.
| Crossref | Google Scholar | PubMed |
12 Wang C, Han L, Stein G, et al. Crowdsourcing in health and medical research: a systematic review. Infect Dis Poverty 2020; 9(1): 8.
| Crossref | Google Scholar | PubMed |
13 Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health 2006; 60(10): 854-7.
| Crossref | Google Scholar | PubMed |
15 Vaughan C, Zayas J, Devine A, et al. W-DARE: a three-year program of participatory action research to improve the sexual and reproductive health of women with disabilities in the Philippines. BMC Public Health 2015; 15: 984.
| Crossref | Google Scholar | PubMed |
16 Dang MT, Amos A, Dangerfield M, et al. A youth participatory project to address STIs and HIV among homeless youth. Compr Child Adolesc Nurs 2019; 42(3): 222-40.
| Crossref | Google Scholar | PubMed |
17 Pavkov TW, Priest J, Fox K. Use of cognitive question testing methodologies in participant action research: implementing the three-step test-interview method in Indian county. Cultur Divers Ethnic Minor Psychol 2012; 18(1): 82-90.
| Crossref | Google Scholar | PubMed |
18 Frost DM, Fine M, Torre ME, et al. Minority stress, activism, and health in the context of economic precarity: results from a national participatory action survey of lesbian, gay, bisexual, transgender, queer, and gender non-conforming youth. Am J Community Psychol 2019; 63(3–4): 511-26.
| Crossref | Google Scholar | PubMed |
19 Murphy BP, O’Raghallaigh P, Carr M. Nurturing the digital baby: open innovation for development and optimization. Health Informatics J 2020; 26(4): 2407-21.
| Crossref | Google Scholar | PubMed |
20 Tao Y, Byrne M, Ho D, et al. HIV interventions across the care continuum for adolescents in high-burden countries: a systematic review and meta-analysis. EClinicalMedicine 2024; 78: 102989.
| Crossref | Google Scholar |
21 Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45.
| Crossref | Google Scholar | PubMed |
22 UNDP. Collective intelligence for sustainable development. Getting smarter together. United Nations Development Programme; 2021. Available at https://smartertogether.earth/download-report.
24 Oladele DA, Iwelunmor J, Gbajabiamila T, et al. An unstructured supplementary service data system to verify HIV self-testing among nigerian youths: mixed methods analysis of usability and feasibility. JMIR Form Res 2023; 7: e44402.
| Crossref | Google Scholar |
25 Macharia P, Pérez-Navarro A, Inwani I, et al. An exploratory study of current sources of adolescent sexual and reproductive health information in kenya and their limitations: are mobile phone technologies the answer? Int J Sex Health 2021; 33(3): 357-70.
| Crossref | Google Scholar | PubMed |
26 Tucker JD, Hocking J, Oladele D, et al. Digital sexually transmitted infection and HIV services across prevention and care continuums: evidence and practical resources. Sex Health 2022; 19(4): 278-85.
| Crossref | Google Scholar | PubMed |
27 Chibi M, Wasswa W, Ngongoni CN, et al. Scaling up delivery of HIV services in Africa through harnessing trends across global emerging innovations. Front Health Serv 2023; 3: 1198008.
| Crossref | Google Scholar |
28 Simoni JM, Nelson KM, Franks JC, et al. Are peer interventions for HIV efficacious? A systematic review. AIDS Behav 2011; 15(8): 1589-95.
| Crossref | Google Scholar | PubMed |
29 Tobin KE, Heidari O, Winiker A, et al. Peer approaches to improve HIV care cascade outcomes: a scoping review focused on peer behavioral mechanisms. Curr HIV/AIDS Rep 2022; 19(4): 251-64.
| Crossref | Google Scholar | PubMed |
30 Javed A, Lee C, Zakaria H, et al. Reducing the stigma of mental health disorders with a focus on low- and middle-income countries. Asian J Psychiatr 2021; 58: 102601.
| Crossref | Google Scholar | PubMed |