Effects of wearing textured versus smooth shoe insoles for 12 weeks on gait, foot sensation and patient-reported outcomes, in people with multiple sclerosis: a randomised controlled trial
Anna L. Hatton A * , Katrina Williams A , Mark D. Chatfield B , Sheree Hurn C , Jayishni N. Maharaj D , Elise M. Gane A , Thomas Cattagni E , John Dixon F , Keith Rome G , Graham Kerr H and Sandra G. Brauer AA School of Health and Rehabilitation Sciences,
B Centre for Health Sciences Research,
C School of Clinical Sciences,
D School of Allied Health Sciences,
E Laboratory Movement, Interactions, Performance EA 4334,
F School of Health & Social Care,
G School of Clinical Sciences,
H Institute of Health and Biomedical Innovation,
Abstract
Innovative shoe insoles, designed to enhance sensory information on the plantar surface of the feet, could help to improve walking in people with Multiple Sclerosis.
To compare the effects of wearing textured versus smooth insoles, on measures of gait, foot sensation and patient-reported outcomes, in people with Multiple Sclerosis.
A prospective, randomised controlled trial was conducted with concealed allocation, assessor blinding and intention-to-treat analysis. Thirty ambulant men and women with multiple sclerosis (MS) (Disease Steps rating 1–4) were randomly allocated to wear textured or smooth insoles for 12 weeks. Self-reported insole wear and falls diaries were completed over the intervention period. Laboratory assessments of spatiotemporal gait patterns, foot sensation and proprioception, and patient-reported outcomes, were performed at Weeks 0 (Baseline 1), 4 (Baseline 2) and 16 (Post-Intervention). The primary outcome was the size of the mediolateral base of support (stride/step width) when walking over even and uneven surfaces. Independent t-tests were performed on change from baseline (average of baseline measures) to post-intervention.
There were no differences in stride width between groups, when walking over the even or uneven surfaces (P ≥ 0.20) at post-intervention. There were no between-group differences for any secondary outcomes including gait (all P values > 0.23), foot sensory function (all P values ≥ 0.08) and patient-reported outcomes (all P values ≥ 0.23).
In our small trial, prolonged wear of textured insoles did not appear to alter walking or foot sensation in people with MS who have limited foot sensory loss. Further investigation is needed to explore optimal insole design.
Australian and New Zealand Clinical Trials Registry (ACTRN12615000421538).
Keywords: Gait, orthotic devices, multiple sclerosis, foot sensation, proprioception.
Introduction
Gait problems are a core feature of multiple sclerosis (MS), with 85% of patients reporting gait disturbances as their main complaint (Scheinberg, Holland & LaRocca, 1980) and 60% reporting falls in any 3-month period (Nilsagård et al., 2015). Half of these falls result in injuries (Matsuda et al., 2011), 23% of which require medical attention (Peterson, Cho, von Koch & Finlayson, 2008) that contribute to escalating health care costs. Impaired mobility is a major risk factor for falls in people with MS (pwMS) (Finlayson, Peterson & Cho, 2006), who typically walk with a reduced stride/step length, velocity and increased mediolateral (ML) base of support and double-limb support time, relative to age-matched healthy adults (Givon, Zeilig & Achiron, 2009; Kalron, Dvir & Achiron, 2010; Martin et al., 2006). Altered spatiotemporal gait patterns in pwMS are indicative of compromised stability and can be exacerbated by concomitant sensory deficits, such as reduced foot sensation (Rougier, Thoumie, Cantalloube & Lamotte, 2007). Existing interventions reported to improve gait in pwMS involve short-term exercise programmes and largely address motor deficits (Davies et al., 2016; DeBolt & McCubbin, 2004; Garrett et al., 2013; Learmonth, Paul, Miller, Mattison & McFadyen, 2012; Pearson, Dieberg & Smart, 2015). However, the benefits of structured exercise on walking ability appear to be short-lived (Wiles et al., 2001). New treatments to complement exercise by addressing MS sensory deficits are needed to achieve longer-term gains in activity, participation and independent living (Khan & Amatya, 2017).
Novel shoe insoles, designed to provide sensory input to the feet using textured materials, have been investigated as a new technique to optimise gait in healthy young (Collings, Paton, Chockalingam, Gorst & Marsden, 2015; Nurse, Hulliger, Wakeling, Nigg & Stefanyshyn, 2005) and older (Perry, Radtke, McIlroy, Fernie & Maki, 2008) adults, fallers (Hatton, Dixon, Rome, Newton & Martin, 2012), stroke survivors (Aries, Pomeroy, Sim, Read & Hunter, 2021; Aruin & Rao, 2018; Ma, Rao, Muthukrishnan & Aruin, 2018), neurodegenerative (Jenkins et al., 2009; Lirani-Silva et al., 2017) and neuromuscular (Baron et al., 2016b; Dixon et al., 2014; Kalron, Pasitselsky, Greenberg-Abrahami & Achiron, 2015; Kelleher, Spence, Solomonidis & Apatsidis, 2010) disease populations. Evidence suggests that tactile stimulation of cutaneous receptors on the plantar surface of the foot can provide the brain with ‘amplified’ cues about the supporting surface, position and acceleration of the body, to inform balance and movement control (Roll, Kavounoudias & Roll, 2002; Viseux et al., 2019). Indeed, recent evidence in healthy and athletic populations support the theory that textured insoles can enhance lower limb sensory feedback to augment dynamic movement control (Hasan, Davids, Chow & Kerr, 2017; Jamali, Forghany, Bapirzadeh & Nester, 2019; Steinberg et al., 2016; Wilkinson et al., 2018). Similar effects of textured insoles could also occur in neurological disease populations, including pwMS, and underpin improvements in gait performance.
Exploratory studies have shown that textured insoles may have potential to improve spatiotemporal gait measures (Dixon et al., 2014), gait kinetics and kinematics (Kelleher et al., 2010), self-perceived walking ability (Baron et al., 2016a) and lower limb proprioception (Baron et al., 2014), in pwMS. A pilot randomised controlled trial in pwMS demonstrated that short-term wear (2 weeks) of textured insoles led to increased stride and step length, and reduced ML base of support, during level-ground walking (Dixon et al., 2014). Importantly, improvements in gait were observed when the textured insoles were not in situ, pointing to a possible sensory learning effect (Dixon et al., 2014). However, further work in pwMS has reported no significant changes in spatiotemporal gait measures during treadmill walking, or foot sensation, after wearing textured insoles for 4 weeks (Kalron et al., 2015). To date, studies exploring textured insoles for pwMS have been limited to the evaluation of level-ground walking; overlooking irregular, uneven terrain encountered in everyday life that can perturb balance to a greater extent and which may provide valuable insight into any insole effects under conditions where falls commonly occur (Hollander, Petersen, Zech & Hamacher, 2022; Menant, Steele, Menz, Munro & Lord, 2009). Furthermore, few studies report the effects of long-term wear of textured insoles on gait in pwMS. This is a critical area to research, as the benefits of textured insoles may accrue (or decline) with prolonged wear, allowing pwMS sufficient time to become familiar with (or habituate to) a new source of sensory stimuli.
Innovative thinking towards the therapeutic capabilities of shoe insoles for pwMS (e.g., providing substitute plantar sensory input) challenges the traditional physiological basis for insole/orthotic prescription in neurological diseases, which has centred on the management of neuromotor control during walking (Young & Moss, 2019). Recent evidence suggests that textured insoles may also influence perceptual aspects of movement control in MS, which manifest as greater walking confidence and awareness of foot position (Baron et al., 2016a; Baron et al., 2014). Whilst textured insoles can improve objective (and self-reported) measures of gait in pwMS, we do not understand their underlying mechanisms. Only one study in pwMS has explored the effect of textured insoles on measures of foot sensation, reporting no significant change in light-touch pressure sense (Kalron et al., 2015). However, alterations may occur in other dimensions of sensory function, such as vibration perception, spatial discrimination, or joint proprioception.
Therefore, the objective of this study was to determine whether wearing textured insoles for 12 weeks can improve spatiotemporal gait patterns and foot sensory function in pwMS. The primary aim was to explore if prolonged wear of textured insoles alters the size of the ML base of support (a measure of gait stability) in pwMS, when walking over even and uneven surfaces – relative to smooth (control) insoles. We hypothesised that wearing textured insoles for 12 weeks would lead to reductions in stride/step width during walking. Secondary aims were to investigate if prolonged wear of textured insoles alters other gait measures (stride time, double-limb support time, stride length and velocity), foot sensory function (light-touch, vibration, two-point discrimination and joint position sense) and patient-reported outcomes (walking ability, MS symptoms, falls, quality of life). We hypothesised that wearing textured insoles would decrease stride time and double support time and increase stride length and velocity and lead to improvements in foot sensory function and patient-reported outcomes.
Methods
Design
A prospective, parallel group, single-blinded, randomised controlled trial of pwMS was conducted. Recruitment occurred from March 2016 to November 2017; and post-intervention assessments until March 2018. Ethical approval was obtained from The University of Queensland (#2014000871) and Queensland University of Technology (#1500000615) Human Research Ethics Committees. All participants provided written informed consent. The trial was conducted in accordance with the Declaration of Helsinki, conformed to the Consolidated Standards of Reporting Trials guidelines (Schulz, Aman & Moher, 2010) and was registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12615000421538). The methods employed are described within the published protocol (Hatton et al., 2016).
Sample size
A priori calculation was performed to determine sample size; following publication of protocol, the sample size calculation was updated resulting in a slightly smaller sample size. Based on preliminary work in pwMS (Dixon et al., 2014), a mean (SD) reduction of 1.7 (3.0) cm in ML base of support during level-ground walking, after wearing textured insoles for 2 weeks, was estimated. With a power of 90% to detect a difference between groups of 1.7 cm, significance of 0.05 and accounting for a 15% dropout rate, 83 participants were required per group.
Participants
Men and women with MS were recruited via volunteer databases maintained at The University of Queensland and MS Queensland, and through advertisements to local MS health care providers and support groups, across South East Queensland, Australia. Participants were eligible to take part if they met the following criteria: aged ≥18 years; diagnosis of MS; ambulant over 100 m (with/without use of an assistive device); and Disease Step rating 1–4 (clinician-rated) (Hohol, Orav & Weiner, 1995). Exclusion criteria were: neurological disease other than MS; peripheral neuropathy; current use of foot insoles/orthoses; cardiovascular or orthopaedic conditions that limit ambulation; unstable psychiatric condition or cognitive impairment (Short Form Mini Mental State Examination score < 24; Folstein, Folstein & McHugh, 1975)). Participants who experienced an exacerbation of MS symptoms (persisting >24 h), 4 weeks prior to, or during, the intervention period were excluded. Volunteers were screened for eligibility by telephone and thereafter invited to attend a clinical examination (conducted by a physiotherapist, KW), which involved the assessment of disease stage (Disease Steps; Hohol et al., 1995), spasticity (Tardieu Scale; Tardieu, Shentoub & Delarue, 1954), ataxia (Brief Ataxia Rating Scale; Schmahmann, Gardner, MacMore & Vangel, 2009) and foot sensation (ability to detect a Semmes–Weinstein 10 g monofilament at ≥4 sites/ft; Armstrong, Lavery, Vela, Quebedeaux & Fleischli, 1998).
Intervention
Both groups continued to receive their usual care during the study; participants were asked to notify the investigators of any change to their usual care during their involvement in the study. The intervention group was fitted with a pair of textured insoles (Evalite Pyramid ethyl vinyl acetate, 3 mm thick, Shore A50; Algeos, VIC, Australia) comprising raised pyramidal peaks (2.5 mm peak-to-peak distances) (Fig. 1). The control group received a pair of smooth insoles (medium-density ethyl vinyl acetate, 3 mm thick, Shore A50; Algeos, VIC, Australia), comprising a flat surface (Fig 1). Insoles were tailored to each individuals’ shoe size and fitted by a podiatrist (SH, JNM), who also provided advice on frequency of wear, completion of insole wear (to monitor hours of insole wear per day) and falls diaries and contact details for podiatry care. Over the 12-week intervention period, participants were instructed to wear their allocated insoles in their own shoes, as much as possible (when indoors and outdoors), and to gradually increase wear time after first being issued the insoles. During laboratory gait tests, the insoles were worn in standard shoes (Volley International Canvas, Volley, China), to control for any confounding shoe/insole interactions. Upon wearing the shoes for the first time, participants walked for 5-min to allow for familiarisation.
Randomization and blinding
The computer-generated randomisation schedule was maintained by an independent investigator. Participants were randomly allocated to one of two groups (Textured insoles; Smooth insoles), using permuted blocks of 4 (1:1 ratio). Consecutively numbered, opaque envelopes containing group allocation were opened after Baseline 2 assessment by the study podiatrists who were only responsible for issuing the insoles. All other investigators involved in participant enrolment and assessments were blinded to group allocation. Participants could not be blinded to their group, as those allocated to the intervention would likely perceive the textured material under their feet. The full study aims were concealed from participants until debriefing, upon completion of the study.
Laboratory assessments
Participants attended three assessments (2–3 h/assessment) within the Gait Laboratory at Queensland University of Technology: Baseline 1 (Week 0); Baseline 2 (Week 4); Post-Intervention (Week 16). Two baseline assessments were conducted to establish participants’ usual rate of disease progression over a 4-week period, prior to issuing the insoles upon completion of Baseline 2.
Baseline 1
Demographic details were collected including age, gender, body mass. Participants completed questionnaires addressing medical history, MS diagnosis and symptoms (MS Impact Scale; Hobart, Lamping, Fitzpatrick, Riazi & Thompson, 2001), and perceived walking ability (MS Walking Scale; Hobart, Riazi, Lamping, Fitzpatrick & Thompson, 2003). Self-report questionnaires were used to assess quality of life (MS Quality of Life Instrument; Vickrey, Hays, Harooni, Myers & Ellison, 1995), the impact of fatigue (Modified Fatigue Impact Scale; Fisk et al., 1992) and pain (Medical Outcomes Study Pain Effects Scale; Archibald et al., 1994), perceived disability (Perceived Deficits Questionnaire; Sullivan, Edgley & Dehoux, 1990) and fear of falling (Falls Efficacy Scale-International; Yardley et al., 2005). Participants also reported the number of falls experienced in the previous 12 months.
Foot sensory function was assessed bilaterally, as described in the study protocol (Hatton et al., 2016). Light-touch pressure sense was measured using Semmes–Weinstein monofilaments (1.65–6.65 gauges), applied to the great toe, first and fifth metatarsal heads, heel and dorsum of the foot (Citaker et al., 2011; Hatton et al., 2016). Vibration sense was measured using a 128-Hz tuning fork applied to the first metatarsal head and medial malleoli (Citaker et al., 2011; Hatton et al., 2016). The two-point discrimination test was performed using an aesthesiometer, to determine tactile spatial acuity at the great toe, first to second metatarsal interspace and fifth metatarsal head (Citaker et al., 2011; Hatton et al., 2016). Proprioception was assessed via the ankle joint angle reproduction test (Riskowski, Mikesky, Bahamonde, Alvey & Burr, 2005), with an internet-based goniometer used to measure accuracy in joint positioning (Russell, Jull & Wootton, 2003).
Gait was assessed whilst walking at a comfortable, self-selected pace over a 12 m even and uneven surface. The even surface comprised the vinyl top cover of a GaitRite® walkway (CIR Systems Inc., Havertown, USA). The uneven surface, designed to simulate outdoor terrain, was created from layers of foam, wood blocks and artificial grass (Menant et al., 2009). Start and finish lines were taped two metres in front and behind the walkways to allow for acceleration and deceleration (Batey, Rome, Finch & Hanchard, 2003). PwMS completed five walking trials (or as many trials as tolerated) along the even and uneven surfaces, under four different footwear conditions: (i) barefoot, (ii) standard shoes only, (iii) textured insoles and (iv) smooth insoles (order randomised). Prior to testing, reflective markers were attached to participants (Vicon Plug-In-Gait full body model). Spatiotemporal gait patterns were measured using the GaitRite® (sampling rate 80 Hz) during even surface walking trials, and an 11-camera Vicon® system (sampled at 200 Hz), for the uneven surface walking trials. It was not possible to collect data using Vicon®, for both surfaces, due to the size of the camera capture area, relative to the layout of the walkways within the laboratory.
Upon completion of Baseline 1, a wireless activity monitor (ActivPALTM, Glasgow, Scotland), was fitted to each participant’s right thigh using adhesive tape. The monitor was worn for seven consecutive days to characterise participants’ habitual activity levels (total number of steps, counts/day; total time spent sitting, standing, walking, h/day) (Edwardson et al., 2017).
Baseline 2
Four weeks after their initial assessment, participants returned to the laboratory to perform tests of foot sensory function and gait, as per Baseline 1. This waiting period enabled observation of participants’ natural rate of MS disease progression, and any changes in the outcome measures, prior to issuing the intervention. Participants’ allocated insoles were fitted by the podiatrist at the end of the Baseline 2 assessment (the investigators left the laboratory to ensure assessor blinding).
Post-intervention
Participants completed a final assessment of foot sensory function and gait, after wearing their allocated insoles for 12 weeks. Questionnaires completed at Baseline 1 were re-administered for a second time. Participants also rated how comfortable their insoles were to wear using a 100 mm visual analogue scale (VAS, 0 = extremely uncomfortable; 100 = extremely comfortable) (Mills, Blanch & Vicenzino, 2010). Insole wear (Supplementary Material 1) and falls (Supplementary Material 2) diaries, completed over the 12-week intervention period, were returned at this time.
Outcome measures
The primary outcome was the change in size of the ML base of support, when walking over the even and uneven surface, with a reduction in stride/step width interpreted to indicate greater stability. Secondary spatiotemporal gait measures included stride time, double-limb support time, stride length and gait velocity. Secondary foot sensation and proprioception measures were light-touch pressure sense (smallest monofilament perceived ≥2/3 applications, at each of the five foot sites) (Citaker et al., 2011; Hatton et al., 2016), vibration sense (duration of vibration, seconds) (Citaker et al., 2011; Hatton et al., 2016), two-point discrimination (smallest distance perceived, mm) (Citaker et al., 2011; Hatton et al., 2016) and ankle joint position sense (accuracy in joint angle re-positioning, degrees error) (Riskowski et al., 2005). Secondary patient-reported outcomes included the MS Impact Scale (Hobart et al., 2001), MS Walking Scale (Hobart et al., 2003), MS Quality of Life Instrument (Vickrey et al., 1995), Modified Fatigue Impact Scale (Fisk et al., 1992), Medical Outcomes Study Pain Effects Scale (Archibald et al., 1994), Perceived Deficits Questionnaire (Sullivan et al., 1990) and Falls Efficacy Scale-International (Yardley et al., 2005).
Data analysis
Statistical analyses were performed in a blinded manner, on an intention-to-treat basis, using Stata 16.0 (StataCorp. 2019). Data were assessed for normality. Outcomes that were skewed, were transformed onto the 100 log(e) scale, to enable reporting of symmetric percentage differences (Cole, 2000). Gait and foot sensory measures were averaged across the left and right leg/foot. To determine any between-group differences in outcomes, independent t-tests were performed on change from baseline (average of Baseline 1 and Baseline 2 measures) to post-intervention. The alpha level was 0.05, with no adjustments for multiple testing.
Results
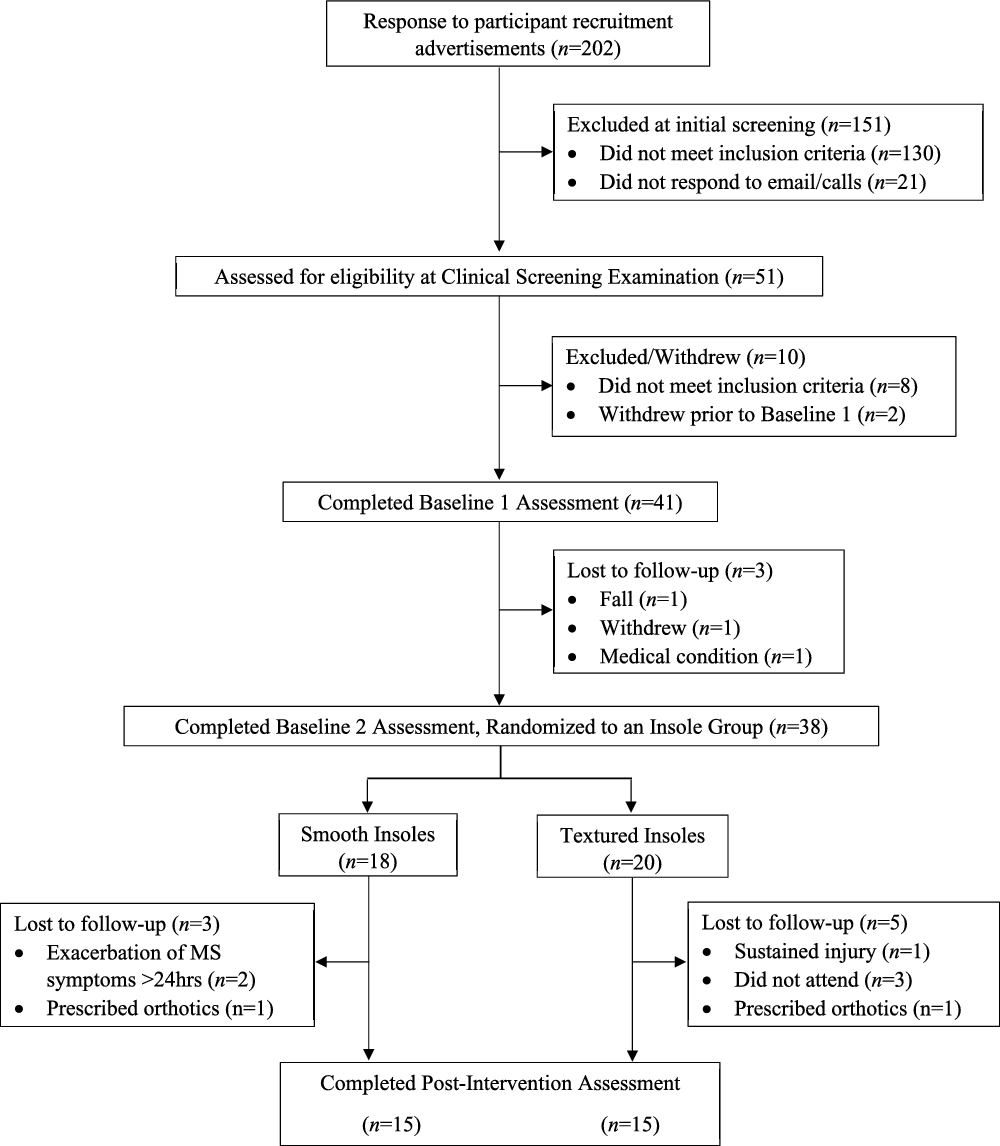
A total of 202 pwMS were screened for eligibility. Of these, 51 pwMS underwent a clinical examination, and 41 pwMS were enrolled into the study and completed Baseline 1 assessment (Fig. 2). Recruitment ceased prior to reaching the estimated sample size (n = 166), and before any data analysis had taken place, due to the exhaustion of funding and resources. Eighteen pwMS were allocated to the smooth insole group and 20 pwMS to the textured insole group. The attrition rate was 7% at 4 weeks and 27% at 16 weeks. Thirty participants successfully completed the trial (Control group, N = 15; Intervention group, N = 15). Baseline demographic and clinical characteristics were similar between groups (Table 1).
Demographics and Clinical Characteristics for Participants Who Were Allocated to the Control Group (Smooth Insoles) and Intervention (Textured Insoles) Group and Successfully Completed the Trial
| Characteristic | Control Group (N = 15) | Intervention Group (N = 15) | |
|---|---|---|---|
| Age, years | 49 (9) | 51 (10) | |
| Female | 13 (87%) | 11 (73%) | |
| Weight, kg | 81 (22) | 77 (19) | |
| Height, m | 1.65 (0.09) | 1.69 (0.08) | |
| Body mass index, kg/m2 | 30 (7) | 27 (5) | |
| Type of Multiple Sclerosis | |||
| Relapsing remitting | 14 (93%) | 12 (80%) | |
| Primary progressive | 0 (0%) | 3 (20%) | |
| Secondary progressive | 1 (7%) | 0 (0%) | |
| Years since Multiple Sclerosis diagnosis | 11 (8) | 10 (9) | |
| Disease Steps (clinician-rated) | |||
| 1 – Mild disability | 5 (34%) | 2 (14%) | |
| 2 – Moderate disability | 6 (40%) | 3 (33%) | |
| 3 – Early cane | 2 (13%) | 8 (53%) | |
| 4 – Late cane | 2 (13%) | 0 (0%) | |
| Disease Steps (patient-rated) | |||
| 0 – Normal | 1 (7%) | 2 (13%) | |
| 1 – Mild disability | 7 (47%) | 1 (7%) | |
| 2 – Moderate disability | 3 (20%) | 1 (7%) | |
| 3 – Early cane | 2 (13%) | 6 (40%) | |
| 4 – Late cane | 1 (7%) | 5 (33%) | |
| 5 – Bilateral support | 1 (7%) | 0 (0%) | |
| Expanded disability status scale | 2.50 (1.50–3.50) | 2.50 (2.00–3.00) | |
| Brief Ataxia Rating Scale | 3.0 (0.0–10.0) | 3.0 (1.0–7.0) | |
| Mini Mental State Examination | 29.5 (0.8) | 29.4 (0.9) | |
| Number of medications | |||
| 0 | 1 (7%) | 2 (13%) | |
| 1 | 3 (20%) | 6 (40%) | |
| ≥2 | 11 (73%) | 7 (47%) | |
| Types of medications | |||
| Multiple sclerosis | 12 (80%) | 10 (67%) | |
| Pain (e.g., anti-inflammatory, opioid) | 2 (13%) | 2 (13%) | |
| Cardiovascular (e.g., anti-hypertensive) | 4 (27%) | 1 (7%) | |
| Cholesterol | 3 (20%) | 0 (0%) | |
| Psychological (e.g., anti-depressant) | 10 (67%) | 3 (20%) | |
| Incontinence | 1 (7%) | 1 (7%) | |
| Other | 11 (73%) | 15 (100%) | |
| Number of falls in previous 12 months | |||
| 0 | 6 (40%) | 6 (40%) | |
| 1 | 4 (27%) | 2 (13%) | |
| ≥2 | 5 (33%) | 7 (47%) | |
| Habitual physical activity (average of 7 days) a | |||
| Total number of steps, count/day | 5247 (2905) | 5403 (2343) | |
| Total time spent sitting, h/day | 18.7 (1.8) | 16.8 (4.0) | |
| Total time spent standing, h/day | 3.2 (1.5) | 3.3 (1.1) | |
| Total time spent walking, h/day | 1.3 (0.6) | 2.6 (4.4) | |
Insole adherence and comfort
Participants in both groups reported wearing their insole for a similar number of (mean ± SD) hours/day over the intervention period (Smooth insole: 5.5 ± 3.5 h/day; Textured insole: 6.4 ± 3.0 h/day; P = 0.47). Perceived comfort when wearing the insoles (VAS, mean ± SD) did not significantly differ between groups (Smooth insole: 64 ± 32; Textured insole: 77 ± 27; P = 0.25).
Adverse events
Over the intervention period, five pwMS (18%) reported a non-injurious fall. Of these, four participants (29%) were in the control group, and one participant (7%) was in the intervention group. The rate of falls did not significantly differ between the groups (P = 0.33). PwMS who experienced a fall during the trial were known to be recurrent fallers and, therefore, wearing the insoles did not increase their usual rate of falls. The insole wear diaries indicated that foot pain and discomfort were experienced by some participants in the smooth (N = 7, 47%) and textured (N = 5, 36%) insole groups, but this was not significantly different (P = 0.71). Nine participants noted minor skin irritation to the soles of their feet, whilst wearing the smooth (N = 2, 13%) and textured (N = 7, 47%) insoles (P = 0.11).
Primary outcome measure
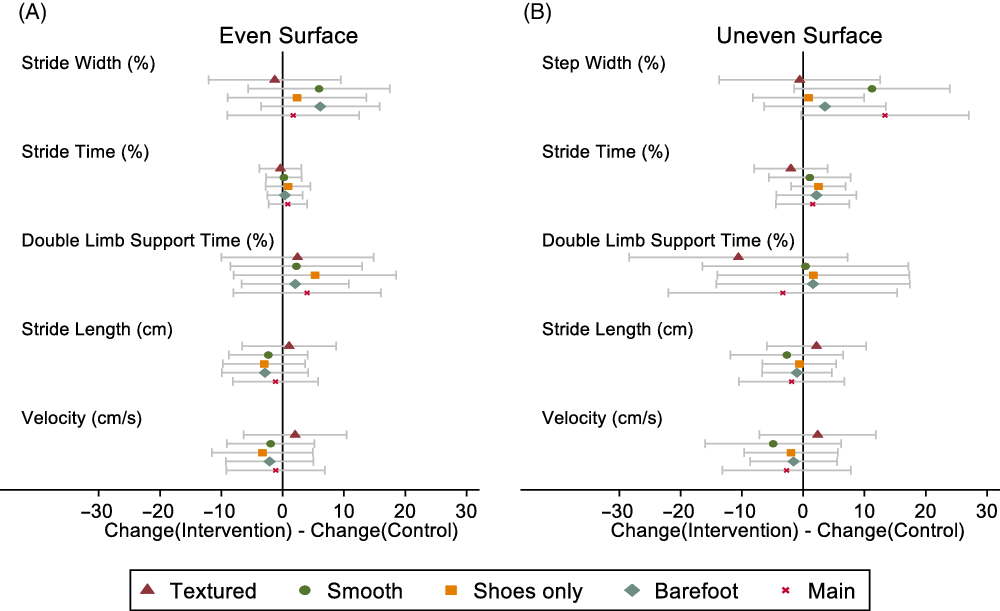
At post-intervention, there were no significant between-group differences in change in stride width, when walking over the even surface (all P values ≥ 0.20) in each of the four footwear conditions (Fig. 3 and Table 2).
Effect of intervention (versus control) with 95% confidence interval for change in Stride Length and Velocity, and symmetric percentage change in Stride/Step Width, Stride Time, and Double-Limb Support Time, when walking over even (A) and uneven (B) surfaces. ‘Main’ denotes a comparison between baseline gait assessments completed in the ‘Shoes only’ condition (i.e., no insoles), and post-intervention gait assessments performed with participants wearing the insoles allocated to them over the intervention period (i.e., textured insole gait assessments for the intervention group; smooth insole gait assessments for the control group).
Changes in Spatiotemporal Gait Measures (Averaged Across Right/Left Legs) from Baseline to Post-Intervention for the Control (Smooth Insole) and Intervention (Textured Insole) Groups, When Walking Over Even and Uneven Surfaces in Four Footwear Conditions
| Insole Condition | Control Baseline | Intervention Baseline | Control Post | Intervention Post | Control Baseline to Post Change | Intervention Baseline to Post Change | Group Difference (Intervention – Control) | P value | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gait Measure | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean | SE | 95% CI | T-test | ||
| Even surface a | ||||||||||||
| Stride width (cm)b | Textured | 14.2 (4) | 13.3 (3.3) | 13.9 (3.5) | 13 (3.3) | −1 (16) | −2 (8) | −1.3 | 5.2 | (−12 to 10) | 0.81 | |
| Smooth | 14.3 (3.9) | 13.2 (2.7) | 13.4 (3.7) | 13.3 (3.6) | −7 (16) | −1 (12) | 5.9 | 5.6 | (−6 to 17) | 0.30 | ||
| Shoes only | 14.1 (4.1) | 13.3 (2.9) | 13.7 (3.6) | 13.5 (3.7) | −2 (15) | 0 (12) | 2.3 | 5.5 | (−9 to 14) | 0.67 | ||
| Barefoot | 14.4 (4.3) | 13 (3.1) | 13.5 (3.6) | 13.2 (3.6) | −5 (14) | 1 (9) | 6.1 | 4.7 | (−4 to 16) | 0.20 | ||
| Main c | −5 (16) | −3 (8) | 1.7 | 5.2 | (−9 to 12) | 0.74 | ||||||
| Stride time (s)b | Textured | 1.22 (0.41) | 1.12 (0.11) | 1.22 (0.38) | 1.12 (0.09) | 0 (5) | 0 (3) | −0.4 | 1.7 | (−4 to 3) | 0.83 | |
| Smooth | 1.23 (0.41) | 1.12 (0.11) | 1.22 (0.42) | 1.12 (0.1) | −1 (4) | 0 (3) | 0.2 | 1.4 | (−3 to 3) | 0.89 | ||
| Shoes only | 1.24 (0.43) | 1.12 (0.1) | 1.23 (0.43) | 1.12 (0.09) | −1 (6) | 0 (3) | 0.9 | 1.8 | (−3 to 5) | 0.62 | ||
| Barefoot | 1.19 (0.42) | 1.08 (0.1) | 1.18 (0.38) | 1.08 (0.09) | −1 (4) | 0 (3) | 0.4 | 1.4 | (−2 to 3) | 0.79 | ||
| Main c | −1 (5) | 0 (3) | 0.8 | 1.5 | (−2 to 4) | 0.59 | ||||||
| Double-limb support time (s)b | Textured | 0.25 (0.16) | 0.22 (0.04) | 0.22 (0.08) | 0.21 (0.04) | −6 (20) | −4 (6) | 2.4 | 6.0 | (−10 to 15) | 0.69 | |
| Smooth | 0.25 (0.15) | 0.22 (0.04) | 0.22 (0.08) | 0.21 (0.04) | −7 (17) | −5 (5) | 2.2 | 5.2 | (−9 to 13) | 0.67 | ||
| Shoes only | 0.25 (0.16) | 0.21 (0.04) | 0.22 (0.08) | 0.21 (0.04) | −8 (21) | −3 (7) | 5.3 | 6.4 | (−8 to 19) | 0.42 | ||
| Barefoot | 0.26 (0.19) | 0.21 (0.05) | 0.24 (0.13) | 0.21 (0.05) | −5 (13) | −3 (7) | 2.1 | 4.2 | (−7 to 11) | 0.63 | ||
| Main c | −6 (19) | −2 (6) | 4.0 | 5.8 | (−8 to 16) | 0.50 | ||||||
| Velocity (cm/s) | Textured | 114 (32) | 123 (24) | 114 (32) | 125 (22) | 0 (11) | 2 (9) | 2 | 4.1 | (−6 to 10) | 0.62 | |
| Smooth | 112 (31) | 123 (25) | 115 (31) | 124 (20) | 3 (9) | 1 (9) | −2 | 3.5 | (−9 to 5) | 0.58 | ||
| Shoes only | 111 (32) | 122 (23) | 115 (32) | 123 (19) | 4 (12) | 0 (8) | −3.3 | 4 | (−12 to 5) | 0.42 | ||
| Barefoot | 108 (32) | 120 (24) | 111 (31) | 121 (19) | 3 (8) | 1 (9) | −2.1 | 3.5 | (−9 to 5) | 0.54 | ||
| Main c | 4 (10) | 3 (9) | −1.1 | 3.9 | (−9 to 7) | 0.77 | ||||||
| Stride length (cm) | Textured | 128 (26) | 137 (22) | 129 (24) | 139 (21) | 1 (11) | 2 (7) | 1.1 | 3.7 | (−7 to 9) | 0.78 | |
| Smooth | 127 (26) | 136 (22) | 131 (23) | 138 (19) | 4 (9) | 2 (6) | −2.3 | 3.1 | (−9 to 4) | 0.46 | ||
| Shoes only | 126 (26) | 136 (21) | 131 (23) | 137 (18) | 5 (10) | 2 (6) | −3 | 3.2 | (−10 to 4) | 0.36 | ||
| Barefoot | 118 (26) | 128 (21) | 122 (22) | 129 (18) | 4 (10) | 1 (6) | −2.9 | 3.4 | (−10 to 4) | 0.41 | ||
| Main c | 5 (9) | 4 (8) | −1.2 | 3.4 | (−8 to 6) | 0.73 | ||||||
| Uneven surface d | ||||||||||||
| Step width (cm)b | Textured | 16.5 (2.6) | 17.6 (4.7) | 15.6 (3.9) | 16.7 (5.6) | −7 (14) | −7 (17) | −0.6 | 6.3 | (−14 to 13) | 0.93 | |
| Smooth | 16.2 (2.9) | 17.6 (4.7) | 14.5 (4) | 17.4 (5.2) | −13 (19) | −2 (11) | 11.2 | 6.1 | (−1 to 24) | 0.08 | ||
| Shoes only | 16.6 (2.7) | 17.1 (5.3) | 16 (2.9) | 16.5 (5.1) | −4 (12) | −3 (10) | 0.9 | 4.4 | (−8 to 10) | 0.84 | ||
| Barefoot | 16.1 (4.1) | 16.7 (4.6) | 15.4 (3.6) | 16.8 (4.8) | −4 (12) | 0 (12) | 3.6 | 4.8 | (−6 to 13) | 0.47 | ||
| Main c | −16 (18) | −3 (15) | 13.3 | 6.6 | (0 to 27) | 0.06 | ||||||
| Stride time (s)b | Textured | 1.2 (0.13) | 1.19 (0.12) | 1.22 (0.24) | 1.17 (0.12) | 1 (9) | −1 (4) | −2.0 | 2.9 | (−8 to 4) | 0.49 | |
| Smooth | 1.23 (0.16) | 1.2 (0.17) | 1.19 (0.18) | 1.17 (0.11) | −3 (7) | −2 (9) | 1.1 | 3.2 | (−6 to 8) | 0.74 | ||
| Shoes only | 1.24 (0.2) | 1.2 (0.13) | 1.19 (0.14) | 1.19 (0.14) | −4 (6) | −1 (4) | 2.5 | 2.2 | (−2 to 7) | 0.26 | ||
| Barefoot | 1.32 (0.34) | 1.21 (0.18) | 1.22 (0.23) | 1.16 (0.13) | −6 (9) | −4 (6) | 2.2 | 3.1 | (−4 to 9) | 0.50 | ||
| Main c | −4 (9) | −2 (5) | 1.5 | 2.9 | (−4 to 8) | 0.60 | ||||||
| Double-limb support time (s)b | Textured | 0.23 (0.08) | 0.21 (0.06) | 0.25 (0.16) | 0.19 (0.07) | 0 (27) | −10 (15) | −10.6 | 8.6 | (−28 to 7) | 0.23 | |
| Smooth | 0.24 (0.09) | 0.23 (0.1) | 0.22 (0.1) | 0.2 (0.06) | −8 (21) | −8 (20) | 0.4 | 8.1 | (−16 to 17) | 0.96 | ||
| Shoes only | 0.26 (0.13) | 0.22 (0.07) | 0.23 (0.08) | 0.21 (0.07) | −8 (24) | −6 (13) | 1.6 | 7.6 | (−14 to 17) | 0.83 | ||
| Barefoot | 0.32 (0.2) | 0.24 (0.1) | 0.26 (0.13) | 0.21 (0.08) | −12 (23) | −10 (14) | 1.6 | 7.6 | (−14 to 17) | 0.83 | ||
| Main c | −13 (25) | −16 (20) | −3.3 | 9.0 | (−22 to 15) | 0.72 | ||||||
| Velocity (cm/s) | Textured | 109 (26) | 114 (26) | 111 (30) | 118 (24) | 2 (13) | 4 (10) | 2.4 | 4.6 | (−7 to 12) | 0.61 | |
| Smooth | 106 (29) | 113 (31) | 115 (28) | 117 (24) | 9 (14) | 4 (13) | −4.9 | 5.4 | (−16 to 6) | 0.37 | ||
| Shoes only | 106 (30) | 111 (25) | 112 (28) | 116 (25) | 7 (10) | 5 (9) | −2 | 3.7 | (−10 to 6) | 0.59 | ||
| Barefoot | 96 (34) | 106 (27) | 103 (30) | 111 (26) | 7 (9) | 6 (8) | −1.6 | 3.4 | (−9 to 6) | 0.65 | ||
| Main c | 9 (15) | 7 (10) | −2.7 | 5.1 | (−13 to 8) | 0.60 | ||||||
| Stride length (cm) | Textured | 128 (22) | 132 (23) | 130 (26) | 136 (20) | 2 (11) | 4 (8) | 2.2 | 3.9 | (−6 to 10) | 0.58 | |
| Smooth | 127 (24) | 131 (26) | 133 (24) | 135 (21) | 7 (13) | 4 (9) | −2.7 | 4.4 | (−12 to 7) | 0.55 | ||
| Shoes only | 126 (25) | 131 (21) | 130 (23) | 134 (21) | 4 (8) | 4 (7) | −0.6 | 2.9 | (−7 to 5) | 0.83 | ||
| Barefoot | 117 (25) | 123 (20) | 121 (24) | 126 (21) | 4 (8) | 3 (6) | −1 | 2.7 | (−7 to 5) | 0.71 | ||
| Main c | 7 (13) | 5 (7) | −1.9 | 4.2 | (−10 to 7) | 0.65 | ||||||
Secondary outcome measures
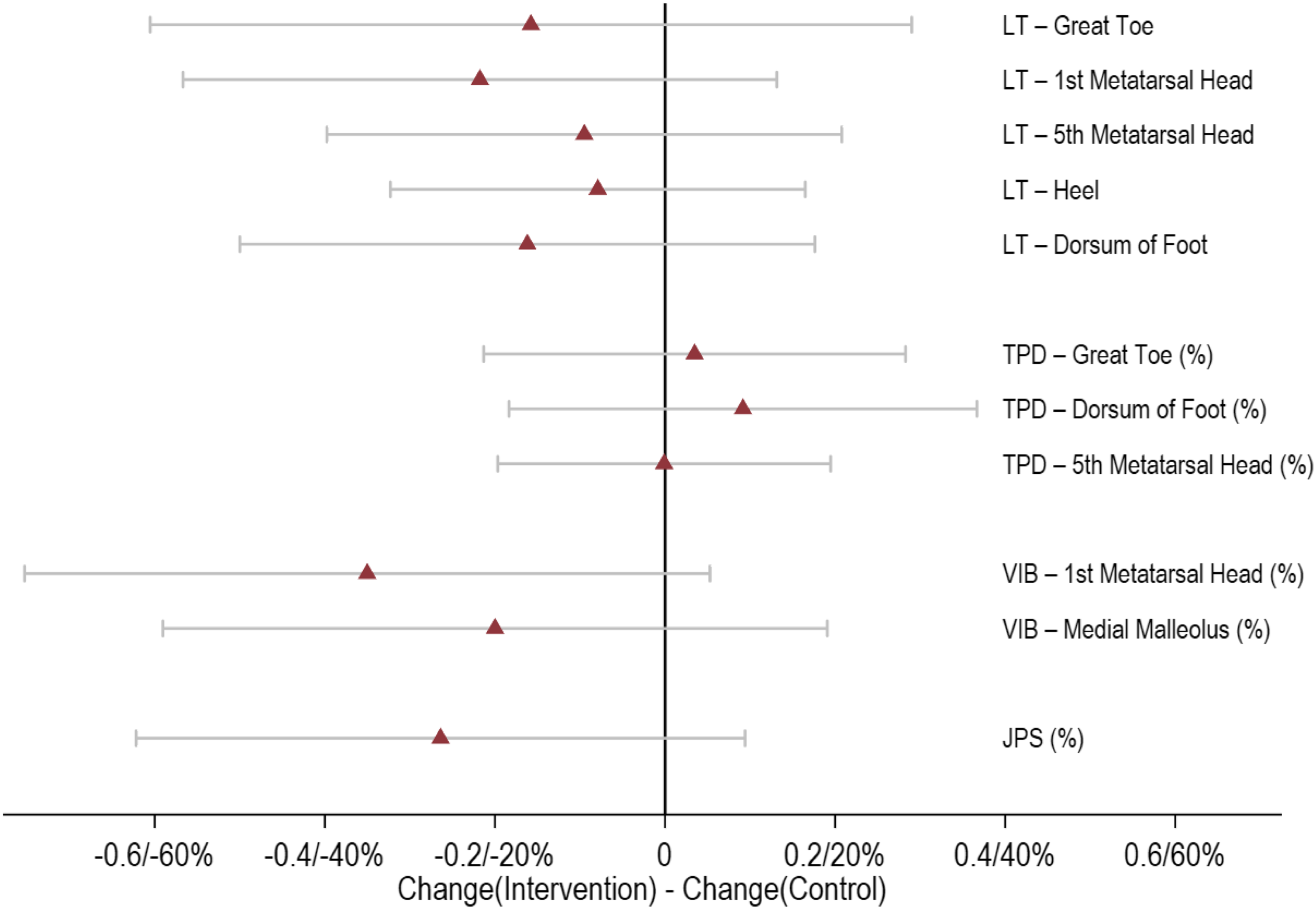
There were no significant between-group differences for changes in the secondary gait parameters when walking over the even or uneven surface, after wearing textured insoles for 12 weeks (all P values > 0.23) (Fig. 3 and Table 2). We observed no significant changes in measures of foot sensory function between groups (all P values ≥ 0.08) (Fig. 4 and Table 3). Data from the insole wear diaries indicated that a proportion of participants in the control (N = 7, 47%) and intervention (N = 9, 60%) groups, reported experiencing changes in foot sensation, but this was not significantly different (P = 0.72). There were no significant between-group differences for any patient-reported outcomes (all P values ≥ 0.23) (Table 4).
Effect of intervention (versus control) with 95% confidence interval for change in light-touch pressure sense measures, and symmetric percentage change in two-point discrimination, vibration sense, and joint position sense measures. LT, light-touch pressure sense; TPD, two-point discrimination; VIB, vibration sense; JPS, joint position sense.
Changes in Foot Sensation and Proprioception Measures (Averaged Across Right and Left Legs) from Baseline to Post-intervention for the Control (Smooth Insole, N = 15) and Intervention (Textured Insole, N = 15) Groups
| Foot Sensory Measure | Control Baseline | Intervention Baseline | Control Post | Intervention Post | Control Baseline to Post Change | Intervention Baseline to Post Change | Group Difference (Intervention – Control) | P value | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean | SE | 95% CI | T-test | ||
| Light-touch pressure sense | |||||||||||
| Great toe | 4.01 (0.66) | 4.14 (0.67) | 4.10 (0.96) | 4.07 (0.8) | 0.09 (0.55) | −0.07 (0.65) | −0.16 | 0.22 | (−0.61 to 0.29) | 0.48 | |
| 1st metatarsal head | 3.89 (0.47) | 3.88 (0.59) | 4.08 (0.62) | 3.85 (0.75) | 0.19 (0.45) | −0.03 (0.48) | −0.22 | 0.17 | (−0.57 to 0.13) | 0.21 | |
| 5th metatarsal head | 4.01 (0.56) | 4.18 (0.59) | 4.09 (0.6) | 4.16 (0.88) | 0.08 (0.29) | −0.01 (0.5) | −0.09 | 0.15 | (−0.4 to 0.21) | 0.53 | |
| Heel | 4.28 (0.44) | 4.28 (0.56) | 4.26 (0.51) | 4.18 (0.71) | −0.02 (0.3) | −0.1 (0.35) | −0.08 | 0.12 | (−0.32 to 0.16) | 0.51 | |
| Dorsum of foot | 3.89 (0.44) | 3.68 (0.44) | 3.99 (0.53) | 3.62 (0.78) | 0.1 (0.32) | −0.06 (0.56) | −0.16 | 0.17 | (−0.5 to 0.18) | 0.34 | |
| Two-point discrimination (mm) | |||||||||||
| Great toea | 1.4 (0.97) | 1.13 (0.59) | 1.43 (1.13) | 1.10 (0.34) | 1 (25) | 5 (40) | 3 | 12 | (−21 to 28) | 0.78 | |
| 5th metatarsal heada | 2.14 (1.18) | 1.65 (0.44) | 2.15 (1.32) | 1.62 (0.52) | 0 (25) | −1 (27) | 0 | 10 | (−20 to 19) | 0.99 | |
| Dorsum of foota | 2.96 (1.2) | 2.09 (0.65) | 2.30 (0.96) | 1.73 (0.33) | −23 (42) | −13 (30) | 9 | 13 | (−18 to 37) | 0.50 | |
| Vibration sense (s) | |||||||||||
| 1st metatarsal heada | 12.45 (17.17) | 10.28 (9.23) | 13.67 (16.78) | 7.78 (5.45) | 17 (35) | −18 (68) | −35 | 20 | (−75 to 5) | 0.09 | |
| Medial malleolusa | 7.59 (8.15) | 9.48 (8.41) | 8.42 (7.89) | 7.47 (4.75) | 11 (41) | −9 (62) | −20 | 19 | (−59 to 19) | 0.30 | |
| Proprioception (°error) | |||||||||||
| Ankle joint position sensea | 3.84 (2.01) | 4.62 (2.15) | 3.62 (1.19) | 3.55 (2.03) | 0 (57) | −26 (36) | −26 | 17 | (−62 to 9) | 0.14 | |
Changes in Patient-Reported Outcome Measures from Baseline to Post-intervention for the Control (Smooth Insole, N = 15) and Intervention (Textured Insole, N = 15) Groups
| Patient-Reported Outcome Measure | Control Baseline | Intervention Baseline | Control Post | Intervention Post | Control Baseline to Post Change | Intervention Baseline to Post Change | Group Difference (Intervention – Control) | P value | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean | SE | 95% CI | T-test | ||
| MS Walking Scale | 32.9 (14.5) | 35.9 (12.4) | 32.1 (15.2) | 35.1 (11.7) | −0.8 (5) | −0.7 (6.6) | 0.1 | 2.1 | (−4.3 to 4.4) | 0.98 | |
| MS Impact Scale | |||||||||||
| Physical subscalea | 34.7 (21.8) | 33.3 (19) | 29.3 (19.1) | 29.6 (18.1) | −21 (41) | −13 (43) | 9 | 15 | (−23 to 40) | 0.58 | |
| Psychological subscalea | 35 (26.1) | 30.4 (20.8) | 30.9 (23.6) | 22 (16.2) | −14 (57) | −18 (64) | −4 | 22 | (−49 to 41) | 0.86 | |
| Total scorea | 69.7 (46.5) | 63.6 (35.1) | 60.3 (40.7) | 51.6 (29.7) | −17 (40) | −17 (44) | 0 | 15 | (−31 to 32) | 0.98 | |
| Perceived Deficits Questionnaire | |||||||||||
| Attention | 9.3 (4) | 8.7 (4.7) | 8.3 (4.9) | 7.9 (3.2) | −1.1 (3.4) | −0.9 (2.2) | 0.2 | 1.1 | (−2 to 2.4) | 0.85 | |
| Retrospective memory | 8.4 (3.8) | 7.7 (4.3) | 7.6 (4.7) | 7.7 (3.5) | −0.8 (3.2) | 0.1 (3.1) | 0.9 | 1.2 | (−1.5 to 3.2) | 0.46 | |
| Prospective memory | 7.7 (3.9) | 5.4 (3.9) | 6.9 (4.5) | 5.7 (2.8) | −0.9 (2.6) | 0.3 (2.5) | 1.1 | 0.9 | (−0.8 to 3) | 0.23 | |
| Planning/organization | 9.1 (4.4) | 7.3 (4.2) | 7.8 (5) | 6.1 (3.6) | −1.3 (2.9) | −1.2 (1.3) | 0.1 | 0.8 | (−1.6 to 1.8) | 0.94 | |
| Total score | 34.5 (15.1) | 29.1 (16.2) | 30.5 (18.1) | 27.4 (11.9) | −4 (10.5) | −1.7 (8) | 2.3 | 3.4 | (−4.7 to 9.2) | 0.51 | |
| Modified Fatigue Impact Scale | |||||||||||
| Physical subscale | 20.5 (8.8) | 22.7 (6.8) | 19.5 (9) | 20.3 (7.9) | −1 (4.1) | −2.4 (4.8) | −1.4 | 1.6 | (−4.7 to 1.9) | 0.40 | |
| Cognitive subscale | 18.6 (8.3) | 17.2 (8.4) | 16.3 (8.3) | 16.3 (8.2) | −2.3 (6.3) | −0.9 (4.6) | 1.3 | 2 | (−2.8 to 5.5) | 0.52 | |
| Psychosocial subscale | 3.9 (1.9) | 4.1 (1.3) | 3.5 (2.3) | 3.9 (1.6) | −0.5 (1.5) | −0.1 (1.4) | 0.3 | 0.5 | (−0.7 to 1.4) | 0.52 | |
| Total score | 43 (18.1) | 44 (13.4) | 39.3 (18.2) | 40.5 (14.7) | −3.7 (10.7) | −3.5 (8.6) | 0.3 | 3.5 | (−7 to 7.5) | 0.94 | |
| Medical Outcomes Study Pain Effects Scalea | 14.7 (7.4) | 12.7 (4.9) | 13.1 (6) | 13.3 (5) | −10 (27) | 5 (43) | 15 | 13 | (−12 to 42) | 0.26 | |
| Falls Efficacy Scale-Internationala | 29.3 (12.4) | 30.9 (11.2) | 29.5 (13.7) | 30.5 (11.5) | −2 (15) | −1 (19) | 0 | 6 | (−12 to 13) | 0.97 | |
| MS Quality of Life Instrument | |||||||||||
| Physical subscaleb | 56.2 (21) | 56.5 (18.1) | 52.3 (24.5) | 54.9 (12.9) | −0.5 (7.9) | −0.2 (10.9) | 0.3 | 4 | (−7.9 to 8.5) | 0.94 | |
| Mental subscale | 66.3 (22.3) | 64.4 (17.5) | 67.6 (19.6) | 69 (15.7) | 1.3 (16.4) | 4.6 (13.8) | 3.3 | 5.5 | (−8 to 14.6) | 0.56 | |
Discussion
This study investigated whether prolonged wear of textured shoe insoles alters spatiotemporal walking patterns and foot sensory function in pwMS. Contrary to our hypotheses, there were no differences in gait patterns, foot sensory measures, or patient-reported outcomes in pwMS after wearing textured insoles for 12 weeks. Similar results were found for the pwMS allocated to the control group, who wore smooth insoles for 12 weeks.
Our study was the first to explore the effects of wearing textured insoles over an extended period (>4 weeks). Several studies have reported the positive effect of textured insoles on balance and walking in neurological disease groups, upon wearing the insoles for the first time (immediate effects) (Jenkins et al., 2009; Kalron et al., 2015; Kelleher et al., 2010; Qiu et al., 2013) and after short-term wear (up to 4 weeks) (Dixon et al., 2014; Kalron et al., 2015; Lirani-Silva et al., 2017). Our previous pilot study in pwMS reported improvements in stride length, ML base of support and double-limb support time during level-ground walking, after wearing textured insoles for 2 weeks (Dixon et al., 2014), however, no significant immediate effects were observed. Subsequent work by Kalron et al. (2015) demonstrated that textured insoles had no immediate or short-term wear (4 weeks) effects on spatiotemporal gait or plantar sensory measures in pwMS. Rather, the therapeutic benefits of textured insoles were observed for standing balance only, with improvements in centre of pressure measures immediately after inserting the insoles (vs shoes only), which were maintained at 4-week follow-up (Kalron et al., 2015). Evidence in other neurological disease groups, specifically Parkinson’s disease, supports the theory that immediate and short-term exposure to textured footwear interventions has the capacity to improve single-limb support time (Jenkins et al., 2009), stride length (Lirani-Silva et al., 2017) and plantar sensation (Lirani-Silva et al., 2017). However, conflicting findings from a systematic review report that sensory-stimulating insoles (e.g., texture) do not improve balance or gait in pwMS or Parkinson’s disease (Alfuth, 2017). Importantly, the findings from Alfuth (2017) should be interpreted with caution due to the methodological approach and analyses undertaken.
In the current study, we observed no significant changes in gait or foot sensory measures after wearing textured insoles for 12 weeks. It is possible that during this longer intervention period participants may have habituated to the sensory stimulus, which negated any beneficial insole effects that accrued in the short term. Furthermore, there may be a dose–response relationship with regard to the therapeutic effects of textured insoles, whereby the physical properties of the textured stimuli may need to be modulated (e.g., increasingly larger protrusions), once a user has acclimatised to the stimuli, to ensure any benefits continue to accrue. There is convincing evidence that an individuals’ response to footwear devices, designed to improve balance and walking, can fluctuate over time. Ramdharry, Marsden, Day and Thompson (2006) reported that wearing foot orthoses for 4 weeks led to an initial de-stabilisation effect in pwMS that was superseded by improvements in balance. Taken together, this evidence suggests that we do not clearly understand the optimal treatment duration for wearing textured insoles, to elicit sustained improvements in gait and foot sensation.
A secondary aim was to explore if wearing textured insoles alters foot sensory function, as an underlying mechanism of action. Contrary to our hypothesis, we reported no between-group differences in any of the foot sensory measures, at post-intervention. This result supports work by other groups (Kalron et al., 2015), who similarly observed no change in plantar light-touch pressure sense in 25 pwMS, following short-term wear (4 weeks) of textured insoles. One possible explanation for this finding is that pwMS who had severe foot sensory loss were excluded from the current study. This was based on the rationale that it was important for participants to be able to perceive the textured stimuli for the insoles to be effective. However, our systematic review indicated that people with reduced foot sensation may benefit most from textured insoles, through the provision of ‘substitute’ sensory information (Paton, Hatton, Rome & Kent, 2016).
Limitations
There were several study limitations. First, our small sample size could mean the study was underpowered to detect effects of a plausible magnitude of textured insoles on gait and foot sensation, and thus, the results should be interpreted with caution. Second, pwMS who had severe loss of foot sensation were excluded. Emerging evidence proposes that individuals with reduced foot sensation may benefit most from textured insoles (Paton et al., 2016). Therefore, our participant selection criteria may have limited the ability to observe the true potential of textured insoles. Third, wearing textured insoles could lead to beneficial changes in measures that were not assessed in this work, e.g., gait kinetics, neuromuscular function, physical activity levels.
Conclusions
Wearing textured insoles for 12 weeks did not appear to alter walking patterns or foot sensation in pwMS who have limited foot sensory loss. However, textured insoles may be an effective gait rehabilitation strategy for pwMS who have significant loss of foot sensation: this area is yet to be explored. It remains unclear if wearing textured insoles for an extended period leads a user to habituate to the sensory stimuli, and thus any immediate or short-term improvements in gait become redundant over time. Further research is warranted to investigate the effects of textured insoles in pwMS with neuropathy and to explore different textured insole design features, by way of larger studies.
Supplementary materials
For supplementary material for this article, please visit https://doi.org/10.1017/BrImp.2022.33
Acknowledgements
The authors would like to acknowledge Sarah Robins and Jessica Thompson for their contribution to completing the blinded assessments; and Robyn Lamont for maintaining the randomisation schedule. The authors would also like to thank Nampech Wuthapanich and Jessica Thompson for their assistance with data processing. In particular, the authors would like to acknowledge Multiple Sclerosis Queensland for their involvement with participant recruitment.
Financial support
This work was supported by a Multiple Sclerosis Research Australia Project Grant (Grant ID: 13-006) awarded to ALH, KW, JD, KR, GK and SGB.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
Alfuth, M. (2017) Textured and stimulating insoles for balance and gait impairments in patients with multiple sclerosis and Parkinson’s disease: A systematic review and meta-analysis. Gait and Posture 51, 132-141.
| Google Scholar |
Archibald, C. J., McGrath, P. J., Ritvo, P. G., Fisk, J. D., Bhan, V., Maxner, C. E., Murray, T. J. (1994) Pain prevalence, severity and impact in a clinic sample of multiple sclerosis patients. Pain 58(1), 89-93.
| Google Scholar |
Aries, A. M., Pomeroy, V. M., Sim, J., Read, S., Hunter, S. M. (2021) Sensory stimulation of the foot and ankle early post-stroke: A pilot and feasibility study. Frontiers in Neurology 5(12), 675106.
| Google Scholar |
Armstrong, D. G., Lavery, L. A., Vela, S. A., Quebedeaux, T. L., Fleischli, J. G. (1998) Choosing a practical screening instrument to identify patients at risk for diabetic foot ulceration. Archives of Internal Medicine 158(3), 289-292.
| Google Scholar |
Aruin, A. S., Rao, N. (2018) The effect of a single textured insole in gait rehabilitation of individuals with stroke. International Journal of Rehabilitation Research 41(3), 218-223.
| Google Scholar |
Baron, Y., Hatton, A., Robinson, J., Hodgson, D., McKeon, P., Rome, K., Dixon, J. (2016) Participant perception of the effect of textured insoles on balance and gait in people with multiple sclerosis. Physiotherapy 102, e58-59.
| Google Scholar |
Baron, Y. J., Hatton, A., Robinson, J., Hodgson, D., McKeon, P., Rome, K., Dixon, J. (2016) Long-term effect of textured insoles on gait and balance in people with multiple sclerosis: An exploratory randomised controlled trial. Physiotherapy 102(Supplement 1), e57.
| Google Scholar |
Baron, Y. J., Robinson, J., Gamesby-Iyayi, H., Hodgson, D., Hatton, D., Warnett, R., Martin, D. (2014) Perceptions of people with multiple sclerosis on the effect and comfort of two different textured insoles: A qualitative study. International Journal of Therapy and Rehabilitation 21(Sup7), S2.
| Google Scholar |
Batey, P., Rome, K., Finn, P., Hanchard, N. (2003) Assessing reliability of measurement of gait velocity. Physiotherapy 89(5), 313-317.
| Google Scholar |
Citaker, S., Gunduz, A. G., Guclu, M. B., Nazliel, B., Irkec, C., Kaya, D. (2011) Relationship between foot sensation and standing balance in patients with multiple sclerosis. Gait and Posture 34(2), 275-278.
| Google Scholar |
Cole, T. J. (2000) Sympercents: Symmetric percentage differences on the 100 log(e) scale simplify the presentation of log transformed data. Statistics in Medicine 19(22), 3109-3125.
| Google Scholar |
Collings, R., Paton, J., Chockalingam, N., Gorst, T., Marsden, J. (2015) Effects of the site and extent of plantar cutaneous stimulation on dynamic balance and muscle activity while walking. The Foot 25(3), 159-163.
| Google Scholar |
Davies, B. L., Arpin, D. J., Liu, M., Reelfs, H., Volkman, K. G., Healey, K., Kurz, M. J. (2016) Two different types of high-frequency physical therapy promote improvements in the balance and mobility of persons with Multiple Sclerosis. Archives of Physical Medicine and Rehabilitation 97(12), 2095-2101.
| Google Scholar |
DeBolt, L., McCubbin, J. (2004) The effects of home-based resistance exercise on balance, power, and mobility in adults with multiple sclerosis. Archives of Physical Medicine and Rehabilitation 85(2), 290-297.
| Google Scholar |
Dixon, J., Hatton, A. L., Robinson, J., Gamesby-Iyayi, H., Hodgson, D., Rome, K., Martin, D. J. (2014) Effect of textured insoles on balance and gait in people with multiple sclerosis: An exploratory trial. Physiotherapy 100(2), 142-149.
| Google Scholar |
Edwardson, C. L., Winkler, E. A. H., Bodicoat, D. H., Yates, T., Davies, M. J., Dunstan, D. W., Healy, G. N. (2017) Considerations when using the activPAL monitor in field-based research with adult populations. Journal of Sport and Health Science 6(2), 162-178.
| Google Scholar |
Finlayson, M., Peterson, E., Cho, C. (2006) Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Archives of Physical Medicine and Rehabilitation 87(9), 1274-1279.
| Google Scholar |
Fisk, J. D., Pontefract, A., Ritvo, P. G., Archibald, C. J., Murray, T. J. (1992) The impact of fatigue on patients with multiple sclerosis. Canadian Journal of Neurological Sciences 21(1), 9-14.
| Google Scholar |
Folstein, M., Folstein, S., McHugh, P. (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 12(3), 189-198.
| Google Scholar |
Garrett, M., Hogan, N., Larkin, A., Saunders, J., Jakeman, P., Coote, S. (2013) Exercise in the community for people with minimal gait impairment due to MS: An assessor-blind randomized controlled trial. Multiple Sclerosis Journal 19(6), 782-789.
| Google Scholar |
Givon, U., Zeilig, G., Achiron, A. (2009) Gait analysis in multiple sclerosis: Characterization of temporal-spatial parameters using GAITRite functional ambulation system. Gait and Posture 29(1), 138-142.
| Google Scholar |
Hasan, H., Davids, K., Chow, J. Y., Kerr, G. (2017) Changes in organisation of instep kicking as a function of wearing compression and textured materials. European Journal of Sport Science 17(3), 294-302.
| Google Scholar |
Hatton, A. L., Dixon, J., Rome, K., Brauer, S. G., Williams, K., Kerr, G. (2016) The effects of prolonged wear of textured shoe insoles on gait, foot sensation and proprioception in people with multiple sclerosis: Study protocol for a RCT. Trials 17(1), 208.
| Google Scholar |
Hatton, A. L., Dixon, J., Rome, K., Newton, J. L., Martin, D. J. (2012) Altering gait by way of stimulation of the plantar surface of the foot: The immediate effect of wearing textured insoles in older fallers. Journal of Foot and Ankle Research 5(1), 11.
| Google Scholar |
Hobart, J., Lamping, D., Fitzpatrick, R., Riazi, A., Thompson, A. (2001) The Multiple Sclerosis Impact Scale (MSIS-29): A new patient-based outcome measure. Brain 124(5), 962-973.
| Google Scholar |
Hobart, J. C., Riazi, A., Lamping, D. L., Fitzpatrick, R., Thompson, A. J. (2003) Measuring the impact of MS on walking ability: The 12-Item MS Walking Scale (MSWS-12). Neurology 60, 31-36.
| Google Scholar |
Hohol, M. J., Orav, E. J., Weiner, H. L. (1995) Disease steps in multiple sclerosis: A simple approach to evaluate disease progression. Neurology 45(2), 251-255.
| Google Scholar |
Hollander, K., Petersen, E., Zech, A., Hamacher, D. (2022) Effects of barefoot vs. shod walking during indoor and outdoor conditions in younger and older adults. Gait and Posture 95, 284-291.
| Google Scholar |
Jamali, A., Forghany, S., Bapirzadeh, K., Nester, C. (2019) The effect of three different insoles on ankle movement variability during walking in athletes with functional ankle instability. Advanced Biomedical Research 28(8), 42.
| Google Scholar |
Jenkins, M. E., Almeida, Q. J., Spaulding, S. J., van Oostveen, R. B., Holmes, J. D., Johnson, A. M., Perry, S. D. (2009) Plantar cutaneous sensory stimulation improves single-limb support time and EMG activation patterns in Parkinson’s disease. Parkinsonism & Related Disorders 15(9), 697-702.
| Google Scholar |
Kalron, A., Dvir, Z., Achiron, A. (2010) Walking while talking - Difficulties incurred during the initial stages of multiple sclerosis disease process. Gait and Posture 32(3), 332-335.
| Google Scholar |
Kalron, A., Pasitselsky, D., Greenberg-Abrahami, M., Achiron, A. (2015) Do textured insoles affect postural control and spatiotemporal parameters of gait and plantar sensation in people with multiple sclerosis? Physical Medicine and Rehabilitation 7(1), 17-25.
| Google Scholar |
Kelleher, K. J., Spence, W. D., Solomonidis, S., Apatsidis, D. (2010) The effect of textured insoles on gait patterns of people with multiple sclerosis. Gait and Posture 32(1), 67-71.
| Google Scholar |
Khan, F., Amatya, B. (2017) Rehabilitation in Multiple Sclerosis: A systematic review of systematic reviews. Archives of Physical Medicine and Rehabilitation 98(2), 353-367.
| Google Scholar |
Learmonth, Y. C., Paul, L., Miller, L., Mattison, P., McFadyen, A. K. (2012) The effects of a 12-week leisure centre-based, group exercise intervention for people moderately affected with multiple sclerosis: A randomized controlled pilot study. Clinical Rehabilitation 26(7), 579-593.
| Google Scholar |
Lirani-Silva, E., Vitório, R., Barbieri, F. A., Orcioli-Silva, D., Simieli, L., Gobbi, L. T. B. (2017) Continuous use of textured insole improve plantar sensation and stride length of people with Parkinson’s disease: A pilot study. Gait and Posture 58, 495-497.
| Google Scholar |
Ma, C. C., Rao, N., Muthukrishnan, S., Aruin, A. S. (2018) A textured insole improves gait symmetry in individuals with stroke. Disability and Rehabilitation 40(23), 2798-2802.
| Google Scholar |
Martin, C. L., Phillips, B. A., Kilpatrick, T. J., Butzkueven, H., Tubridy, N., McDonald, E., Galea, M. P. (2006) Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Multiple Sclerosis Journal 12(5), 620-628.
| Google Scholar |
Matsuda, P. N., Shumway-Cook, A., Bamer, A. M., Johnson, S. L., Amtmann, D., Kraft, G. H. (2011) Falls in multiple sclerosis. Physical Medicine and Rehabilitation 3(7), 624-632.
| Google Scholar |
Menant, J. C., Steele, J. R., Menz, H. B., Munro, B. J., Lord, S. R. (2009) Effects of walking surfaces and footwear on temporo-spatial gait parameters in young and older people. Gait and Posture 29(3), 392-397.
| Google Scholar |
Mills, K., Blanch, P., Vicenzino, B. (2010) Identifying clinically meaningful tools for measuring comfort perception of footwear. Medicine & Science in Sports & Exercise 42(10), 1966-1971.
| Google Scholar |
Nilsagård, Y., Gunn, H., Freeman, J., Hoang, P., Lord, S., Mazumder, R., Cameron, M. (2015) Falls in people with MS, an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Multiple Sclerosis Journal 21, 92-100.
| Google Scholar |
Nurse, M. A., Hulliger, M., Wakeling, J. M., Nigg, B. M., Stefanyshyn, D. J. (2005) Changing the texture of footwear can alter gait patterns. Journal of Electromyography & Kinesiology 15(5), 496-506.
| Google Scholar |
Paton, J., Hatton, A. L., Rome, K., Kent, B. (2016) Effects of foot and ankle devices on balance, gait and falls in adults with sensory perception loss: A systematic review. JBI Database of Systematic Reviews and Implementation Reports 14(12), 127-162.
| Google Scholar |
Pearson, M., Dieberg, G., Smart, N. (2015) Exercise as a therapy for improvement of walking ability in adults with multiple sclerosis: A meta-analysis. Archives of Physical Medicine and Rehabilitation 96(7), 1339-1348.
| Google Scholar |
Perry, S. D., Radtke, A., McIlroy, W. E., Fernie, G. R., Maki, B. E. (2008) Efficacy and effectiveness of a balance-enhancing insole. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 63(6), 595-602.
| Google Scholar |
Peterson, E., Cho, C., von Koch, L., Finlayson, M. L. (2008) Injurious falls among middle aged and older adults with Multiple Sclerosis. Archives of Physical Medicine and Rehabilitation 89(6), 1031-1037.
| Google Scholar |
Qiu, F., Cole, M. H., Davids, K. W., Hennig, E. M., Silburn, P. A., Netscher, H., Kerr, G. K. (2013) Effects of textured insoles on balance in people with Parkinson’s disease. PLoS One 8(12), e83309.
| Google Scholar |
Ramdharry, G. M., Marsden, J. F., Day, B. L., Thompson, A. J. (2006) De-stabilizing and training effects of foot orthoses in multiple sclerosis. Multiple Sclerosis Journal 12(2), 219-226.
| Google Scholar |
Riskowski, J. L., Mikesky, A. E., Bahamonde, R. E., Alvey, T. V., Burr, D. B. (2005) Proprioception, gait kinematics, and rate of loading during walking: Are they related? Journal of Musculoskeletal and Neuronal Interactions 5(4), 379-387.
| Google Scholar |
Roll, R., Kavounoudias, A., Roll, J. P. (2002) Cutaneous afferents from human plantar sole contribute to body posture awareness. Neuroreport 13(15), 1957-1961.
| Google Scholar |
Rougier, P., Thoumie, P., Cantalloube, S., Lamotte, D. (2007) What compensatory motor strategies do patients with multiple sclerosis develop for balance control? Revue Neurologique 163(11), 1054-1064.
| Google Scholar |
Russell, T. G., Jull, G. A., Wootton, R. (2003) Can the Internet be used as a medium to evaluate knee angle? Manual Therapy 8(4), 242-246.
| Google Scholar |
Scheinberg, L., Holland, N., LaRocca, N. (1980) Multiple Sclerosis: Earning a living. New York State Journal of Medicine 80(9), 1395-1400.
| Google Scholar |
Schmahmann, J. D., Gardner, R., MacMore, J., Vangel, M. G. (2009) Development of a Brief Ataxia Rating Scale (BARS) based on a modified form of the ICARS. Movement Disorders 24(12), 1820-1828.
| Google Scholar |
Schulz, K. F., Altman, D. G., Moher, D. (2010) CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 340, c323.
| Google Scholar |
Steinberg, N., Waddington, G., Adams, R., Karin, J., Begg, R., Tirosh, O. (2016) Can textured insoles improve ankle proprioception and performance in dancers? Journal of Sports Sciences 34(15), 1430-1437.
| Google Scholar |
Sullivan, J. J., Edgley, K., Dehoux, E. (1990) A survey of multiple sclerosis. Part 1. Perceived cognitive problems and compensatory strategy use. Canadian Journal of Rehabilitation 4, 99-105.
| Google Scholar |
Tardieu, G., Shentoub, S., Delarue, R. (1954) A la recherche d’une technique de mesure de la spasticite. Revue Neurologique 91, 143-144.
| Google Scholar |
Vickrey, B. G., Hays, R. D., Harooni, R., Myers, L. W., Ellison, G. W. (1995) A health-related quality of life measure for Multiple Sclerosis. Quality of Life Research 4(3), 187-206.
| Google Scholar |
Viseux, F., Lemaire, A., Barbier, F., Charpentier, P., Leteneur, S., Villeneuve, P. (2019) How can the stimulation of plantar cutaneous receptors improve postural control? Review and clinical commentary. Neurophysiologie Clinique 49(3), 263-268.
| Google Scholar |
Wiles, C. M., Newcombe, R. G., Fuller, K. J., Shaw, S., Furnival-Doran, J., Pickersgill, T. P., Morgan, A. (2001) Controlled randomised crossover trial of the effects of physiotherapy on mobility in chronic multiple sclerosis. Journal of Neurology, Neurosurgery, and Psychiatry 70(2), 174-179.
| Google Scholar |
Wilkinson, M., Ewen, A., Caplan, N., O'leary, D., Smith, N., Stoneham, R., Saxby, L. (2018) Textured insoles reduce vertical loading rate and increase subjective plantar sensation in overground running. European Journal of Sport Science 18(4), 497-503.
| Google Scholar |
Yardley, L., Beyer, N., Hauer, K., Kempen, G., Piot-Ziegler, C., Todd, C. (2005) Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age and Ageing 34(6), 614-619.
| Google Scholar |
Young, J., Moss, C. (2019) Orthotic care needs in a cohort of neurological rehabilitation inpatients. Disability and Rehabilitation: Assistive Technology 16(6), 609-613.
| Google Scholar |