Coronavirus (COVID-19) and sexualised drug use among men who have sex with men: a systematic review
Dean J. Connolly A * , Ece Eraslan A and Gail Gilchrist A
A * , Ece Eraslan A and Gail Gilchrist A
A National Addiction Centre, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, Windsor Walk, London, UK.
Abstract
Drug-related harms, including harms from sexualised drug use (SDU), are disproportionately experienced by sexual and gender minority people, relative to their majority counterparts. Chemsex, a type of SDU practiced mainly by MSM, is associated with methamphetamine use and increased HIV seropositivity or risk of acquisition. Therefore, participants are at increased risk of immunocompromise. Existing evidence suggests that drug use increases following natural disasters. The impact of coronavirus disease 2019 (COVID-19) on chemsex is unknown. A PRISMA-adherent systematic review was conducted to synthesise reports of changes in the prevalence, frequency, or characteristics of drug use (and factors associated with these changes) following the onset of the COVID-19 pandemic. This report presents findings related to SDU/chemsex among MSM. A comprehensive search across nine databases, supplemented with backward-forward citation searching and contact with key opinion leaders, was conducted. Two reviewers carried out title-abstract screening, full-text screening, and data extraction. Following a final, single database search, nine studies were included in the narrative synthesis. More than half the sample were studies investigating HIV pre-exposure prophylaxis use. Twenty percent of participants in most studies reported chemsex participation. In four, participants reported a net increase or maintenance of chemsex participation during the pandemic and five reported a net decrease. Increased chemsex participation was associated with loneliness, cravings, and working during the pandemic. Decreased chemsex practice was associated with COVID-19-related fear. This synthesis suggests that chemsex practice continued, and for some MSM increased, throughout COVID-19 pandemic ‘lockdowns’. This may have increased COVID-19 transmission and severity among potentially vulnerable MSM.
Keywords: chemsex, coronavirus, COVID-19, LGBTQ+, lockdown, men who have sex with men, pandemic, sexualised drug use.
Introduction
Despite significant progress affording lesbian, gay, bisexual, transgender and other sexual and gender minority (LGBT+) people greater social liberty and legal protections, they continue to experience disparities across a range of health domains.1 These include harm from alcohol, tobacco and illicit drug (drug) use and dependence.2,3 Sexual minority people have been found to use drugs earlier, in greater quantities, with more associated harms than their heterosexual counterparts.4–8
Sexualised drug use (SDU) is defined as the use of drugs before and or during sexual activity to prolong or enhance the experience.9 While SDU is common among people of all genders and sexual orientations,10 there are unique conditions that make SDU more common, and in some cases more harmful, among particular LGBT+ subgroups. Men who have sex with men (MSM) are believed to experience a unique set of social (e.g. hook-up culture) and psychological (e.g. shame around ‘homo sex’) conditions that bring about a cultural phenomenon known as ‘chemsex’ that is characterised by the use of geospatial networking applications to engage in sex with multiple concurrent or sequential partners under the influence of any combination of crystal methamphetamine (crystal), gamma hydroxybutyric acid/gamma butyrolactone (GHB/GBL) and mephedrone.11 SDU has also been found to be common among women who have sex with women (WSW) and among transgender women who have sex with men.3,12,13 However, these groups are not as widely reported on as cisgender MSM and there is a dearth of evidence relating to SDU among transgender men and non-binary people.3
The prevalence of SDU/chemsex varies between countries and depends on the operationalisation of the behaviour. However, using the United Kingdom (UK) as an example, ~17% of sexual health clinic attendees and ~31% of HIV service users are estimated to participate in chemsex.9 While not all MSM who participate in SDU/chemsex encounter significant problems,14 there is a substantial risk of a range of physical and psychosocial harms. SDU practice has been associated with an increased risk of acquiring sexually transmitted infections (STIs),15 poorer engagement in HIV-related care,16 soft-tissue and other injecting consequences,17 mental ill health (including psychosis),18 sexual violence victimisation,19 among other issues.
In March 2020, the World Health Organization declared a pandemic as cases of the novel, highly infectious strain of coronavirus disease 2019 (COVID-19) continued to rise across the globe.20 Public health emergencies of this magnitude have rarely been recorded. However, evidence from historical natural disasters (e.g. flood or earthquake) suggest that living through such times is associated with increases in drug use, with a disproportionate effect on those with greater pre-disaster drug use.21,22 Specific to the COVID-19 pandemic, the evidence is variable. However, one cross-sectional study found an increase in participants’ cannabis use23 and a longitudinal study found a progressive increase in Alcohol Use Disorders Identification Test Consumption questionnaire score as the pandemic progressed.24
The COVID-19 pandemic created unique stressors, many of which disproportionately disadvantaged LGBT+ people. Since the start of the pandemic, hate crimes against LGBT+ people in the UK have increased.25 Mental distress, manifesting as anxiety, depression and suicidality has increased among LGBT+ people internationally.26–30 For some, this was in part related to disruptions to HIV-related31 and gender-affirming care.26,32
Pandemic-related financial hardship27 has resulted in many LGBT+ people moving away from their ‘rainbow families’33 and returning to their family of origin. This has brought about an increase in identity concealment which compounds the loss of community connectedness resulting from ‘lockdown’ and other social restrictions. According to minority stress theories, these pandemic-related difficulties disproportionately affected LGBT+ people, contributing to an increase in drug use.34–38 Early research suggests that LGBT+ people who drank to cope with these minority stressors, drank more than before the pandemic.39
Hypothesising a pandemic-associated increase in the frequency and quantity of drug use by LGBT+ people, we conducted a systematic review to synthesise the extant literature reporting changes in drug use in this population to understand if public health and clinical responses require adjustment or upregulation. This review reports findings related to SDU/chemsex among MSM only. The authors felt that the ‘double jeopardy’ of potential SDU-associated HIV acquisition and immune suppression following crystal use40,41 during the COVID-19 pandemic warranted a separate report to ensure these important findings were not lost in a larger review with considerable data.
In this article, we aimed to:
Describe changes in SDU (including increase/decrease in prevalence or frequency; type of drug use; administration route; setting for use) among MSM since the beginning of the pandemic
Explore factors associated with an increase or decrease in the prevalence or frequency of SDU among MSM since the beginning of the pandemic.
Materials and methods
This study was registered on the international prospective register of systematic reviews on 10 August 2021 (PROSPERO: CRD42021271426) and informed by Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) 2020 and extensions PRISMA-S and PRISMA-P.42–44
Search strategy
This study comprised a primary and secondary search. First, eight bibliographic databases (Embase, Epistemonikos, KCI-Journal Database, Medline, PsycINFO, Russian Science Citation Index, SciELO Citation Index, and Web of Science Core Collection) were searched from 1 January 2019 to 14 August 2021 using terms informed by reviewer expertise and previous systematic reviews (see Supplementary Tables S1–S5). Google Scholar was searched three times on 29 August 2021 with terms: ((‘chemsex’ OR ‘drug use’) AND ‘X’), where ‘X’ was ‘COVID*’, ‘coronavirus’ or ‘lockdown’ (Table S6). Four specialist journals in drug use (Addiction, International Journal of Drug Policy) or LGBT+ health (LGBT Health, International Journal of Transgender Health) were hand-searched from March 2019 to August 2021 and a COVID-19 special issue of Journal of Homosexuality screened. Thirteen global key opinion leaders (KOLs) were contacted to request additional published or unpublished work. All potentially relevant records from Google Scholar, handsearching journals and KOLs were read in full. Backward and forward citation searching was completed for each systematic review identified by the search and all texts read in full, using the software ‘citationchaser’.45 This yielded 2037 abstracts. A secondary search was conducted to update the review. This involved a single, focused PubMed search (search two; from 2021) on 9 February 2023 to identify any SDU studies that had been published since the primary search (search one): ((‘sexualised drug use’ OR ‘sexualised drug use’ OR ‘slamsex’ OR ‘hnh’ OR ‘pnp’ OR ‘methamphetamine’ OR ‘GHB’ OR ‘GBL’ OR ‘mephedrone’) AND (‘COVID*’ OR ‘coronavirus’ OR ‘pandemic’ OR ‘lockdown’ OR ‘social restrictions’)).
Inclusion and exclusion criteria
Regional, national, or international studies reporting on adult (≥18 years old) MSM who disclosed SDU during the COVID-19 pandemic were included. Samples with aggregated data for MSM and transgender women were included. Owing to anticipated variation in the definition of chemsex, studies could report on changes in the use of any drug, by any route, in any sexualised context. Primary quantitative, qualitative and mixed-methods studies were eligible with no restriction by study design. Reviews, conference proceedings, book/chapters, commentary articles, editorials, media articles and letters not presenting original data were excluded.
Study selection
Data identified from search one were uploaded to Rayyan, a systematic review software.46 Title-abstract screening was completed by two independent reviewers (DC, GG) and full texts were retrieved when consensus could not be reached. Full texts from all 2021 sources were uploaded to Rayyan and each independently reviewed against the inclusion criteria by two reviewers (DC 100%, EE 50%, GG 50%). Reasons for inclusion/exclusion were documented and disagreements resolved through discussion. Where clarification or additional data were required, study authors were contacted. Results from search two were reviewed twice (DC) against the same inclusion criteria.
Data extraction
A data extraction table was piloted before two independent reviewers (DC, EE) extracted the pre-specified data from included studies identified by search one. The first author extracted data from records identified by search two and these data were reviewed prior to submission.
Data synthesis
Owing to a legal requirement to abstain from SDU/chemsex during pandemic restrictions, studies were allocated to one of two groups: (1) net increase or unchanged SDU/chemsex frequency or duration; and (2) reduced or no SDU/chemsex participation. Groups were summarised separately followed by a description of any factors associated with changes in SDU/chemsex.
Results
Search results and sample characteristics
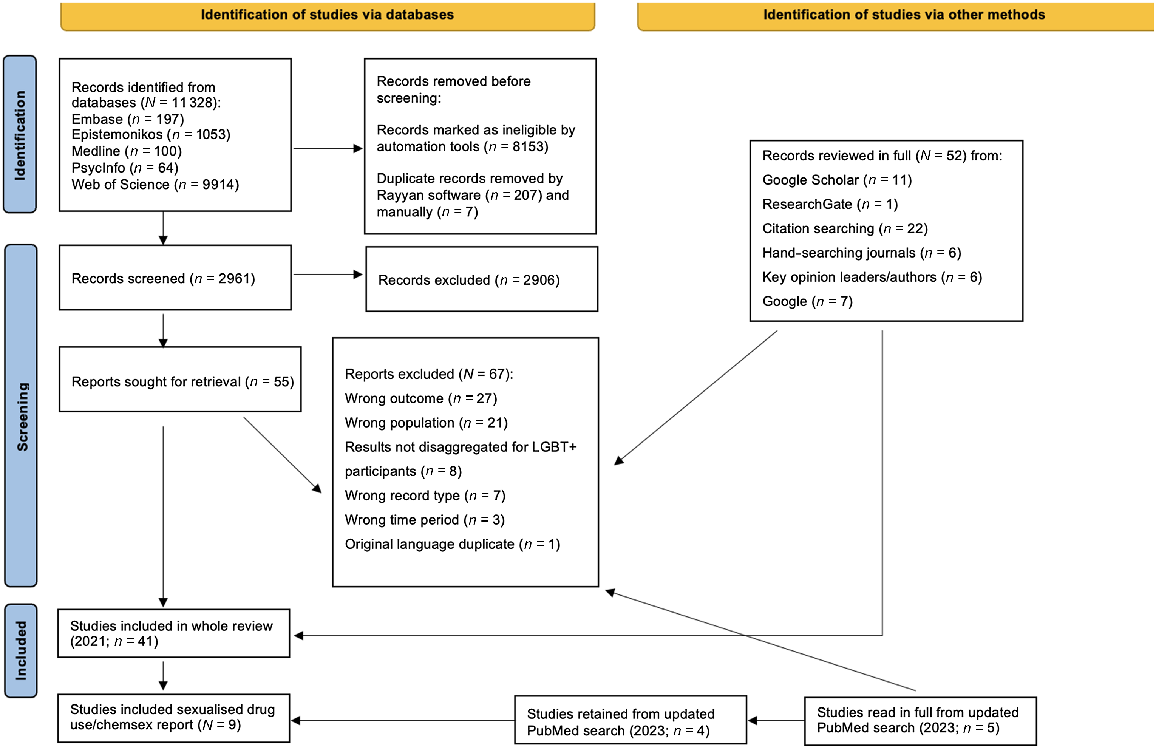
Record selection is in Fig. 1. Across both search one (n = 5) and two (n = 4), nine studies, comprising 5060 MSM and one transgender woman (whose data were aggregated with MSM and therefore retained), met criteria for inclusion in this review. Most studies were small with two-thirds reporting data from fewer than 500 participants (Table 1). Five studies were cross-sectional, three were prospective and one qualitative. Convenience sampling was most common (n = 6; half clinical samples), followed by purposive (n = 3), with one study using both purposive and respondent-driven methods. Included studies were conducted in Australia, China, France, Germany, Israel, Netherlands (n = 2), Singapore and UK. Average age was largely between 30 and 50 years. Lastly, the primary aim of almost half of the included studies was to monitor changes in HIV pre-exposure prophylaxis (PrEP) use and related behaviour during the pandemic.
| Authors (year) | Country | Primary aim | SDU definition | Sampling method | Sample size and characteristics | Age (years) | Study design | |
|---|---|---|---|---|---|---|---|---|
| Chow et al. (2021) 47 | Australia | To understand if MSM changed their PrEP use and sexual behaviour in July–August 2020 (second lockdown) compared with May–June 2020 (post-first lockdown) | Drug use before and/or during sex (chemsex) | Convenience (clinical) | N = 192; 60% born in Australia; med time taking PrEP was 35 (IQR 17–47) months | Med: 38 IQR: 32–49 | Cross-sectional | |
| de la Court et al. (2022) 49 | Netherlands | To assess if the pandemic impacted MSM’s return to clinic for PrEP and STI care during COVID-19-related restrictions | Any drug use during sex (chemsex) | Purposive | The AMPrEP participants included in the analysis (n = 305) were mainly highly educated, white and exclusively MSM | Med: 45 IQR: 38–53 | Prospective cohort | |
| Hyndman et al. (2021) 52 | United Kingdom | To understand the influence of COVID-19 on sexual behaviour of SHS-engaged MSM signed up to an online HIV risk-reduction service | Sexualised recreational drug use (chemsex) | Convenience (clinical) | N = 814 (612 PrEP users; 157 chemsex participants). 83.3% white | Med: 40 IQR: 33–48 | Cross-sectional | |
| L’Yavanc et al. (2022) 48 | France | To measure changes in chemsex participation among MSM after the second lockdown (30/10/2020 to 15/12/2020) and factors associated with continued or increased chemsex practice | Use of drugs, including cathinones, GHB/GBL, methamphetamine, cocaine, or other drugs, during or just before sex (chemsex) | Convenience | N = 86 MSM with a history of chemsex participation (n = 61, 66% LWHIV; n = 15, 15% HCV positive; n = 30, 33% stable relationship; n = 52, 56% recent group sex; n = 31, 33% used chemsex drugs alone) | Med: 38 IQR: 33–48 | Prospective cohort | |
| Shilo and Mor (2020) 53 | Israel | To assess mental health and sexual behaviour of MSM during social distancing and to compare behaviours before and during COVID-19 social restrictions | Alcohol/other drug use before or during sex | Convenience (appA/social network) | N = 2562 (n = 1970, 76.9% gay; n = 551, 21.5% bisexual; n = 41, 1.6%, HMSM) | : 37 s.d.: 11.3 | Cross-sectional | |
| Tan et al. (unpubl. data) | Singapore | To understand the impact of COVID-19 on mental health, substance use and sexual health among MSM | NR | Purposive | N = 16 (n = 14 gay; n = 1 bisexual; n = 1 queer) | NR | Qualitative (IDI) | |
| Uhrmacher et al. (2022) 54 | Germany | To understand the relationship between the pandemic onset and PrEP uptake and sexual behaviour | Psychoactive substances consumed during sex | Convenience (clinical) | N = 138 PrEP-using MSM (n = 7 MSMW; n = 124, 90% employed/in education; n = 119, 86.2% Germany-born; n = 86, 63.3% prev. STI) | : 33.9 s.d.: 10.1 | Prospective observational | |
| van Bilsen et al. (2021) 51 | Netherlands | To measure the impact of COVID-19 social restrictions on sexual behaviour and HIV/STI acquisition among ACS participants | Use of GHB/GBL, (meth)amphetamine, mephedrone, ketamine, cocaine, ecstasy, 2,5-dimethoxy-4-bromophenethylamine, or 4-fluoroamphetamine around sex (chemsex) | Convenience (from cohort) | N = 353 (n = 304, 86% born in NL; n = 275, 78% college education; n = 236, 67% in relationship; n = 11, 3% living with HIV) | Med: 47 IQR: 38–53 | Cross-sectional | |
| Zhang et al. (2022) 50 | China | To report the different HIV testing techniques used by MSM across three time periods, including before and during COVID-19-related restrictions | Use of ketamine, methamphetamine, cocaine, cannabis, ecstasy, Dormicum/Halcion/Erimin 5/non-prescription hypnotic drugs, heroin, cough suppressant (not for curing cough), GHB/GBL, 5-methocy-N,N-diisopropyltryptamine (Foxy), or mephedrone before or during sex (SDU) | Purposive and respondent-driven | N = 595 (n = 427, 72% homosexual, n = 117, 20% bisexual; n = 18 3% HMSM; n = 33, 6% uncertain of orientation; 453, 75.9% 18–30 years; 481, 80.2% single; 433, 72.8% employed full-time; 394, 66.2% tertiary education) | Mode: 18–30 years (n = 452, 75.9%) | Cross-sectional |
ACS, Amsterdam cohort study; HIV, human immunodeficiency virus; IDI, in-depth interviews; IQR, interquartile range; Med, median; GHB/GBL, γ-hydroxybutyrate/γ-butyrolactone; HCV, hepatitis C virus; (LW)HIV, (living with) human immunodeficiency virus; (H)MSM, (heterosexual) men who have sex with men; MSMW, men who have sex with men and women; NL, Netherlands; NR, not reported; OR, odds ratio; PrEP, pre-exposure prophylaxis; s.d., standard deviation; SHS, sexual health service; STI, sexually transmitted infection.
AGeospatial networking application.
Changes in SDU following the onset of the pandemic
Four records reported a net maintenance or increase in SDU participation (Table 2). In an Australian study of PrEP-using MSM, 21% continued chemsex participation during social restrictions. Fifteen percent increased and 6% decreased chemsex participation during Australia’s second lockdown, relative to after the first lockdown.47
| Authors (year) | Study findings | |
|---|---|---|
| Increased or unchanged SDU prevalence or frequency | ||
| Chow et al. (2021)47 | Most men did not participate in chemsex (79%). Of those who did, 3% increased the number of chemsex events they attended in the second lockdown relative to immediately after the first. 6% decreased. 12% reported no change in the frequency of chemsex participation | |
| de la Court et al. (2022)49 | Almost half of survey respondents in wave 1 (15/03/20–15/06/20; n = 82, 40.4%), wave 2 (until 15/09/20; n = 75, 46.9%) and wave 3 (until 31/12/20; n = 73 45.6%) reported chemsex participation during COVID-19 restrictions and more than half the respondents reported that chemsex participation had escalated (wave 1: n = 57, 50.9%; wave 2: n = 44, 58.7%; wave 3: n = 41, 56.2%) | |
| L’Yavanc et al. (2022)48 | Compared to 6 weeks before lockdown, n = 31 (36%) participants declared they had stopped (n = 12, 14%) or decreased (n = 19, 22%) their chemsex participation, during 6 weeks of lockdown. Most (n = 55, 64%) reported they maintained (n = 19, 22%) or increased (n = 36, 42%) their drug use during lockdown. During lockdown, there was a significant increase in GHB/GBL consumption (52% to 58%, P = 0.038) and the number of days participants consumed chemsex drugs over the 6 weeks before (med 3, IQR 2–6) and during (med 8, IQR 3–15) lockdown (P < 0.001). Slamming prevalence increased from 19% to 24% (n.s.). Loneliness (OR 3.53, 95% CI 1.16–10.74, P = 0.03), cravings (OR 4.51, 95% CI 1.38–14.72, P = 0.01) and working (OR 3.82, 95% CI 1.05–13.96, P = 0.04) during the lockdown were associated with maintained or increased chemsex participation during lockdown. Fear of COVID-19 was associated with decreasing chemsex frequency (OR 0.25, 95% CI 0.07–0.90, P = 0.03). In order of decreasing prevalence of use: cathinones, GHB/GBL, cocaine, methamphetamine were most commonly reported chemsex drugs | |
| Zhang et al. (2022)50 | SDU prevalence increased from n = 57 (9.6%) before COVID-19 (November 2019–January 2020) to n = 67 (11.3%) following onset of COVID restrictions (February–July 2020) | |
| Decreased SDU prevalence or frequency (including no participation) | ||
| Hyndman et al. (2021)52 | 19.3% participated in chemsex during lockdown. Compared with usual (i.e. pre-pandemic), 26.8% had more and 66.9% had less chemsex during lockdown. 6.4% began chemsex participation during lockdown. Participants who used PrEP during lockdown were significantly more likely to have chemsex than those who did not (P = 0.01). 14.1% of participants said their reason for sex outside household was seeking chemsex | |
| Shilo and Mor (2020)53 | SDU was reported by fewer MSM during social distancing (n = 249, 24.6%) than before (n = 321, 31.7%). SAU was reported by fewer MSM during social distancing (n = 322, 31.8%) than before (n = 420, 41.5%). SDU was twice as common among MSM who had casual sex during lockdown. MSM who had casual sex were 60% more likely to report SAU than those who did not. | |
| Tan et al. (unpubl. data) | Suggestion that SDU frequency decreased: ‘We cannot interact in any other ways other than online … for us gay guys we definitely use drugs for sex, because of COVID we are not able to meet up there’s a lot of restrictions, we are only using it at our own end.’ | |
| Uhrmacher et al. (2022)54 | Across four quarters of 2020, 55.9–67.4% PrEP users reported SDU. SAU was most common (32.0–43.6%), then poppers (27.1–31.9%), cannabis (12.7–17.9%), PDE-5i (11.9–17.9%) and ecstasy (4.0–7.6%). In 2020, 0.8–4.2% consumed a chemsex drug. In 2018, 72–73.9% reported any SDU: alcohol (45.5–51.4%), poppers (47.8–60.3%), PDE5i (27.3–35.9%), cannabis (13.6–21.7%), ketamine (up to 6.5%). 12.1% reported use of ecstasy, cocaine and GHB/GBL. SDU declined during pandemic (2020) compared with pre-pandemic (2018). | |
| van Bilsen et al. (2021)51 | 92 (26%) reported chemsex in the pre–COVID-19 period and 69 (20%) during COVID-19 | |
CI, confidence interval; GHB/GBL, γ-hydroxybutyrate/γ-butyrolactone; IQR, interquartile range; MSM, men who have sex with men; n.s., not significant; OR, odds ratio; PDE5i, phosphodiesterase 5 inhibitors; PrEP, pre-exposure prophylaxis; SAU, sexualised alcohol use; SDU, sexualised drug use.
A French study of chemsex behaviour during lockdown found that 64% of participants maintained (22%) or increased (42%) while 36% stopped (14%) or decreased (22%) their chemsex drug consumption during lockdown.48 They also found that the median number of chemsex days during 6 weeks of lockdown (n = 8) increased significantly from the 6 weeks preceding lockdown (n = 3).48 The prevalence of GHB/GBL use (52% vs 58%, P = 0.038) and slamming (19% vs 24%) both increased though the latter was not statistically significant.48
Across three waves of follow-up, corresponding to three episodes of pandemic-related restrictions, between 40.4% and 46.9% of a PrEP-using cohort reported chemsex participation.49 Of these, between 50.9% and 58.7% reported that their participation had increased during restriction periods.49 Lastly, the prevalence of SDU in a Chinese sample presenting for HIV testing throughout the pandemic rose from 9.6% before to 11.3% after the outbreak.50
Five studies reported a net decrease in SDU following the onset of the pandemic. One cohort study reported that chemsex prevalence fell from 26% to 20% during lockdown.51 A UK-based study found similarly, reporting that 20% of their sampled sexual health service attendees continued with chemsex participation. Of these, two-thirds decreased while 26.8% increased chemsex participation. A further 6.4% newly began chemsex practice.52
In another article reporting lockdown-associated changes in patterns of casual sex in Israel, fewer men participated in SDU (24.6% vs 31.7%) and sexualised alcohol use (SAU; 31.8% vs 41.5%) during social restrictions than before.53 A German study asked MSM to report SDU for each quarter of 2018 (72.0–73.9%) and 2020 (55.9–67.4%). Each measure of SDU decreased in frequency in 2020, relative to 2018.54 In the sole qualitative report, there was no mention of increased SDU during the pandemic. However, one participant disclosed ‘We cannot interact in any other ways other than online...for us gay guys we definitely use drugs for sex, because of COVID we are not able to meet up there’s a lot of restrictions, we are only using it at our own end’ (RKJ Tan, unpubl. data).
Factors associated with changes in SDU following the onset of the pandemic
PrEP use was associated with SDU in two studies.49,52 In one, chemsex participation during lockdown was associated with using PrEP (16.2% vs 6.1%, P < 0.01). This study also found chemsex to be a strong motivator for sex outside the household (reported by 14.1% of participants). In another, where each wave of follow-up took place after a period of pandemic-related restrictions, chemsex was associated with unchanged or increased PrEP use in waves one (adjusted odds ratio (aOR) 2.79, P < 0.001) and three (aOR 2.19, P < 0.020).49
SDU was reported to be twice as common and SAU 60% more common among those having casual sex during a lockdown period.53 Lastly, experiencing loneliness (OR 3.53, 95% CI 1.16–10.74, P = 0.03) or cravings (OR 4.51, 95% CI 1.38–14.72, P = 0.01) and working (OR 3.82, 95% CI 1.05–13.96, P = 0.04) were all associated with maintained of increased chemsex participation during COVID-19 social restrictions. Fear of COVID-19 was associated with decreased chemsex participation (OR 0.25, 95% CI 0.07–0.90, P = 0.03).48
Discussion
Key findings
In the context of a need for total lockdown to limit the spread of COVID-19, four studies estimated that ~20% participants engaged in SDU, including chemsex, during social restrictions.47,51–53 Several studies reported a significant increase in SDU participation during lockdown with one investigating chemsex-practicing MSM finding that more than 60% maintained or increased this practice. One study reported the number of chemsex events attended, suggesting sex with non-cohabitant partners.49 However, the context of SDU is not specified in other studies. This is a significant omission because the risk of COVID-19, STI and HIV acquisition when participating in SDU with new partners outside the home was much greater than SDU practice with a regular partner in a shared household or with partners on videoconferencing software.55
Few correlates were identified. However, two identified that PrEP use was associated with chemsex participation. Given the prevalence of PrEP use among the whole sample, it is possible that these studies provide an inflated estimate of chemsex participation during the pandemic.52 In another study, loneliness, craving and working during the pandemic were all strongly associated with chemsex participation.48 Conversely, those reporting greater fear of COVID-19 were less likely to participate in chemsex.48
Findings in context
The wider literature confirms that chemsex practice did not cease during the pandemic with studies reporting prevalence (but not change) suggesting significant participation in Portugal (20.2%) and Brazil (39.1%), throughout lockdown periods, consistent with the findings of this review.56–58 This may be, in part, related to the perceived increase in difficulty getting help with crystal reduction among those using in a sexualised context59 or simply a consequence of the pandemic-associated freedoms (i.e. time away from work) facilitating more frequent drug use.60 The exact cause is likely multifactorial and individual-specific.
To the best of the authors’ knowledge, SDU has not been investigated in the context of other natural disasters, nor among cisgender and heterosexual couples during the COVID-19 pandemic. However, the impact of COVID-19 on the use of other drugs has been investigated. Participants in these studies were also more likely to report an increase (9.9%) than decrease (6.8%) in use of other illicit drugs61 and there were reports of substantial increases in cannabis62 and alcohol use,63–65 with one study reporting an 82.6% increase in number of drinks participants consumed in the 30 days preceding assessment.64 Contrary to findings of this review, fear of COVID-19 was associated with near 20-fold increased probability of increased alcohol use.66 It is possible that COVID-19-related fear resulted in different patterns of alcohol consumption and SDU because of the differing risk of COVID-19 acquisition in their respective contexts.
Strengths and limitations
This review was adherent to a pre-specified protocol and informed by the PRISMA 2020 statement and both PRISMA-P and PRISMA-S extensions.42–44 The primary search strategy was comprehensive, peer reviewed, had no restrictions and was informed by input from KOLs. However, the heterogeneity in sample composition (e.g. all PrEP users or men with a history of chemsex participation) and its poor generalisability precluded quantitative meta-synthesis.
Implications for research, policy, and practice
Overall, there was little research reporting changes in SDU during the pandemic. SDU was a secondary outcome in all but one study which investigated participants with a history of chemsex participation.48 Only one unpublished, qualitative report was identified (RKJ Tan, unpubl. data). Further qualitative work is required to understand motivations for SDU participation and abstinence during the COVID-19 pandemic and to identify targets for intervention. The association between PrEP use and SDU represents a potential concern and further work is required to understand if this association is bidirectional. If so, SDU screening and harm reduction interventions may be required on PrEP initiation and follow-up. Additional work is required to understand the nature of pandemic-associated changes in SDU in terms of drugs used, routes of administration and harms experienced so that existing interventions can be adapted, as required. Pandemic-related changes may suggest a need for trauma-informed interventions moving forward.
At the height of the COVID-19 pandemic, there was reduced testing for STIs and access to, particularly parenteral, treatment.67 Since high-risk behaviour continued, policymakers and clinicians should consider providing STI chemoprophylaxis (i.e. doxycycline P(r)EP) to those at greatest risk in the event of future similar disasters.68,69 Postal needle exchange and STI testing services should be evaluated to inform future provision.
People living with HIV who participate in SDU are more likely to report sub-optimal anti-retroviral therapy (ART) adherence and therefore require additional support.70 Widespread disruptions to HIV service delivery reported during the pandemic71 may have exacerbated difficulties engaging with ART care among a population reporting high-risk sex and intravenous drug use. HIV transmission may have increased among SDU participants. Assertive outreach is required to ensure people who have disengaged in testing or ART care due to SDU participation are re-engaged.
Conclusion
Chemsex practice continued, and for some MSM increased, throughout COVID-19 pandemic lockdowns. This may have contributed to increased COVID-19 transmission and severity among these potentially vulnerable people.
References
1 Saunders CL, MacCarthy S, Meads C, Massou E, Mant J, Saunders AM, et al. Long-term conditions among sexual minority adults in England: evidence from a cross-sectional analysis of responses to the English GP Patient Survey. BJGP Open 2021; 5(5): BJGPO.2021.0067.
| Crossref | Google Scholar |
2 King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry 2008; 8: 70.
| Crossref | Google Scholar |
3 Connolly D, Gilchrist G. Prevalence and correlates of substance use among transgender adults: a systematic review. Addict Beha 2020; 111: 106544.
| Crossref | Google Scholar |
4 Bloomfield K, Wicki M, Wilsnack S, Hughes T, Gmel G. International differences in alcohol use according to sexual orientation. Subst Abus 2011; 32(4): 210-9.
| Crossref | Google Scholar |
5 Demant D, Hides L, Kavanagh DJ, White KM, Winstock AR, Ferris J. Differences in substance use between sexual orientations in a multi-country sample: findings from the Global Drug Survey 2015. J Public Health 2017; 39(3): 532-41.
| Crossref | Google Scholar |
6 Kerr DL, Ding K, Chaya J. Substance use of lesbian, gay, bisexual and heterosexual college students. Am J Health Behav 2014; 38(6): 951-62.
| Crossref | Google Scholar |
7 Lea T, Reynolds R, De Wit J. Alcohol and club drug use among same-sex attracted young people: associations with frequenting the lesbian and gay scene and other bars and nightclubs. Subst Use Misuse 2013; 48(1–2): 129-136.
| Crossref | Google Scholar |
8 Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, et al. Sexual orientation and adolescent substance use: a meta-analysis and methodological review. Addiction 2008; 103(4): 546-56.
| Crossref | Google Scholar |
9 Edmundson C, Heinsbroek E, Glass R, Hope V, Mohammed H, White M, et al. Sexualised drug use in the United Kingdom (UK): a review of the literature. Int J Drug Policy 2018; 55: 131-48.
| Crossref | Google Scholar |
10 Lawn W, Aldridge A, Xia R, Winstock AR. Substance-linked sex in heterosexual, homosexual, and bisexual men and women: an online, cross-sectional “Global Drug Survey” report. J Sex Med 2019; 16(5): 721-32.
| Crossref | Google Scholar |
11 Stuart D. Chemsex: origins of the word, a history of the phenomenon and a respect to the culture. Drugs Alcohol Today 2019; 19(1): 3-10.
| Crossref | Google Scholar |
12 Goldsmith D, Hillyard M. The lack of focus on trans women in a themed issue of the International Journal of Drug Policy on sexualised drug use. Int J Drug Policy 2019; 68: 1-2.
| Crossref | Google Scholar |
13 Hibbert MP, Hillis A, Brett CE, Porcellato LA, Hope VD. A narrative systematic review of sexualised drug use and sexual health outcomes among LGBT people. Int J Drug Policy 2021; 93: 103187.
| Crossref | Google Scholar |
14 Bourne A, Reid D, Hickson F, Torres-Rueda S, Steinberg P, Weatherburn P. “Chemsex” and harm reduction need among gay men in South London. Int J Drug Policy 2015; 26(12): 1171-6.
| Crossref | Google Scholar |
15 Kohli M, Hickson F, Free C, Reid D, Weatherburn P. Cross-sectional analysis of chemsex drug use and gonorrhoea diagnosis among men who have sex with men in the UK. Sex Health 2019; 16(5): 464-72.
| Crossref | Google Scholar |
16 Howarth AR, Apea V, Michie S, Morris S, Sachikonye M, Mercer CH, et al. The association between use of chemsex drugs and HIV clinic attendance among gay and bisexual men living with HIV in London. HIV Med 2021; 22(8): 641-9.
| Crossref | Google Scholar |
17 Schreck B, Victorri-Vigneau C, Guerlais M, Laforgue E, Grall-Bronnec M. Slam practice: a review of the literature. Eur Addict Res 2021; 27(3): 161-78 PMID:.
| Crossref | Google Scholar | PubMed |
18 Moreno-Gámez L, Hernández-Huerta D, Lahera G. Chemsex and psychosis: a systematic review. Behavioral Sciences 2022; 12(12): 516.
| Crossref | Google Scholar |
19 Wilkerson JM, Di Paola A, Nieto D, Schick V, Latini DM, Braun-Harvey D, et al. Sexual violence and chemsex among substance-using sexual and gender minorities in Texas. Subst Use Misuse 2021; 56(14): 2141-50.
| Crossref | Google Scholar |
20 Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed 2020; 91(1): 157-60.
| Crossref | Google Scholar |
21 North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Arch Gen Psychiatry 2011; 68(2): 173-80.
| Crossref | Google Scholar |
22 Heslin KC, Stein JA, Dobalian A, Simon B, Lanto AB, Yano EM, et al. Alcohol problems as a risk factor for postdisaster depressed mood among U.S. veterans. Psychol Addict Behav 2013; 27(1): 207-13.
| Crossref | Google Scholar |
23 van Laar MW, Oomen PE, van Miltenburg CJA, Vercoulen E, Freeman TP, Hall WD. Cannabis and COVID-19: reasons for Concern. Front Psychiatry 2020; 11: 601653.
| Crossref | Google Scholar |
24 Irizar P, Jones A, Christiansen P, Goodwin L, Gage SH, Roberts C, et al. Longitudinal associations with alcohol consumption during the first COVID-19 lockdown: associations with mood, drinking motives, context of drinking, and mental health. Drug Alcohol Depend 2021; 226: 108913.
| Crossref | Google Scholar |
26 Kidd JD, Jackman KB, Barucco R, Dworkin JD, Dolezal C, Navalta TV, et al. Understanding the impact of the COVID-19 pandemic on the mental health of transgender and gender nonbinary individuals engaged in a longitudinal cohort study. J Homosex 2021; 68(4): 592-611.
| Crossref | Google Scholar |
27 Moore SE, Wierenga KL, Prince DM, Gillani B, Mintz LJ. Disproportionate impact of the COVID-19 pandemic on perceived social support, mental health and somatic symptoms in sexual and gender minority populations. J Homosex 2021; 68(4): 577-91.
| Crossref | Google Scholar |
28 Flentje A, Obedin-Maliver J, Lubensky ME, Dastur Z, Neilands T, Lunn MR. Depression and anxiety changes among sexual and gender minority people coinciding with onset of COVID-19 pandemic. J Gen Intern Med 2020; 35(9): 2788-90.
| Crossref | Google Scholar |
29 Salerno JP, Shrader CH, Algarin AB, Lee JY, Fish JN. Changes in alcohol use since the onset of COVID-19 are associated with psychological distress among sexual and gender minority university students in the U.S. Drug Alcohol Depend 2021; 221: 108594.
| Crossref | Google Scholar |
30 Peterson ZD, Vaughan EL, Carver DN. Sexual identity and psychological reactions to COVID-19. Traumatology 2021; 27(1): 6-13.
| Crossref | Google Scholar |
31 Santos GM, Ackerman B, Rao A, Wallach S, Ayala G, Lamontage E, et al. Economic, mental health, HIV prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of cisgender gay men and other men who have sex with men. AIDS Behav 2021; 25(2): 311-21.
| Crossref | Google Scholar |
32 Wang Y, Pan B, Liu Y, Wilson A, Ou J, Chen R. Health care and mental health challenges for transgender individuals during the COVID-19 pandemic. Lancet Diabetes Endocrinol 2020; 8(7): 564-5.
| Crossref | Google Scholar |
33 Bleckmann C, Leyendecker B, Busch J. Sexual and gender minorities facing the coronavirus pandemic: a systematic review of the distinctive psychosocial and health-related impact. J Homosex 2022; 1-22.
| Crossref | Google Scholar |
35 Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003; 129(5): 674-97.
| Crossref | Google Scholar |
36 Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the minority stress model. Prof Psychol Res Pr 2012; 43(5): 460-7.
| Crossref | Google Scholar |
37 Tan KKH, Treharne GJ, Ellis SJ, Schmidt JM, Veale JF. Gender minority stress: a critical review. J Homosex 2020; 67(10): 1471-89.
| Crossref | Google Scholar |
38 Lefevor GT, Boyd-Rogers CC, Sprague BM, Janis RA. Health disparities between genderqueer, transgender, and cisgender individuals: an extension of minority stress theory. J Couns Psychol 2019; 66(4): 385-95.
| Crossref | Google Scholar |
39 Surace A, Kang A, Operario D, Kahler CW. How the loss of gay spaces has impacted alcohol use among sexual minorities during the COVID-19 pandemic. Alcohol Clin Exp Res 2021; 45: 259A-260A.
| Google Scholar |
40 Hossain MK, Hassanzadeganroudsari M, Apostolopoulos V. Why METH users are at high risk of fatality due to COVID-19 infection? Expert Rev Vaccines 2020; 19(12): 1101-3.
| Crossref | Google Scholar |
41 Carrico AW, Horvath KJ, Grov C, Moskowitz JT, Pahwa S, Pallikkuth S, et al. Double jeopardy: methamphetamine use and HIV as risk factors for COVID-19. AIDS Behav 2020; 24(11): 3020-3.
| Crossref | Google Scholar |
42 Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA Statement for reporting literature searches in systematic reviews. Syst Rev 2021; 10(1): 39.
| Crossref | Google Scholar |
43 Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021; 372: n160.
| Crossref | Google Scholar |
44 Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015; 349: g7647.
| Crossref | Google Scholar |
45 Haddaway NR, Grainger MJ, Gray CT. Citationchaser: a tool for transparent and efficient forward and backward citation chasing in systematic searching. Res Synth Methods 2022; 13(4): 533-45.
| Crossref | Google Scholar |
46 Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016; 5(1): 210.
| Crossref | Google Scholar |
47 Chow EPF, Hocking JS, Ong JJ, Phillips TR, Schmidt T, Buchanan A, et al. Changes in PrEP use, sexual practice, and use of face mask during sex among MSM during the second wave of COVID-19 in Melbourne, Australia. J Acquir Immune Defic Syndr 2021; 86: 153-6.
| Crossref | Google Scholar |
48 L’Yavanc T, Gosset D, Platey M, Jedrzejewski T, Gazalet P, Lasry S, et al. Is there a reduction in chemsex practice in men who have sex with men during Covid-19 lockdown? Results of the CheRRLock study. J Acquir Immune Defic Syndr 2023; 92(5): 378-84.
| Crossref | Google Scholar |
49 de la Court F, Boyd A, Coyer L, van den Elshout M, de Vries HJC, Matser A, et al. The impact of COVID-19-related restrictions in 2020 on sexual healthcare use, pre-exposure prophylaxis use, and sexually transmitted infection incidence among men who have sex with men in Amsterdam, the Netherlands. HIV Med 2023; 24(2): 212-23.
| Crossref | Google Scholar |
50 Zhang KC, Fang Y, Cao H, Chen H, Hu T, Chen YQ, et al. The impacts of the COVID-19 pandemic on HIV testing utilization among men who have sex with men in China: Cross-sectional online survey. JMIR Public Health Surveill 2022; 8(5): e30070.
| Crossref | Google Scholar |
51 van Bilsen WPH, Zimmermann HML, Boyd A, Coyer L, van der Hoek L, Kootstra N, et al. Sexual behavior and Its determinants during COVID-19 restrictions among men who have sex with men in Amsterdam. J Acquir Immune Defic Syndr 2021; 86(3): 288-96.
| Crossref | Google Scholar |
52 Hyndman I, Nugent D, Whitlock GG, Mcowan A, Girometti N. COVID-19 restrictions and changing sexual behaviours in HIV-negative MSM at high risk of HIV infection in London, UK. Sex Transm Infect 2021; 97: 521-4.
| Crossref | Google Scholar |
53 Shilo G, Mor Z. COVID-19 and the changes in the sexual behavior of men who have sex with men: Results of an online survey. J Sex Med 2020; 17(10): 1834.
| Crossref | Google Scholar |
54 Uhrmacher M, Skaletz-Rorowski A, Nambiar S, Schmidt AJ, Ahaus P, Serova K, et al. HIV pre-exposure prophylaxis during the SARS-CoV-2 pandemic: Results from a prospective observational study in Germany. Front Public Health 2022; 10: 930208.
| Crossref | Google Scholar |
55 Florêncio J. Chemsex cultures: subcultural reproduction and queer survival. Sexualities 2021; 136346072098692.
| Crossref | Google Scholar |
56 Chone JS, Lima SVMA, Fronteira I, Mendes IAC, Shaaban AN, Martins MRO, et al. Fatores associados à prática de chemsex em Portugal durante pandemia de COVID-19. Rev. Latino-Am. Enfermagem 2020; 29: e3474.
| Crossref | Google Scholar |
57 Sousa AFL de, Oliveira LB de, Queiroz AAFLN, Carvalho HEF de, Schneider G, Camargo ELS, et al. Casual sex among men who have sex with men (MSM) during the period of sheltering in place to prevent the spread of COVID-19. Int J Environ Res Public Health 2021; 18(6): 3266.
| Crossref | Google Scholar |
58 Sousa AFL de, Queiroz AAFLN, Lima SVMA, Almeida PD, Oliviera LB de, Chone JS, et al. Chemsex practice among men who have sex with men (MSM) during social isolation from COVID-19: Multicentric online survey. Cad Saude Publica 2020; 36(12): e00202420.
| Crossref | Google Scholar |
59 Card K, McGuire M, Bond-Gorr J, Nguyen T, Wells GA, Fulcher K, et al. Perceived difficulty of getting help to reduce or abstain from substances among sexual and gender minority men who have sex with men (SGMSM) and use methamphetamine during the early period of the COVID-19 pandemic. Subst Abuse Treat Prev Policy 2021; 16(1): 88.
| Crossref | Google Scholar |
60 Harkness A, Weinstein ER, Atuluru P, Vidal R, Rodriguez-Diaz CE, Safren SA. “Let’s Hook Up When the Pandemic is Over:” Latinx sexual minority men’s sexual behavior during COVID-19. J Sex Res 2021; 58(8): 951-7.
| Crossref | Google Scholar |
61 Sanchez TH, Zlotorzynska M, Rai M, Baral SD. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav 2020; 24(7): 2024-32.
| Crossref | Google Scholar |
62 Krueger EA, Barrington-Trimis JL, Unger JB, Leventhal AM. Sexual and gender minority young adult coping disparities during the COVID-19 pandemic. J Adolesc Health 2021; 69(5): 746-53.
| Crossref | Google Scholar |
63 Fish JN, Salerno J, Williams ND, Gordon Rinderknecht R, Drotning KJ, Sayer L, et al. Sexual minority disparities in health and well-being as a consequence of the COVID-19 pandemic differ by sexual identity. LGBT Health 2021; 8(4): 263-72.
| Crossref | Google Scholar |
64 Coakley KE, Lardier DT, Holladay KR, Amorim FT, Mechler H, Zuhl MN. Mental health severity is associated with increases in alcohol consumption in young adult students during the COVID-19 Pandemic. Alcohol Treat Q 2021; 39(3): 328-41.
| Crossref | Google Scholar |
66 Jacques-Aviñó C, López-Jiménez T, Medina-Perucha L, de Bont J, Berenguera A. Social conditions and mental health during COVID-19 lockdown among people who do not identify with the man/woman binomial in Spain. PLoS ONE 2021; 16(8): e0256261.
| Crossref | Google Scholar |
67 Pinto CN, Niles JK, Kaufman HW, Marlowe EM, Alagia DP, Chi G, et al. Impact of the COVID-19 pandemic on chlamydia and gonorrhea screening in the U.S. Am J Prev Med 2021; 61(3): 386-93.
| Crossref | Google Scholar |
68 Grant JS, Stafylis C, Celum C, Grennan T, Haire B, Kaldor J, et al. Doxycycline prophylaxis for bacterial sexually transmitted infections. Clin Infect Dis 2020; 70(6): 1247-53.
| Crossref | Google Scholar |
69 Cornelisse VJ, Ong JJ, Ryder N, Ooi C, Wong A, Kenchington P, et al. Interim position statement on doxycycline post-exposure prophylaxis (Doxy-PEP) for the prevention of bacterial sexually transmissible infections in Australia and Aotearoa New Zealand – the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM). Sex Health 2023; 20(2): 99-104.
| Crossref | Google Scholar |
70 Perera S, Bourne AH, Thomas S. P198 Chemsex and antiretroviral therapy non-adherence in HIV-positive men who have sex with men: a systematic review. Sex Transm Infect 2017; 93(Suppl 1): A81.
| Crossref | Google Scholar |
71 Brazier E, Ajeh R, Maruri F, Musick B, Freeman A, Wester CW, et al. Service delivery challenges in HIV care during the first year of the COVID-19 pandemic: Results from a site assessment survey across the global IeDEA consortium. J Int AIDS Soc 2022; 25(12): e26036.
| Crossref | Google Scholar |