How do general practitioners persuade parents to vaccinate their children? A study using standardised scenarios
Julie LeaskA National Centre for Immunisation Research and Surveillance of Vaccine Preventable Diseases, The Children’s Hospital at Westmead
B Discipline of Paediatrics and Child Health, University of Sydney
C School of Public Health, University of Sydney
D Email: JulieL3@chw.edu.au
NSW Public Health Bulletin 20(8) 119-124 https://doi.org/10.1071/NB08064
Published: 7 September 2009
Abstract
Objective: To understand how general practitioners (GPs) address parental concerns about childhood immunisation using standardised scenarios. Methods: A combination of typical case and intensity sampling was used to recruit GPs. Interviews began with role-play vignettes of four different scenarios, exemplifying concerns about immunisation and the parents who have them. They ended with GPs’ reflections on these encounters. Transcripts were analysed with the focus on describing and evaluating typical persuasive strategies. Results: Eleven GPs were interviewed from a range of demographic areas. In the role plays, GPs acknowledged the mother’s concerns, tailored their discussion to her individual circumstances, and conveyed the notion of choice. Theoretical frameworks guided some in their responses. Less successful strategies were to enter into games of scientific ‘ping pong’; to discredit a mother’s source of information; or to ask confronting hypothetical questions. Attempts to negotiate with a mother refusing all vaccines for her children proved to be the most challenging role play. Conclusions: GPs tended to adopt the role of persuader rather than informer. Communication frameworks such as shared decision-making may help them to better balance these roles.
The analysis of health care communication has been a growing area of interest for qualitative researchers. It has required methods of data collection that access discussions that occur between patients and health professionals. Video or audio-assisted observations of actual patient encounters have been used.1,2 Another approach uses standardised patients. These are people who act out a set patient scenario with a clinician.3 A widely used assessment tool in medical education, standardised patients have been increasingly used in qualitative research of doctor–patient communication.4–6 This study used this method to attempt to describe how general practitioners (GPs) communicate with parents concerned about immunisation.
Discussions about immunisation occur frequently in face-to-face encounters between a health professional and a parent.7 These discussions are key since health professionals are the single most important influence on a parent’s decision to immunise or not immunise their children.8–11 Health professionals have a public health responsibility to maximise childhood immunisation rates. They are also faced with ethical and legal obligations to ensure that parents are adequately informed about the risks and benefits of immunisation and that valid consent is given before a vaccine is administered.
This study investigated the ways GPs communicate about vaccine risk and benefit to parents who have strong concerns about immunisation. GPs were chosen because they represented 85% of immunisation providers in NSW at the time of the study.
Methods
The study sought to assess the strategies GPs used when communicating with parents. To achieve the study’s aims, direct observation of actual conversations with parents would have been the ideal method but this was costly and impractical. A second option was to talk to GPs about their experiences of communicating with parents, yet this approach was likely to result in a polemic on what GPs think ‘should’ happen. A middle ground was the choice of standardised patients, which would allow both an assessment of the GP’s rhetoric and a way into the GP’s own reflection of their experiences.
Ethical approval to conduct this study was gained from the University of Sydney Human Research Ethics Committee.
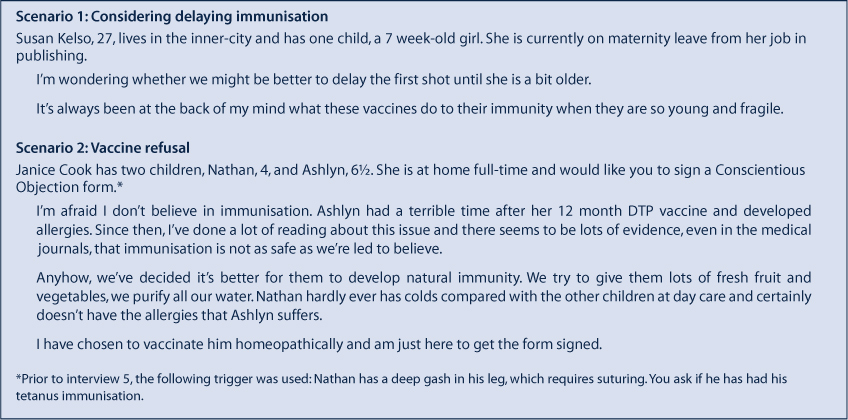
For the standardised scenarios in this study, characters and scripts were based on what is known of parents who refuse or vacillate about immunisation, and the arguments they employ.9,12–16 Proposed scenarios were discussed with a team of researchers, piloted with two GPs and modified accordingly (Box 1).
Participants
The study used a purposive sample drawn from typical case sampling and intensity sampling.17 Initially, GPs who were assumed to be typical cases were sought, using a database of respondents to a previous survey who had agreed to a further interview. GPs were chosen from a mix of inner-urban and suburban locations within the Sydney metropolitan area. Each GP was sent a letter that was followed by a telephone call. Due to a poor response using this method, the sample was supplemented with GPs known to have a particular interest in immunisation (intensity sampling). Some of these were ‘outliers’ – interesting and divergent cases who broaden the scope of the enquiry and provide richer insights than if the study were limited to only typical cases. Similar mixed recruitment strategies have been used elsewhere.18
Interviews
Interviews were conducted between November 2000 and February 2001. Participants who agreed to an interview were visited in their own practice. Two interstate GPs were interviewed over the telephone and another asked to email her responses. It was emphasised that the study aimed to describe how GPs communicate with parents about childhood immunisation.
In each interview, the researcher played the role of the parent, first giving the GP a brief character description and then initiating the script. GPs were asked to respond as they would in a normal encounter. The mock encounter was followed by questions aimed at debriefing; ascertaining whether the GP felt the scenarios were similar to situations experienced with parents; and discussing their actual experiences.
All interviews were recorded and transcribed by a professional transcription service. Each transcription was checked for inaccuracies.
Analysis
To evaluate GP communication, the analysis used previous research on what parents desire from such encounters; guidelines in the area of patient–doctor communication; the views of two mothers who read a representative cross-section of the transcripts; and the researcher’s own in-character reflections.15,19,20
Qualitative analysis is interpretive by nature.21 When the researcher is the instrument, he or she must be aware of how his or her beliefs and experiences shape the analysis. The qualitative literature labels this ‘reflexivity’.22 A journal was kept that included the author’s own experiences and reflections relevant to the study. This enabled the analysis to proceed with an awareness of how these might interact with the interpretation.
Transcripts were coded according to the dual perspective of describing typical rhetorical styles and evaluating interactions. Open coding was used where each interview transcript was read and re-read, and emerging patterns and themes noted freely.23 For each interview, memorandums were recorded that made brief observations about the wider meaning of the text and its connection to the emerging themes. Themes were reviewed, refined and grouped into a hierarchical coding system.24 All interviews were then coded according to this system. Passages preceding the coded text were re-read to ensure they were understood in context. Transcripts were also grouped by scenario in order to map typical discursive patterns peculiar to the scenarios. A sample of transcripts considered to most represent a cross-section of the themes was read by two women who had young children. The author met with each woman to discuss her impressions of the GPs’ responses. These were used to refine the emergent thematic framework.
Results
Twenty-eight GPs were approached via a letter and a follow-up telephone call. Of the 21 who returned calls, eight declined, with most citing lack of time and one because she was opposed to immunisation. Eleven interviews were completed.
Participants came from a range of areas, including three from semi-rural areas; three from mid-low income suburban areas; three from mid-high income suburban areas; and two from mid-high income inner-urban areas. Six of the GPs were women.
The analysis was grouped under three major categories: GPs’ persuasive strategies; content of what GPs said about risk; and the contexts in which discussions with parents occur. This paper focuses on the GPs’ persuasive strategies in responding to two of the four scenarios: one mother who was thinking about delaying scheduled vaccines until her baby was older and one who refused vaccines altogether. Each theme is identified in bold text.
Scenario 1: Considering delaying immunisation
Responses to Susan’s concerns could be broadly described as a ‘yes, but’ strategy. The ‘yes’ was where the GP acknowledged Susan’s concerns, sometimes with personalisation. The ‘but’ was usually expressed as straightforward negation or reframing. One GP even conceded his own concerns about immunisation:
I’m a parent myself … I know how awful it is to give these tiny little ones a vaccine, but it is safer for them to have it so that they have some protection at that young age from these quite serious diseases. (GP 2)
Many GPs probed for specifics, revealing that Susan held concerns about preservatives after reading about them on a website. One GP explained the strategic usefulness of this:
It’s only once you have agreed with them that … you become their ally before you can start changing them. (GP 11)
Following the acknowledgment and probing, the conjunction ‘but’ was often used to establish that Susan was wrong using subtle and unsubtle techniques. In relation to Susan’s baby’s immunity, one GP said:
… what we are actually doing is stimulating it by giving the shots. We’re not harming it. (GP 5)
GPs then directly addressed the preservatives issue, discrediting her source of information – the internet. Many compared disease risk with vaccine reaction risk. Some went on to define the possible vaccine side effects and how these might be minimised. Some reframed the vulnerability issue by focusing on the potentially damaging effects of a young child contracting a vaccine-preventable disease.
Scenario 2: Vaccine refusal
After the fifth GP interview, this scenario was introduced differently so that Janice approached the GP to have her Conscientious Objection form signed. Initial GPs had mentioned this as the most common context for encountering vaccine refusal. The Conscientious Objection form is a declaration signed by the parent and the provider, stating that a discussion about the risks and benefits of immunisation has taken place. It allows non-immunising parents in Australia to access government allowances.
Almost all GPs engaged in concerted attempts to convince Janice to vaccinate. Some offered written information and proposed to extend the consultation over a period of time. In the tetanus scenario, some offered immunoglobulin and penicillin as a compromise. In the form-signing scenario, two said they would not sign the form.
This scenario took the longest to act out and was confronting and uncomfortable to role play. It was often terminated by the interviewer before resolution because of time constraints. Debriefing was therefore important. Underlying the difficulties were diametrically opposed belief systems about health and disease prevention. One GP reflected on these conflicts:
I actually think most doctors have a lot of trouble with these sort of patients. They feel quite combatant towards them and quite stupidly evangelical in the same way that these people can be evangelical. (GP 10)
Most GPs began by attempting to convince Janice that her causal thinking had been wrong:
The fact that it occurred at that time in your child and the child subsequently developed various allergies I think is just a coincidence. It’s just a timing effect, not a cause … it was just something that occurred more or less at the same time. (GP 6)
Some conversations with Janice descended into games of scientific ‘ping pong’ where she would present her opinion, the GP would reply, and the conversation would get lost in a duel of competing claims.
GPs appealed to Janice’s sense of social obligation to other children who were at risk from her unvaccinated child. A repeated technique was the use of hypothetical scenarios to persuade Janice:
How would you feel if your child got something? Say your child got measles and another child caught it from your child and that child died? (GP 9)
GPs portrayed strong discomfort with Janice’s position. Although many would later acknowledge they stood little chance of changing her mind, many explained their persistence as concern for the child’s safety, particularly in the tetanus scenario:
You probably are not going to get her back. That child is at risk. But you can’t actually get a court order easily to make him have a tetanus vaccination. I mean, what do you do? (GP 4)
One GP used a counselling framework to explain his persistence:
If, in a counselling situation, someone makes an invalid statement, and then goes on with something and you don’t challenge it, they read that response as you agreeing with their position, or concurring with it. (GP 5)
This strategy was useful to the GP in terms of providing a reference point if Janice changed her mind. Using the transtheoretical model of behaviour change, the GP would establish the mother’s position on immunisation with respect to her readiness for change and move from there:25
If you want to get behavioural change out of people, you want to try three positions, like ‘don’t talk to me, I don’t want to know about it’, ‘give me the information, I’m shopping’, or ‘don’t bother me with details, just do it’. They’re the three basic levels of readiness for change. So she is number one, ‘don’t bother me with the information’. So you don’t bother them with the information. But you’ve still got to let them know that there’s information, that there is something out there, if they transition to stage 2. (GP 5)
Another GP, while engaged in concerted persuasive efforts, felt ultimately that keeping the ‘door open’ was in the interests of the child’s health should future medical care be needed (GP 9).
One GP’s strategy differed strikingly from most. He first established the firmness of Janice’s decision by asking, ‘Have you ever had any doubts about your decision?’. He then ascertained her knowledge about the consequences of her refusal and completed the discussion. In the debriefing he said:
This isn’t about being successful; this is a mother’s choice. I don’t consider it a failure if the person doesn’t choose to immunise their child. (GP 10)
Even though he shared with the other GPs a support for immunisation, his response to Janice was different in terms of brevity, content and implicit goals.
Discussion
This study examined the communication of 11 GPs who were likely to be confident communicators and interested in immunisation. The study identified many positive aspects of GP communication, some of which are reported in this paper. Almost all GPs acknowledged the mother’s concerns and sought to understand them further. Many also acknowledged the mother’s choice in relation to immunisation. They would often tailor their advice to the woman’s individual circumstances and the use of frameworks to guide communication appeared helpful. Perhaps less successful aspects of the encounters were when GPs entered into games of scientific ‘ping pong’; discredited a mother’s source of information; or asked hypothetical questions. While all these points are worthy of discussion, the latter two will be explored.
In the discussions following the role plays, GPs would explain their source discrediting strategy. For many, the internet and news media appeared to comprise an external battlefield. From it, parents brought various opinions, arguments and fashions in thinking. By implication, the GP’s surgery represented the centre of calm scientific rationality – the ‘war room’ where those who entered equipped themselves to counter-attack the outside influences. In the discrediting of sources was the implicit message, ‘Don’t trust what is out there, trust what is in here’. Indeed, many GPs referred to an existing level of trust with their patients. However, where trust is not yet built – either because of a patient’s transience or scepticism towards medicine – this strategy may not be helpful. Pointing women to more reliable websites provides an alternative viewpoint while not rejecting their preferred source of information.
Similarly, there are likely to be more successful strategies than the asking of hypothetical ‘how would you feel if’ questions, as seen in the vaccine refusal scenario. These force the respondent into a rhetorical corner where they must inhabit the GPs definition of how events would transpire. Such strategies are unlikely to be productive in risk discussions because they either alienate the respondent or manipulate them into action. A better way to convey the message might be in terms of it being a woman’s own choice, which also acknowledges vaccine risks but is more value neutral. The following example does not oblige the person to answer an emotive question:
You have to consider the illnesses you are preventing and how comfortable you feel about facing those without immunisation, versus the actual immunisation and the slight risks that are associated with that. That is the balancing act you need to decide … . (GP 10)
The doctors in this study appeared to readily take on the promotion of immunisation. This mainly generated discussion of the risks of non-immunisation, leaving less time to talk about the side effects from vaccines and their magnitude (a finding not detailed in this paper). This focus on persuasion is understandable: if a parent refuses immunisation, the costs are incurred by their child and society more broadly. In addition, GPs receive financial incentives to maintain high vaccination rates within their practices. However, doctors are also obliged to help parents reach an informed decision. Balancing these obligations is challenging.
Strong persuasion, rather than achieving its goal, may be counter-productive, further polarising a parent and, at worst, eroding trust.26,27 The fields of motivational interviewing and shared decision-making recommend a respectful interchange where health professionals help patients consider their options and the consequences of these.20,26 This less direct approach gives parents a supportive space to make their choice in which immunisation would often be chosen.28 Some, however, will stay committed in their resolve and providers must recognise their autonomy.29 The ethical merits of refusing to care for a family who will not vaccinate their child have been discussed.30 However, as some of the GPs in this study noted, maintaining a relationship with parents who delay or refuse immunisation leaves the door open should they change their mind.
In undertaking this study, I assumed that my findings were shaped by the research context and myself as interviewer. I had two roles in this study: that of actor and researcher. Rather than being a conflict, this approach added strength to the analysis, helping me to experience what a parent might feel in these interactions. Reflecting on my own experiences allowed me to explicitly identify how a background in nursing, my expectations and my preferences influenced my reading and evaluation of the interactions in this study. They particularly informed the categorisation of the themes into helpful and unhelpful communication, aided by the reflections of the two mothers and widely accepted principles of good communication.
Conclusions
The GPs in this study made concerted attempts to encourage immunisation while giving some information about its risks. Balancing the promotion of public health alongside supporting valid consent is possible but remains challenging. Communication frameworks such as shared decision-making may help doctors to negotiate these tensions.
Acknowledgments
This study was supported by a National Health and Medical Research Council project grant 1999–2000. The author is grateful to Simon Chapman, Penny Hawe and Margaret Burgess who were involved in planning the study, with advice from Phyllis Butow. Kirrily Leask and Louise O’Shea provided feedback on the interviews.
[1] Fagerlind H, Lindblad AK, Bergstrom I, Nilsson M, Naucler G, Glimelius B, et al. Patient-physician communication during oncology consultations. Psychooncology 2008; 17 975–85.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[2] Donovan JL, Blake DR. Qualitative study of interpretation of reassurance among patients attending rheumatology clinics: ‘just a touch of arthritis, doctor?’ BMJ 2000; 320 541–4.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[3] Colliver JA, Swartz MH, Robbs RS, Cohen DS. Relationship between clinical competence and interpersonal and communication skills in standardized-patient assessment. Acad Med 1999; 74 271–4.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[4] Epstein RM, Morse DS, Frankel RM, Frarey L, Anderson K, Beckman HB. Awkward moments in patient-physician communication about HIV risk. Ann Intern Med 1998; 128 435–42.
| CAS | PubMed |

[5] Ward J, Sanson-Fisher R. Does a 3-day workshop for family medicine trainees improve preventive care? A randomized control trial. Prev Med 1996; 25 741–7.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[6] Edwards A, Elwyn G, Gwyn R. General practice registrar responses to the use of different risk communication tools in simulated consultations: a focus group study. BMJ 1999; 319 749–52.
| CAS | PubMed |

[7] Leask J, Quinn HE, Macartney K, Trent M, Massey P, Carr C, et al. Immunisation attitudes, knowledge and practices of health professionals in regional NSW. Aust N Z J Public Health 2008; 32 224–9.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[8] Gellin BG, Maibach EW, Marcuse EK. Do parents understand immunizations? A national telephone survey. Pediatrics 2000; 106 1097–102.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[9]
[10] Sporton RK, Francis S-A. Choosing not to immunize: are parents making informed decisions? Fam Pract 2001; 18 181–8.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[11] Blair A, Davies E. Parental reasons for discontinuing the Australian vaccination schedule. Neonatal Paediatr Child Health Nurs 2003; 6 6–12.

[12]
[13] Pareek M, Pattison HM. The two-dose measles, mumps, and rubella (MMR) immunisation schedule: factors affecting maternal intention to vaccinate. Br J Gen Pract 2000; 50 969–71.
| CAS | PubMed |

[14] Bond L, Nolan T, Pattison P, Carlin J. Vaccine preventable diseases and immunisations: a qualitative study of mothers’ perceptions of severity, susceptibility, benefits and barriers. Aust N Z J Public Health 1998; 22 441–6.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[15] Leask J, Chapman S, Hawe P, Burgess M. What maintains parental support for vaccination when challenged by anti-vaccination messages? A qualitative study. Vaccine 2006; 24 7238–45.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[16] Leask JA, Chapman S. ‘An attempt to swindle nature’: press anti-immunisation reportage 1993–1997. Aust N Z J Public Health 1998; 22 17–26.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[17]
[18] Kitzinger J. Qualitative research. Introducing focus groups. BMJ 1995; 311 299–302.
| CAS | PubMed |

[19] Stoto MA, Evans G, Bostrom A. Vaccine risk communication. Am J Prev Med 1998; 14 237–9.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[20]
[21]
[22] Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ 2000; 320 50–2.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[23]
[24]
[25] Prochaska JO, Velicer WF. The transtheoretical model of behavior change. Am J Health Promot 1997; 12 38–48.
| CAS | PubMed |

[26]
[27] Meszaros JR, Asch DA, Baron J, Hershey JC, Kunreuther H, Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J Clin Epidemiol 1996; 49 697–703.
| Crossref | GoogleScholarGoogle Scholar | CAS | PubMed |

[28] Wallace C, Leask J, Trevena LJ. Effects of a web based decision aid on parental attitudes to MMR vaccination: a before and after study. BMJ 2006; 332 146–9.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[29] Asveld L. Mass-vaccination programmes and the value of respect for autonomy. Bioethics 2008; 22 245–57.
| Crossref | GoogleScholarGoogle Scholar | PubMed |

[30] Lyren A, Leonard E. Vaccine refusal: issues for the primary care physician. Clin Pediatr (Phila) 2006; 45 399–404.
| Crossref | GoogleScholarGoogle Scholar | PubMed |