Familiarity with, perceived accuracy of, and willingness to rely on Undetectable=Untransmittable (U=U) among gay and bisexual men in Australia: results of a national cross-sectional survey
James MacGibbon A * , Benjamin R. Bavinton
A * , Benjamin R. Bavinton  B , Timothy R. Broady
B , Timothy R. Broady  A , Jeanne Ellard C , Dean Murphy
A , Jeanne Ellard C , Dean Murphy  B D , Sarah K. Calabrese E , David A. Kalwicz F , Dash Heath-Paynter G , Angus Molyneux H , Cherie Power E , Andrew Heslop I , John de Wit A J and Martin Holt
B D , Sarah K. Calabrese E , David A. Kalwicz F , Dash Heath-Paynter G , Angus Molyneux H , Cherie Power E , Andrew Heslop I , John de Wit A J and Martin Holt  A
A
A Centre for Social Research in Health, UNSW Sydney, Sydney, NSW, Australia.
B Kirby Institute, UNSW Sydney, Sydney, NSW, Australia.
C Australian Research Centre in Sex, Health and Society, La Trobe University, Melbourne, Vic., Australia.
D Department of Infectious Diseases, Alfred Hospital and Central Clinical School, Monash University, Melbourne, Vic., Australia.
E New South Wales Ministry of Health, Sydney, NSW, Australia.
F Department of Psychological and Brain Sciences, George Washington University, Washington, DC, USA.
G Health Equity Matters, Sydney, NSW, Australia.
H ACON, Sydney, NSW, Australia.
I Positive Life NSW, Sydney, NSW, Australia.
J Department of Interdisciplinary Social Science, Utrecht University, Utrecht, Netherlands.
Sexual Health 20(3) 211-222 https://doi.org/10.1071/SH23050
Submitted: 6 March 2023 Accepted: 1 June 2023 Published: 28 June 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: The Undetectable=Untransmittable (U=U) message has been promoted since it was demonstrated that viral suppression through HIV treatment prevents sexual transmission between serodiscordant partners (HIV treatment as prevention). Our study assessed familiarity with, perceived accuracy of, and willingness to rely on U=U in a national sample of gay and bisexual men in Australia.
Methods: We conducted a national, online cross-sectional survey in April–June 2021. Eligible participants were gay, bisexual and queer men and non-binary people who lived in Australia. Logistic regression was used to identify factors associated with familiarity, perceived accuracy and willingness to rely on U=U (by having condomless sex with a partner with HIV who has an undetectable viral load).
Results: Of 1280 participants, most were familiar with U=U (1006/1280; 78.6%), the majority of whom believed U=U was accurate (677/1006; 67.3%). Both familiarity and perceived accuracy were higher among participants living with HIV, followed by pre-exposure prophylaxis (PrEP) users, HIV-negative participants not taking PrEP, and untested/unknown status participants. Knowing at least one person living with HIV, among other factors, was associated with familiarity and perceived accuracy of U=U; and familiarity was associated with perceived accuracy. Among participants familiar with U=U, less than half were willing to rely on U=U (473/1006; 47.0%). Familiarity with U=U and knowing at least one person living with HIV were associated with willingness to rely on U=U, among other factors.
Conclusions: We found familiarity with U=U was associated with perceived accuracy and willingness to rely upon it. There is an ongoing need to educate gay and bisexual men (particularly HIV-negative men) about U=U and its benefits.
Keywords: attitudes, Australia, biomedical HIV prevention, gay and bisexual men (GBM), HIV prevention, HIV undetectability, men who have sex with men (MSM), treatment as prevention (TasP).
Introduction
In 2016, the Prevention Access Campaign initiated the global Undetectable equals Untransmittable campaign (U=U; see preventionaccess.org) to increase awareness about the benefits of HIV treatment as prevention (TasP); that is, a person living with HIV who has achieved and maintained an undetectable viral load (UVL) through antiretroviral therapy (ART) cannot transmit HIV to their sexual partners.1–3 The U=U message has been widely embraced by the scientific community and global health organisations, including the World Health Organization.4 The Australian guidelines for healthcare providers who work with people living with HIV also strongly recommend that clinicians discuss U=U with their patients to reduce HIV-related stigma, encourage HIV treatment commencement and adherence, and support their psychosocial needs.5
Australian health organisations adopted TasP as part of a ‘combination HIV prevention’ approach and have promoted U=U in community messaging alongside the use of HIV pre-exposure prophylaxis (PrEP), condoms, and HIV testing.6 In addition to promoting the benefits of U=U for HIV prevention, the international U=U campaign has broader aims to reduce the stigma associated with HIV, improve quality of life for people living with HIV and their partners, and create a more supportive environment in which people more readily seek HIV testing and treatment.7 Illustrating some of these potential benefits for people living with HIV, an international study found that those who had discussed U=U with their healthcare providers were more likely to achieve viral suppression through ART, have better sexual health, and were more comfortable disclosing their HIV status.8
Prior to 2016 and the HIV Prevention Trials Network (HPTN) 052 randomised clinical trial results that informed the U=U campaign, TasP was generally understood to be a strategy for risk reduction rather than a strategy that eliminated risk.9 Research with communities affected by HIV (e.g. gay and bisexual men (GBM), heterosexual people in high prevalence countries) tended to assess knowledge of TasP as both an interpersonal strategy and a population level one – both the idea that viral suppression prevents transmission between sexual partners, and that achieving high levels of treatment and viral suppression in a population might slow or stop transmission.10,11 Research on how affected communities understood and engaged with TasP in the early 2010s generally found that there were both low levels of awareness of TasP, and high levels of scepticism that it worked.12–14 This research also tended to find that people living with HIV had higher levels of knowledge about and belief in TasP, compared with HIV-negative people. More recent reviews suggest that awareness and knowledge of TasP has grown over time in multiple countries and populations, but belief in its effectiveness remains lower than the level of awareness of the strategy.14 Our research with GBM, Australia’s main HIV-affected population, aligns with international research. We found that the proportion of GBM who believed that TasP was effective increased from 2.6% in 2013 to 38.1% in 2021, with participants with HIV consistently reporting higher levels of belief (9.1% in 2013 to 51.6% in 2021) compared to HIV-negative and untested/unknown status participants (2.0% in 2013 to 37.0% in 2021).15,16 However, these are relatively low levels of belief in TasP given the strong scientific evidence that viral suppression prevents transmission between serodiscordant couples,1–3 and the public discussion of these findings in Australia in social and community media, in community-directed education campaigns, and in public forums for GBM and other people affected by HIV, particularly since 2018.17
One issue that may contribute to low levels of belief in TasP is the conflation or overlap between the idea of TasP as an interpersonal strategy (preventing transmission between serodiscordant partners) and a population strategy (reducing transmission at a population level). Although there is strong scientific evidence that viral suppression prevents transmission between sexual partners (the key element of the U=U message), the effectiveness of TasP at a population level appears to be much less than was initially anticipated,9,18 with the population strategy undermined by delays in diagnosing people with HIV, and difficulties in people accessing and sustaining treatment.11 Even in countries with low levels of undiagnosed HIV, high levels of treatment coverage and viral suppression, TasP appears to have reduced but not stopped HIV transmission.19,20 This disconnect between the interpersonal and population-level strategies may affect how people respond to research about the acceptability or effectiveness of TasP. For instance, our previous research measured belief in the effectiveness of TasP with a three-item scale, with participants asked to rate their level of agreement with three items: ‘An HIV-positive person who is on HIV treatment is unlikely to transmit HIV’, ‘A person with an undetectable viral load cannot pass on HIV’, and ‘If every HIV-infected person was on treatment, the HIV epidemic would be over’.15,21,22 Although the first two items relate to the likelihood of interpersonal transmission, the third item references TasP as a population strategy, and has consistently had the lowest level of agreement among our participants, lowering the overall level of belief in TasP we recorded.16 This suggests that it may be worth assessing knowledge and belief in the interpersonal strategy of U=U separately from the population-level concept of TasP.
Since the Prevention Access Campaign coined the term U=U, research has begun to evaluate familiarity or perceived accuracy of the specific U=U message, rather than more general awareness or belief in TasP.14 A US study of GBM conducted in 2017–18 found that most of the sample knew what undetectable meant (92%), but only half (55%) perceived U=U as accurate.23 Perceived accuracy was highest among participants living with HIV (84%), followed by HIV-negative participants (54%), and untested/unknown status participants (39%). The proportion of those who agreed that U=U was accurate increased to 60% when those who did not know what undetectable meant were excluded; that is, to 84% of participants living with HIV, 58% of HIV-negative participants and 48% of untested/unknown status participants.23 Another US-based study conducted in 2018 found lower familiarity with, and perceived accuracy of U=U, with 85% of those surveyed aware of U=U, of whom 43% trusted that U=U was accurate.24 An international survey conducted in 2019 found that 88% of people living with HIV had heard of U=U,8 and a Canadian study conducted in 2018 found that 73% of participants were aware of U=U but did not ask about its perceived accuracy.25
Previous Australian research has not evaluated familiarity with the specific U=U message or its perceived accuracy. Previous research has assessed the willingness of Australian GBM to have condomless sex with a partner living with HIV who has an undetectable viral load, and found low levels of willingness,26–29 particularly among HIV-negative and untested men who do not use PrEP. However, most of this research was conducted before the U=U campaign gathered momentum and did not explicitly ask participants whether they were familiar with the U=U message, believed in its accuracy, or were willing to rely upon an undetectable viral load when having condomless sex with partners living with HIV. We therefore set out to address this gap by assessing demographic and behavioural characteristics associated with knowledge and belief in U=U in our latest survey of Australian GBM.
Methods
Study design and participants
The study design and methods have been described elsewhere.30–32 In brief, data were collected in a national, online, cross-sectional survey of GBM conducted in April–June 2021 using Qualtrics software (Provo, UT, USA). We promoted the survey through community organisations, Facebook groups about HIV prevention, and paid advertisements on Facebook and the dating/hook up app, Grindr. Potential participants were directed to the project website containing study information and a link to the survey. Participants provided consent before starting the survey. In 2021, eligible participants were aged ≥16 years, did not identify as female, did not identify as heterosexual, and lived in Australia; that is, male or non-binary and gay, bisexual or queer-identified people could participate. The study was approved by the ethics committee of UNSW Sydney (HC16954) and the community organisation ACON’s research review panel (2017/04; formerly the AIDS Council of New South Wales).
Measures
The questionnaire measures have been described previously.31,32 This analysis focuses on familiarity with, perceived accuracy of, and willingness to rely on U=U (the main outcome measures), some of which were new items in the 2021 survey. We also collected data on demographics, recent sexual practices, HIV status and testing, STI testing and recent diagnoses, use of HIV treatment and PrEP, and how many people living with HIV the participants knew.
We used a two-step approach to measure familiarity with and perceived accuracy of U=U, adapted from Rendina and Parsons.33 Familiarity was measured with the item, ‘How familiar are you with the Undetectable=Untransmittable (U=U) message?’. Response options were 1 = ‘Not at all’, 2 = ‘A little’, 3 = ‘Somewhat’, and 4 = ‘Very’. We coded responses 2–4 as being familiar with U=U. Participants who were familiar with U=U were asked how accurate they believed it to be: ‘How accurate do you believe the Undetectable=Untransmittable (U=U) message is?’. Response options were: 1 = ‘Completely inaccurate’, 2 = ‘Inaccurate’, 3 = ‘I don’t know’, 4 = ‘Accurate’, and 5 = ‘Completely accurate’. We coded responses 4–5 as believing that U=U was accurate.
Willingness to rely on U=U was operationalised as willingness to have condomless sex with a sexual partner who was living with HIV and had an undetectable viral load. All participants were presented with this item: ‘I would have sex without condoms with a HIV-positive person who is undetectable’. Responses were collected on a Likert-type scale ranging from 1 = ‘Strongly disagree’ to 5 = ‘Strongly agree’. We coded responses 4–5 as being willing to rely on U=U. We note that for participants using PrEP and most participants living with HIV, this item was not solely measuring willingness to rely on U=U (as they were protected by PrEP, or had an undetectable viral load themselves, respectively). The responses of HIV-negative and untested participants not using PrEP to this item is more indicative of willingness to rely solely on U=U.
Statistical analyses
Frequencies and proportions are reported for demographic and behavioural variables. Pearson’s chi-squared (X2) tests identified bivariable associations between the main outcome measures, HIV status and PrEP use. Multivariable logistic regression was used to identify independent associations of demographic and behavioural variables with the key outcomes (i.e. familiarity with, perceived accuracy of, and willingness to rely on U=U), with each outcome variable dichotomised; for example, familiar vs unfamiliar, perceived to be accurate vs inaccurate. Independent variables that were statistically significant at the bivariable level were block entered into the multivariable analyses. Statistical assumptions were assessed, including model diagnostics for logistic regression, none of which were violated. Variables in the regression models had no missing observations. We report unadjusted and adjusted odds ratios (OR and aOR) with 95% confidence intervals (CI). Statistical significance was set at P < 0.05 (two-tailed), which was also the cut-off point for the selection of independent variables in the multivariable analyses. Analyses were conducted using Stata ver. 16.1 (StataCorp, College Station, TX, USA).
Compliance with ethical standards
The questionnaire and methodology for this study were approved by the Human Research Ethics Committee of UNSW Sydney (HC16954) and endorsed by the community organisation, ACON (2017/04). Informed consent was obtained from all individual participants included in the study prior to their participation in the questionnaire.
Results
A total of 1280 participants completed the survey in 2021. The median age of the 1280 participants was 38 years (IQR = 30–52), 1038 (80.8%) identified as gay, 1261 (98.5%) were male, 916 (71.6%) were Australian born, 747 (58.4%) were university educated, 770 (60.2%) reported full-time employment, and 897 (70.1%) lived in the capital city of their state or territory. The greatest proportions of overseas-born participants originated from Europe (8.9% of the total sample), followed by South-East and East Asia (5.6%), and Oceania (excluding Australia; 4.1%). Most participants lived in one of Australia’s three most populous states: New South Wales (482; 37.7%), Victoria (318; 24.8%), or Queensland (209; 16.3%). In total, 1059 participants (82.7%) were HIV negative, 95 (7.4%) were HIV positive, and 126 (9.8%) were untested or did not know their status. Of the 1059 HIV-negative participants, 466 (44.0%) were taking PrEP at the time of the survey. Nearly all participants with HIV reported that they were on HIV treatment (94/95; 99.0%) and had an undetectable viral load (92/95; 96.8%).
Familiarity with U=U
Of the 1280 participants, 274 (21.4%) were ‘not at all’ familiar with U=U, 238 (18.6%) were ‘a little’ familiar, 305 (23.8%) were ‘somewhat’ familiar, and 463 (36.2%) were ‘very’ familiar with U=U; that is, 1006 (78.6%) participants had heard of U=U before the survey. Fig. 1 shows differences in familiarity with U=U (dichotomised as ‘not at all familiar’ vs everyone else) by HIV status and PrEP use, X2(3, 1280) = 139.06, P < 0.001. Participants living with HIV were most familiar with the U=U message (91/95; 95.8%), followed by PrEP users (421/472; 89.2%), HIV-negative participants not taking PrEP (441/593; 74.4%), and participants who were untested or did not know their HIV status (53/120; 44.2%).
Familiarity with, perceived accuracy of, and willingness to rely on Undetectable=Untransmittable (U=U) by HIV status and PrEP use. UVL, undetectable viral load.
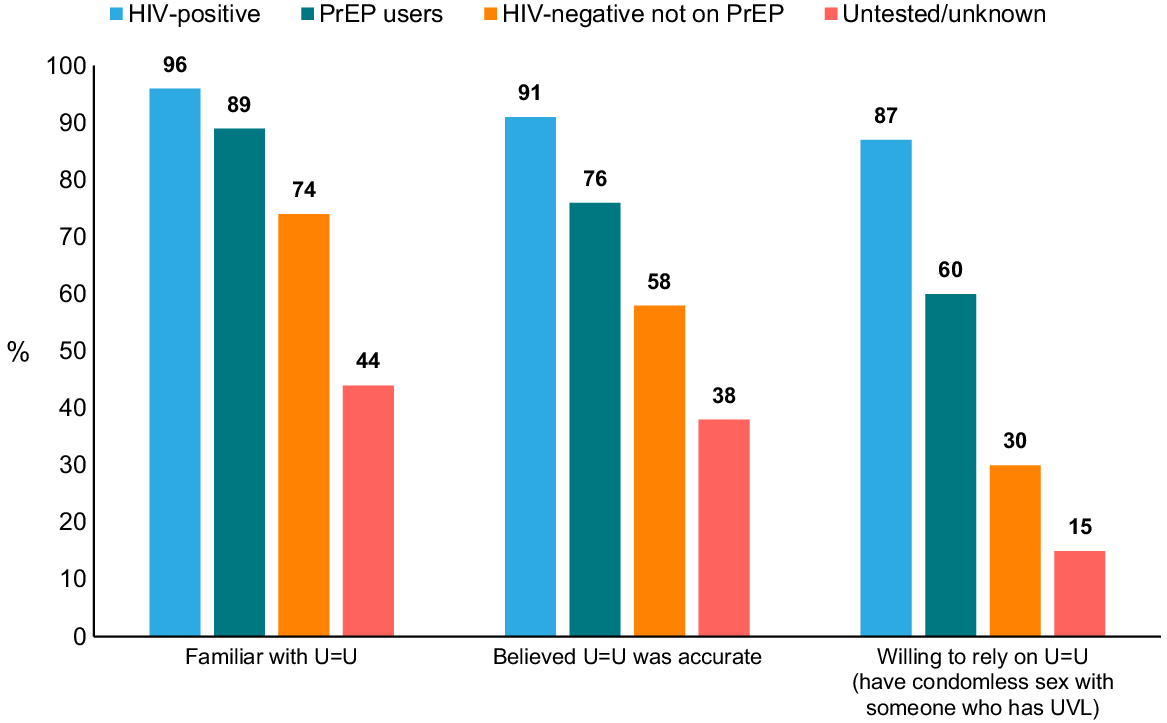
Table 1 shows factors associated with familiarity with U=U. Participants with HIV and PrEP users were more likely to be familiar with U=U compared to HIV-negative participants not taking PrEP, whereas untested and unknown HIV status participants were less likely to be familiar with U=U. Participants who knew at least one person living with HIV were also more likely to be familiar with U=U, compared to those who did not know anyone living with HIV. Participants who identified as bisexual compared to gay, and those living outside of capital cities, were less likely to be familiar with U=U.
| Total | No | Yes | OR (95% CI) | P-value | aOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|---|
| N = 1280 | n = 274 | n = 1006 | |||||
| Age (years) | |||||||
| <30 | 310 (24.2) | 94 (34.3) | 216 (21.5) | Ref | Ref | ||
| ≥30 | 970 (75.8) | 180 (65.7) | 790 (78.5) | 1.91 (1.43–2.56) | <0.001 | 0.82 (0.56–1.20) | 0.302 |
| Sexuality | |||||||
| Gay | 1034 (80.8) | 185 (67.5) | 849 (84.4) | Ref | Ref | ||
| Bisexual/pansexual | 193 (15.1) | 80 (29.2) | 113 (11.2) | 0.31 (0.22–0.43) | <0.001 | 0.56 (0.38–0.81) | 0.002 |
| Queer/another term | 53 (4.1) | 9 (3.3) | 44 (4.4) | 1.07 (0.51–2.22) | 0.866 | 1.42 (0.62–3.25) | 0.406 |
| State/territory | |||||||
| NSW | 482 (37.7) | 97 (35.4) | 385 (38.3) | Ref | Ref | ||
| Vic | 318 (24.8) | 57 (20.8) | 261 (25.9) | 1.15 (0.80–1.66) | 0.44 | 1.27 (0.85–1.90) | 0.247 |
| Qld | 209 (16.3) | 45 (16.4) | 164 (16.3) | 0.92 (0.62–1.37) | 0.674 | 1.19 (0.76–1.88) | 0.442 |
| Other states/territories | 271 (21.2) | 75 (27.4) | 196 (19.5) | 0.66 (0.47–0.93) | 0.018 | 0.80 (0.55–1.18) | 0.26 |
| Residential location | |||||||
| Capital city | 897 (70.1) | 158 (57.7) | 739 (73.5) | Ref | Ref | ||
| Other city/regional, rural or remote area | 383 (29.9) | 116 (42.3) | 267 (26.5) | 0.49 (0.37–0.65) | <0.001 | 0.69 (0.50–0.96) | 0.026 |
| Education level | |||||||
| High school/trade certificate | 533 (41.6) | 155 (56.6) | 378 (37.6) | Ref | Ref | ||
| University degree | 747 (58.4) | 119 (43.4) | 628 (62.4) | 2.16 (1.65–2.84) | <0.001 | 1.32 (0.96–1.82) | 0.082 |
| Employment status | |||||||
| Employed full time | 770 (60.2) | 143 (52.2) | 627 (62.3) | Ref | Ref | ||
| Employed part time | 196 (15.3) | 52 (19.0) | 144 (14.3) | 0.63 (0.44–0.91) | 0.014 | 0.88 (0.57–1.34) | 0.55 |
| Student/unemployed/other | 314 (24.5) | 79 (28.8) | 235 (23.4) | 0.68 (0.50–0.93) | 0.015 | 0.82 (0.57–1.17) | 0.272 |
| HIV status and PrEP use | |||||||
| Untested/unknown | 120 (9.4) | 67 (24.5) | 53 (5.3) | 0.27 (0.18–0.41) | <0.001 | 0.19 (0.04–0.84) | 0.028 |
| HIV negative not on PrEP | 593 (46.3) | 152 (55.5) | 441 (43.8) | Ref | Ref | ||
| HIV negative taking PrEP | 472 (36.9) | 51 (18.6) | 421 (41.8) | 2.85 (2.02–4.01) | <0.001 | 1.89 (1.24–2.89) | 0.003 |
| HIV positive | 95 (7.4) | 4 (1.5) | 91 (9.0) | 7.84 (2.83–21.70) | <0.001 | 5.05 (1.76–14.47) | 0.003 |
| Time since last HIV test | |||||||
| ≤12 months | 886 (69.2) | 142 (51.8) | 744 (74.0) | Ref | Ref | ||
| >12 months | 278 (21.7) | 70 (25.5) | 208 (20.7) | 0.57 (0.41–0.78) | 0.001 | 0.93 (0.53–1.65) | 0.811 |
| Never tested for HIV | 116 (9.1) | 62 (22.6) | 54 (5.4) | 0.17 (0.11–0.25) | <0.001 | 3.52 (0.73–16.88) | 0.116 |
| Time since last STI test | |||||||
| ≤12 months | 853 (66.6) | 129 (47.1) | 724 (72.0) | Ref | Ref | ||
| >12 months | 262 (20.5) | 66 (24.1) | 196 (19.5) | 0.53 (0.38–0.74) | <0.001 | 0.91 (0.51–1.61) | 0.744 |
| Never tested for STIs | 165 (12.9) | 79 (28.8) | 86 (8.5) | 0.19 (0.14–0.28) | <0.001 | 0.61 (0.34–1.10) | 0.099 |
| Number of male sex partners (last 6 months) | |||||||
| None | 175 (13.7) | 53 (19.3) | 122 (12.1) | Ref | Ref | ||
| 1–5 | 610 (47.7) | 151 (55.1) | 459 (45.6) | 1.32 (0.91–1.91) | 0.142 | 1.21 (0.76–1.94) | 0.423 |
| 6–10 | 209 (16.3) | 38 (13.9) | 171 (17.0) | 1.95 (1.21–3.15) | 0.006 | 1.09 (0.58–2.05) | 0.789 |
| >10 | 286 (22.3) | 32 (11.7) | 254 (25.2) | 3.45 (2.11–5.62) | <0.001 | 1.20 (0.61–2.37) | 0.591 |
| Sex with casual male partners (last 6 months) | |||||||
| Any condomless sex | 677 (52.9) | 107 (39.1) | 570 (56.7) | Ref | Ref | ||
| No casual partners/no anal sex | 455 (35.5) | 122 (44.5) | 333 (33.1) | 0.51 (0.38–0.69) | <0.001 | 1.01 (0.66–1.55) | 0.955 |
| Consistent condom use | 148 (11.6) | 45 (16.4) | 103 (10.2) | 0.43 (0.29–0.65) | <0.001 | 0.84 (0.53–1.34) | 0.468 |
| STI diagnosis in last 12 months | 284 (22.2) | 29 (10.6) | 255 (25.3) | 2.87 (1.90–4.32) | <0.001 | 1.39 (0.85–2.26) | 0.184 |
| Knows ≥1 person living with HIV | 737 (57.6) | 85 (31.0) | 652 (64.8) | 4.10 (3.07–5.46) | <0.001 | 2.48 (1.78–3.46) | <0.001 |
Note: data are n (%). Bolded values indicate statistical significance at P < 0.001 (two-tailed). Ref denotes the reference category for categorical variables, i.e., the baseline against which other levels of the variable were compared. Bivariable analyses showed that participants’ country of birth (i.e. Australia vs overseas) was not related to familiarity with U=U and this variable was excluded from further analyses.
Perceived accuracy of U=U
Of the 1006 participants who were familiar with the U=U message, 9 (0.9%) rated U=U as ‘completely inaccurate’, 39 (3.9%) rated it as ‘inaccurate’, 281 (27.9%) responded they ‘did not know’, 393 (39.1%) rated U=U as ‘accurate’, and 284 (28.2%) rated it as ‘completely accurate’; that is, 677 (67.3%) participants believed the U=U message was accurate or completely accurate. Fig. 1 shows differences in perceived accuracy of U=U (dichotomised as ‘accurate’ and ‘completely accurate’ vs all else) by HIV status and PrEP use, X2(3, 1006) = 74.80, P < 0.001. Most participants living with HIV rated the U=U message as accurate (83/91; 91.2%), followed by PrEP users (318/421; 75.5%), HIV-negative participants not taking PrEP (256/441; 58.0%), and participants who were untested or did not know their HIV status (20/53; 37.7%).
Table 2 shows factors associated with perceived accuracy of U=U. Participants who were more familiar with U=U had far greater odds of perceiving the U=U message as accurate, as did participants who knew at least one person living with HIV. By contrast, people who lived outside of Australia’s three most populous states (compared to participants in New South Wales), and separately, participants who reported consistent condom use compared to any condomless sex in the last 6 months, were less likely to perceive U=U as accurate.
| Total | No | Yes | OR (95% CI) | P-value | aOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|---|
| N = 1006 | n = 329 | n = 677 | |||||
| Age (years) | |||||||
| <30 | 216 (21.5) | 78 (23.7) | 138 (20.4) | Ref | |||
| ≥30 | 790 (78.5) | 251 (76.3) | 539 (79.6) | 1.21 (0.89–1.66) | 0.229 | ||
| Sexuality | |||||||
| Gay | 849 (84.4) | 261 (79.3) | 588 (86.9) | Ref | Ref | ||
| Bisexual | 113 (11.2) | 56 (17.0) | 57 (8.4) | 0.45 (0.30–0.67) | <0.001 | 0.73 (0.44–1.22) | 0.229 |
| Queer/another term | 44 (4.4) | 12 (3.6) | 32 (4.7) | 1.18 (0.60–2.33) | 0.627 | 0.81 (0.34–1.94) | 0.64 |
| State/territory | |||||||
| NSW | 385 (38.3) | 104 (31.6) | 281 (41.5) | Ref | |||
| Vic | 261 (25.9) | 93 (28.3) | 168 (24.8) | 0.67 (0.48–0.94) | 0.02 | 0.66 (0.42–1.02) | 0.063 |
| Qld | 164 (16.3) | 58 (17.6) | 106 (15.7) | 0.68 (0.46–1.00) | 0.05 | 0.78 (0.46–1.30) | 0.341 |
| Other states/territories | 196 (19.5) | 74 (22.5) | 122 (18.0) | 0.61 (0.42–0.88) | 0.008 | 0.59 (0.37–0.94) | 0.026 |
| Residential location | |||||||
| Capital city | 739 (73.5) | 224 (68.1) | 515 (76.1) | Ref | |||
| Other city/regional, rural or remote area | 267 (26.5) | 105 (31.9) | 162 (23.9) | 0.67 (0.50–0.90) | 0.007 | 0.96 (0.64–1.42) | 0.82 |
| Education level | |||||||
| High school/trade certificate | 378 (37.6) | 163 (49.5) | 215 (31.8) | Ref | |||
| University degree | 628 (62.4) | 166 (50.5) | 462 (68.2) | 2.11 (1.61–2.76) | <0.001 | 1.42 (1.00–2.03) | 0.053 |
| HIV status and PrEP use | |||||||
| Untested/unknown | 53 (5.3) | 33 (10.0) | 20 (3.0) | 0.44 (0.24–0.79) | 0.006 | 0.67 (0.09–5.25) | 0.703 |
| HIV negative not on PrEP | 441 (43.8) | 185 (56.2) | 256 (37.8) | Ref | |||
| HIV negative taking PrEP | 421 (41.8) | 103 (31.3) | 318 (47.0) | 2.23 (1.67–2.99) | <0.001 | 1.32 (0.86–2.02) | 0.208 |
| HIV positive | 91 (9.0) | 8 (2.4) | 83 (12.3) | 7.50 (3.54–15.87) | <0.001 | 2.41 (0.98–5.94) | 0.055 |
| Time since last HIV test | |||||||
| ≤12 months | 744 (74.0) | 220 (66.9) | 524 (77.4) | Ref | |||
| >12 months | 208 (20.7) | 77 (23.4) | 131 (19.4) | 0.71 (0.52–0.99) | 0.041 | 1.11 (0.53–2.30) | 0.788 |
| Never tested for HIV | 54 (5.4) | 32 (9.7) | 22 (3.2) | 0.29 (0.16–0.51) | <0.001 | 1.86 (0.22–15.82) | 0.57 |
| Time since last STI test | |||||||
| ≤12 months | 724 (72.0) | 206 (62.6) | 518 (76.5) | Ref | |||
| >12 months | 196 (19.5) | 75 (22.8) | 121 (17.9) | 0.64 (0.46–0.89) | 0.008 | 0.86 (0.42–1.76) | 0.677 |
| Never tested for STIs | 86 (8.5) | 48 (14.6) | 38 (5.6) | 0.31 (0.20–0.50) | <0.001 | 0.71 (0.32–1.56) | 0.397 |
| Number of male sex partners (last 6 months) | |||||||
| None | 122 (12.1) | 50 (15.2) | 72 (10.6) | Ref | |||
| 1–5 | 459 (45.6) | 174 (52.9) | 285 (42.1) | 1.14 (0.76–1.71) | 0.535 | 1.44 (0.79–2.63) | 0.24 |
| 6–10 | 171 (17.0) | 47 (14.3) | 124 (18.3) | 1.83 (1.12–3.00) | 0.016 | 1.66 (0.76–3.59) | 0.2 |
| >10 | 254 (25.2) | 58 (17.6) | 196 (29.0) | 2.35 (1.47–3.74) | <0.001 | 1.49 (0.69–3.22) | 0.312 |
| Sex with casual male partners (last 6 months) | |||||||
| Any condomless sex | 570 (56.7) | 158 (48.0) | 412 (60.9) | Ref | Ref | ||
| No casual partners/no anal sex | 333 (33.1) | 117 (35.6) | 216 (31.9) | 0.71 (0.53–0.95) | 0.020 | 1.18 (0.71–1.95) | 0.521 |
| Consistent condom use | 103 (10.2) | 54 (16.4) | 49 (7.2) | 0.35 (0.23–0.53) | <0.001 | 0.52 (0.30–0.92) | 0.023 |
| STI diagnosis in last 12 months | 255 (25.3) | 60 (18.2) | 195 (28.8) | 1.81 (1.31–2.51) | <0.001 | 1.13 (0.71–1.79) | 0.616 |
| Knows ≥1 person living with HIV | 677 (67.3) | 191 (51.1) | 496 (76.1) | 3.04 (2.31–4.00) | <0.001 | 1.49 (1.04–2.14) | 0.032 |
| Self-rated familiarity with U=U | |||||||
| A little familiar | 238 (23.7) | 185 (56.2) | 53 (7.8) | Ref | |||
| Somewhat familiar | 305 (30.3) | 107 (32.5) | 198 (29.2) | 6.46 (4.39–9.50) | <0.001 | 6.29 (4.19–9.46) | <0.001 |
| Very familiar | 463 (46.0) | 37 (11.2) | 426 (62.9) | 40.19 (25.52–63.28) | <0.001 | 29.19 (18.11–47.04) | <0.001 |
Note: data are n (%). Bolded values indicate statistical significance at P < 0.001 (two-tailed). Ref denotes the reference category for categorical variables, i.e., the baseline against which other levels of the variable were compared. Bivariable analyses showed that participants’ country of birth was not related to perceived accuracy of U=U and this variable was excluded from further analyses.
Willingness to rely on U=U
Of the 1006 participants who were familiar with the U=U message, 473 (47.0%) were willing to have condomless anal sex with a partner who had an undetectable viral load (i.e. to rely on U=U). Among those familiar with U=U, there were differences in willingness to have condomless sex with a partner who was undetectable, by HIV status and PrEP use, X2(3, 1006) = 158.59, P < 0.001. Fig. 1 shows that greater proportions of participants living with HIV were willing to have condomless sex with a partner who was undetectable (80/91; 87.9%), followed by PrEP users (251/421; 59.6%), HIV-negative participants not taking PrEP (134/441; 30.4%), and participants who were untested or did not know their HIV status (8/53; 15.1%); that is, the proportion of HIV-negative and untested participants not on PrEP who were familiar with U=U and willing to rely on it during sex was 15.1–30.4%. When we restricted the sample to those who were both familiar with U=U and believed that the U=U message was accurate, the proportions in each subgroup who were willing to have condomless sex with a partner who was undetectable increased. However, the differences in willingness by HIV status and PrEP use remained similar. Among those who were familiar with U=U and who believed U=U was accurate (n = 677), greater proportions of participants living with HIV were willing to have condomless sex with a partner with HIV who was undetectable (75/83; 90.4%), followed by PrEP users (230/318; 72.3%), HIV-negative participants not taking PrEP (112/256; 43.8%), and participants who were untested or did not know their HIV status (5/20; 25.0%; X2(3, 677) = 90.82, P < 0.001). Among the same group of participants who were familiar with U=U and believed U=U was accurate (n = 677), willingness to have condomless sex with a partner who was undetectable was higher among participants who believed U=U was completely accurate (239/284; 84.2%), compared with participants who believed U=U was only ‘accurate’ (183/393; 46.6%; X2(1, 677) = 99.22, P < 0.001).
Table 3 shows factors associated with willingness to have condomless sex with a partner with HIV who was undetectable among the 1006 participants who were familiar with U=U. Participants who were more familiar with U=U had far greater odds of being willing to have condomless sex with a partner who was undetectable, as were participants who knew at least one person living with HIV and university-educated participants. By contrast, the following groups were less willing to have condomless sex with a partner who was undetectable: people who lived outside of Australia’s three most populous states (compared to participants in New South Wales), people aged >30 years, and people who reported consistent condom use.
| Total | No | Yes | OR (95% CI) | P-value | aOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|---|
| N = 1006 | n = 533 | n = 476 | |||||
| Age (years) | |||||||
| <30 | 216 (21.5) | 142 (26.6) | 74 (15.6) | Ref | Ref | ||
| ≥30 | 790 (78.5) | 391 (73.4) | 399 (84.4) | 1.96 (1.43–2.68) | <0.001 | 0.49 (0.31–0.79) | 0.003 |
| Sexuality | |||||||
| Gay | 849 (84.4) | 429 (80.5) | 420 (88.8) | Ref | Ref | ||
| Bisexual | 113 (11.2) | 81 (15.2) | 32 (6.8) | 0.40 (0.26–0.62) | <0.001 | 0.76 (0.45–1.28) | 0.3 |
| Queer/another term | 44 (4.4) | 23 (4.3) | 21 (4.4) | 0.93 (0.51–1.71) | 0.822 | 0.75 (0.31–1.79) | 0.518 |
| State/territory | |||||||
| NSW | 385 (38.3) | 185 (34.7) | 200 (42.3) | Ref | Ref | ||
| Vic | 261 (25.9) | 147 (27.6) | 114 (24.1) | 0.72 (0.52–0.98) | 0.039 | 0.65 (0.42–1.02) | 0.06 |
| Qld | 164 (16.3) | 84 (15.8) | 80 (16.9) | 0.88 (0.61–1.27) | 0.497 | 0.76 (0.46–1.25) | 0.277 |
| Other states/territories | 196 (19.5) | 117 (22.0) | 79 (16.7) | 0.62 (0.44–0.88) | 0.008 | 0.59 (0.37–0.95) | 0.031 |
| Education level | |||||||
| High school/trade certificate | 378 (37.6) | 223 (41.8) | 155 (32.8) | Ref | Ref | ||
| University degree | 628 (62.4) | 310 (58.2) | 318 (67.2) | 1.48 (1.14–1.91) | 0.003 | 1.48 (1.04–2.11) | 0.031 |
| HIV status and PrEP use | |||||||
| Untested/unknown | 53 (5.3) | 45 (8.4) | 8 (1.7) | 0.41 (0.19–0.89) | 0.024 | 0.57 (0.07–4.73) | 0.606 |
| HIV negative not on PrEP | 441 (43.8) | 307 (57.6) | 134 (28.3) | Ref | Ref | ||
| HIV negative taking PrEP | 421 (41.8) | 170 (31.9) | 251 (53.1) | 3.38 (2.55–4.48) | <0.001 | 1.19 (0.56–2.50) | 0.65 |
| HIV positive | 91 (9.0) | 11 (2.1) | 80 (16.9) | 16.66 (8.59–32.31) | <0.001 | 1.63 (0.19–14.20) | 0.659 |
| Time since last HIV test | |||||||
| ≤12 months | 744 (74.0) | 363 (68.1) | 381 (80.5) | Ref | Ref | ||
| >12 months | 208 (20.7) | 126 (23.6) | 82 (17.3) | 0.62 (0.45–0.85) | 0.003 | 1.19 (0.56–2.50) | 0.65 |
| Never tested for HIV | 54 (5.4) | 44 (8.3) | 10 (2.1) | 0.22 (0.11–0.44) | <0.001 | 1.63 (0.19–14.20) | 0.659 |
| Time since last STI test | |||||||
| ≤12 months | 724 (72.0) | 342 (64.2) | 382 (80.8) | Ref | Ref | ||
| >12 months | 196 (19.5) | 125 (23.5) | 71 (15.0) | 0.51 (0.37–0.70) | <0.001 | 0.83 (0.40–1.72) | 0.618 |
| Never tested for STIs | 86 (8.5) | 66 (12.4) | 20 (4.2) | 0.27 (0.16–0.46) | <0.001 | 0.66 (0.30–1.46) | 0.306 |
| Number of male sex partners (last 6 months) | |||||||
| None | 122 (12.1) | 78 (14.6) | 44 (9.3) | Ref | Ref | ||
| 1–5 | 459 (45.6) | 292 (54.8) | 167 (35.3) | 1.01 (0.67–1.54) | 0.948 | 1.33 (0.73–2.45) | 0.355 |
| 6–10 | 171 (17.0) | 83 (15.6) | 88 (18.6) | 1.88 (1.17–3.03) | 0.009 | 1.55 (0.71–3.37) | 0.272 |
| >10 | 254 (25.2) | 80 (15.0) | 174 (36.8) | 3.86 (2.45–6.07) | <0.001 | 1.43 (0.66–3.10) | 0.367 |
| Sex with casual male partners (last 6 months) | |||||||
| Any condomless sex | 570 (56.7) | 238 (44.7) | 332 (70.2) | Ref | Ref | ||
| No casual partners/no anal sex | 333 (33.1) | 210 (39.4) | 123 (26.0) | 0.42 (0.32–0.55) | <0.001 | 1.12 (0.67–1.86) | 0.670 |
| Consistent condom use | 103 (10.2) | 85 (15.9) | 18 (3.8) | 0.15 (0.09–0.26) | <0.001 | 0.49 (0.27–0.86) | 0.014 |
| STI diagnosis in last 12 months | 255 (25.3) | 97 (18.2) | 158 (33.4) | 2.25 (1.68–3.02) | <0.001 | 1.08 (0.68–1.73) | 0.732 |
| Knows ≥1 person living with HIV | 652 (64.8) | 259 (48.6) | 393 (83.1) | 5.20 (3.87–6.98) | <0.001 | 1.74 (1.19–2.54) | 0.004 |
| Self-rated familiarity with U=U | |||||||
| A little familiar | 238 (23.7) | 193 (36.2) | 45 (9.5) | Ref | Ref | ||
| Somewhat familiar | 305 (30.3) | 192 (36.0) | 113 (23.9) | 2.52 (1.69–3.76) | <0.001 | 6.44 (4.27–9.72) | <0.001 |
| Very familiar | 463 (46.0) | 148 (27.8) | 315 (66.6) | 9.13 (6.25–13.33) | <0.001 | 29.94 (18.52–48.40) | <0.001 |
Note: data are n (%). Bolded values indicate statistical significance at P < 0.001 (two-tailed). Ref denotes the reference category for categorical variables, i.e., the baseline against which other levels of the variable were compared. Bivariable analyses showed that participants’ country of birth was not related to willingness to rely on U=U and this variable was excluded from further analyses.
Discussion
This was the first study to assess familiarity with, perceived accuracy of, and willingness to rely on the specific U=U message in a national sample of GBM in Australia. We found that most participants were familiar with U=U, but fewer believed it was accurate and were willing to rely upon it. Familiarity with U=U in the sample was concentrated among participants with HIV and PrEP users, and participants who knew at least one person living with HIV. Consistent with previous studies, our findings reaffirm that there is greater awareness of the U=U message in the social networks of GBM who are more engaged with HIV prevention and sexual health services, such as people living with HIV and PrEP users.23,24
Over three-quarters of GBM in our study had heard of (were familiar with) the U=U message, two-thirds of those who were familiar with U=U believed it was accurate, and nearly half those who believed U=U was accurate were willing to rely upon it. Our measure of familiarity differed from other studies. For example, in a US study conducted in 2017–18, participants either rated how accurate U=U was or instead selected if they were unsure what undetectable meant; this measure therefore inferred that 92% of the sample knew what undetectable meant, but did not ask specifically about knowledge of U=U.23 Another US study conducted in 2018 found that 85% of participants were aware of the specific U=U message.24 The level of perceived accuracy of U=U in our sample (67%) was higher compared to the aforementioned US studies, at 60% of participants in the first study who knew what undetectable meant23 and 43% of the participants in the second study who were aware of U=U.24 The greater perceived accuracy of U=U observed in our study was likely due to it being conducted a number of years later. Similarly, the level of familiarity with and perceived accuracy of U=U among people living with HIV in our study (96% and 91% respectively) was higher than that found in Australian and international research conducted in 2017–19.8,28,34 These results suggest that awareness of and belief in U=U continue to grow over time,14 and that most GBM living with HIV in Australia now believe that U=U is accurate, which is likely to be beneficial in supporting their health and sense of wellbeing.14 Willingness to have condomless sex with a person with HIV who had an undetectable viral load was our measure of willingness to rely on U=U, which we stratified by HIV status and PrEP use. Our results showed the highest level of confidence in relying on U=U recorded to date among GBM in Australia.26,27,29
Consistent with previous research, we found that knowledge of and belief in U=U was concentrated among people living with HIV, followed by PrEP users.15,23 The lowest levels of familiarity, perceived accuracy and willingness to rely upon U=U were among HIV-negative and untested men who were not using PrEP (some of the groups who might benefit from greater knowledge of U=U). As familiarity was independently associated with both belief in U=U’s accuracy, and willingness to rely upon it, this suggests that education efforts should continue to focus (as a first step) on raising awareness of U=U among HIV-negative and untested men (particularly among those who do not use PrEP). However, we acknowledge that asking someone who does not know their HIV status to learn about U=U may be missing some important intermediate steps, such as confirming basic knowledge about HIV prevention and transmission, explaining why testing is useful, and the efficacy of contemporary HIV treatments in maintaining health and wellbeing. Previous Australian research suggests that, compared with previously tested GBM, those who have never tested for HIV are more likely to be younger, identify as bisexual, be more afraid of testing positive, not know where to test, and live outside inner city areas,35–38 which overlaps with some of our findings about who was less likely to know about, believe in or rely on U=U. Improving basic knowledge of HIV, how to access supportive services and encouraging testing may be important factors for encouraging discussions about U=U among untested GBM. This is most likely to be achieved through community-level health promotion and education campaigns. International research suggests that HIV-negative people may be concerned about relying on U=U because it involves them trusting that a partner living with HIV is adherent to treatment and has accurate knowledge of their viral load;14,39 for that reason, researchers have suggested it may be easier to rely on U=U in relationships where trust has already been established rather than broaching a potentially difficult conversation about U=U with casual sex partners.39,40
We acknowledge the limitations of our analyses. We recruited a convenience sample that may not be representative of GBM nationally,41 and may have had an overrepresentation of PrEP users. This means the levels of familiarity, perceived accuracy and willingness to rely on U=U we measured could have been overestimated in the whole sample (although we stratified by HIV status and PrEP use to compensate for this). We asked participants to self-rate their familiarity with U=U, but did not seek to assess their knowledge of U=U against any objective criteria. Participants also self-rated the accuracy of U=U based on their own understanding of it, which may or may not have been correct. For example, consistent with early health messaging, they may have understood U=U to mean ‘effectively no risk’ or ‘minimal risk,’ and rated U=U as completely accurate believing it to reflect something other than 0% risk. It would be beneficial to explore relative levels of perceived risk among participants in future studies. Next, measuring willingness to have condomless sex with a person with an undetectable viral load is a crude way to assess willingness to rely upon U=U that does not consider other contextual factors, levels of trust, or how intimate relationships affect condom use.32 For PrEP users in particular, the measure of willingness to have condomless sex with an undetectable partner does not really assess reliance on U=U (as they may be relying on PrEP as much as or more than U=U). Willingness to rely on U=U among HIV-negative and untested GBM not using PrEP is probably the truer measure of willingness to rely solely on U=U in this sample. In addition, there is likely to be a gap between hypothetical willingness to rely on U=U and what GBM do in practice, and it would be beneficial to assess how many GBM report condomless sex with partners living with HIV and how this relates to beliefs about U=U. Future research could also explore the extent to which some HIV-negative GBM prefer to rely on an individual prevention strategy under their own control, such as PrEP or condom use, and how such a preference might influence reliance on U=U for HIV prevention. Finally, our analysis is useful for assessing community knowledge of U=U and identifying some groups who may benefit from greater education about the strategy. However, we did not assess what would make it easier for GBM to learn about or believe in U=U. We also did not explore specific fears and concerns about the strategy, such as potential uncertainty about partners sustaining an undetectable viral load and psychosocial barriers to relying on U=U, which qualitative studies have raised.39,42 This could be investigated in future research.
Conclusion
International research suggests that encouraging greater awareness of U=U appears to lead to higher levels of belief in the strategy.14 This may be useful for combination prevention efforts, highlighting that there are a range of effective ways to prevent HIV. Knowledge of U=U may be particularly critical for people living with HIV and their partners, reassuring them that serodiscordant sex can be safe.43 Our results suggest that GBM living with HIV in Australia are now largely convinced of U=U’s efficacy, which is a welcome development. Knowledge of U=U appears to have grown among other GBM, but there is an ongoing need to continue to familiarise people with U=U and convince them of its safety.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons. Syntax for the database coding and analysis may be available upon reasonable request to the corresponding author.
Conflicts of interest
The authors declare no conflicts of interest. Authors BB and MH are Editors of Sexual Health, but were blinded from the peer review process for this paper.
Declaration of funding
The PrEPARE Project is supported by the Bloodborne Viruses and Sexually Transmissible Infection Research, Intervention and Strategic Evaluation Program of the New South Wales Ministry of Health, and surveillance funding from the Australian Government Department of Health. The Centre for Social Research in Health and the Kirby Institute receive funding from the Australian Government Department of Health. The funding agencies did not have any involvement in the collection, analysis and interpretation of data, or in the writing of this manuscript and decision to submit for publication. No pharmaceutical funding was received for this study.
Author contributions
JM, BRB, TRD, JE, DM, HP, AM, CP, JdW and MH contributed to the study design. JM and MH oversaw data collection. JM conducted the quantitative analyses. JM and MH drafted the manuscript. All authors contributed to the interpretation of findings, reviewed drafts of the manuscript and agreed with the final version.
References
1 Bavinton BR, Pinto AN, Phanuphak N, Grinsztejn B, Prestage GP, Zablotska-Manos IB, et al. Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. Lancet HIV 2018; 5(8): e438-e47.
| Crossref | Google Scholar |
2 Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet 2019; 393(10189): 2428-38.
| Crossref | Google Scholar |
3 Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365(6): 493-505.
| Crossref | Google Scholar |
7 Ford OG, Rufurwadzo TG, Richman B, Green I, Alesi J. Adopting U = U to end stigma and discrimination. J Int AIDS Soc 2022; 25(3): e25891.
| Crossref | Google Scholar |
8 Okoli C, Van de Velde N, Richman B, Allan B, Castellanos E, Young B, et al. Undetectable equals untransmittable (U = U): awareness and associations with health outcomes among people living with HIV in 25 countries. Sex Transm Infect 2021; 97(1): 18-26.
| Crossref | Google Scholar |
9 Bavinton BR, Rodger AJ. Undetectable viral load and HIV transmission dynamics on an individual and population level: where next in the global HIV response? Curr Opin Infect Dis 2020; 33(1): 20-7.
| Crossref | Google Scholar |
10 Montaner JSG. Treatment as prevention – a double hat-trick. Lancet 2011; 378(9787): 208-9.
| Crossref | Google Scholar |
11 Baral S, Rao A, Sullivan P, Phaswana-Mafuya N, Diouf D, Millett G, et al. The disconnect between individual-level and population-level HIV prevention benefits of antiretroviral treatment. Lancet HIV 2019; 6(9): e632-e8.
| Crossref | Google Scholar |
12 Young I, McDaid L. How acceptable are antiretrovirals for the prevention of sexually transmitted HIV?: a review of research on the acceptability of oral pre-exposure prophylaxis and treatment as prevention. AIDS Behav 2014; 18(2): 195-216.
| Crossref | Google Scholar |
13 Holt M. HIV pre-exposure prophylaxis and treatment as prevention: a review of awareness and acceptability among men who have sex with men in the Asia-Pacific region and the Americas. Sex Health 2014; 11(2): 166-70.
| Crossref | Google Scholar |
14 Bor J, Fischer C, Modi M, Richman B, Kinker C, King R, et al. Changing knowledge and attitudes towards HIV treatment-as-prevention and “Undetectable = Untransmittable”: a systematic review. AIDS Behav 2021; 25(12): 4209-24.
| Crossref | Google Scholar |
15 Holt M, MacGibbon J, Bear B, Lea T, Kolstee J, Crawford D, et al. Trends in belief that HIV treatment prevents transmission among gay and bisexual men in Australia: results of national online surveys 2013–2019. AIDS Educ Prev 2021; 33(1): 62-72.
| Crossref | Google Scholar |
16 MacGibbon J, Bavinton B, Broady TR, Kolstee J, Power C, Molyneux A, et al. Trends in attitudes to biomedical HIV prevention among gay and bisexual men: key findings from the PrEPARE Project 2021. Sydney: Centre for Social Research in Health, UNSW Sydney; 2022. Available at http://doi.org/10.26190/jpap-4w04
18 Montaner JSG, Hogg R, Wood E, Kerr T, Tyndall M, Levy AR, et al. The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet 2006; 368(9534): 531-6.
| Crossref | Google Scholar |
19 Wilson DP. HIV treatment as prevention: natural experiments highlight limits of antiretroviral treatment as HIV prevention. PLoS Med 2012; 9(7): e1001231.
| Crossref | Google Scholar |
20 Callander D, McManus H, Gray RT, Grulich AE, Carr A, Hoy J, et al. HIV treatment-as-prevention and its effect on incidence of HIV among cisgender gay, bisexual, and other men who have sex with men in Australia: a 10-year longitudinal cohort study. Lancet HIV 2023; 10: E385-E93.
| Crossref | Google Scholar |
21 Holt M, Lea T, Murphy DA, Ellard J, Rosengarten M, Kippax SC, et al. Australian gay and bisexual men’s attitudes to HIV treatment as prevention in repeated, national surveys, 2011–2013. PLoS ONE 2014; 9(11): e112349.
| Crossref | Google Scholar |
22 Holt M, Lea T, Schmidt H-M, Murphy D, Rosengarten M, Crawford D, et al. Increasing belief in the effectiveness of HIV treatment as prevention: results of repeated, national surveys of Australian gay and bisexual men, 2013–15. AIDS Behav 2016; 20(7): 1564-71.
| Crossref | Google Scholar |
23 Rendina HJ, Cienfuegos-Szalay J, Talan A, Jones SS, Jimenez RH. Growing acceptability of Undetectable = Untransmittable but widespread misunderstanding of transmission risk: findings from a very large sample of sexual minority men in the United States. J Acquir Immune Defic Syndr 2020; 83(3): 215-22.
| Crossref | Google Scholar |
24 Carneiro PB, Westmoreland DA, Patel VV, Grov C. Awareness and acceptability of Undetectable = Untransmittable among a U.S. national sample of HIV-negative sexual and gender minorities. AIDS Behav 2021; 25(2): 634-44.
| Crossref | Google Scholar |
25 Card KG, St. Denis F, Higgins R, Klassen B, Ablona A, Rutherford L, et al. Who knows about U = U? Social positionality and knowledge about the (un)transmissibility of HIV from people with undetectable viral loads. AIDS Care 2022; 34(6): 753-61.
| Crossref | Google Scholar |
26 Bavinton BR, Holt M, Grulich AE, Brown G, Zablotska IB, Prestage GP. Willingness to act upon beliefs about ‘treatment as prevention’ among Australian gay and bisexual men. PLoS ONE 2016; 11(1): e0145847.
| Crossref | Google Scholar |
27 Holt M, Draper BL, Pedrana AE, Wilkinson AL, Stoové M. Comfort relying on HIV pre-exposure prophylaxis and treatment as prevention for condomless sex: results of an online survey of Australian gay and bisexual men. AIDS Behav 2018; 22: 3617-26.
| Crossref | Google Scholar |
28 Huntingdon B, de Wit J, Duracinsky M, Juraskova I. Belief, covariates, and impact of the “Undetectable = Untransmittable” message among people living with HIV in Australia. AIDS Patient Care STDS 2020; 34(5): 205-12.
| Crossref | Google Scholar |
29 Dowell-Day A, Dobbins T, Chan C, Fraser D, Holt M, Vaccher SJ, et al. Attitudes towards treatment as prevention among PrEP-experienced gay and bisexual men in Australia. AIDS Behav 2023;
| Google Scholar |
30 MacGibbon J, Lea T, Ellard J, Murphy D, Kolstee J, Power C, et al. Access to subsidized health care affects HIV pre-exposure prophylaxis (PrEP) uptake among gay and bisexual men in Australia: results of national surveys 2013–2019. J Acquir Immune Defic Syndr 2021; 86(4): 430-5.
| Crossref | Google Scholar |
31 Holt M, MacGibbon J, Bavinton B, Broady T, Clackett S, Ellard J, et al. COVID-19 vaccination uptake and hesitancy in a national sample of Australian gay and bisexual men. AIDS Behav 2022; 26(8): 2531-8.
| Crossref | Google Scholar |
32 MacGibbon J, Bavinton B, Drysdale K, Murphy D, Broady T, Kolstee J, et al. Explicit relationship agreements and HIV pre-exposure prophylaxis use by gay and bisexual men in relationships. Arch Sex Behav 2023; 52: 761-71.
| Crossref | Google Scholar |
33 Rendina HJ, Parsons JT. Factors associated with perceived accuracy of the Undetectable = Untransmittable slogan among men who have sex with men: implications for messaging scale-up and implementation. J Int AIDS Soc 2018; 21(1): e25055.
| Crossref | Google Scholar |
34 Cingolani A, Tavelli A, Calvino GV, Maggiolo F, Girardi E, Cozzi-Lepri A, et al. Awareness and perception of accuracy of the Undetectable=Untransmittable message (U=U) in Italy: results from a survey among PLWHA, infectious-diseases physicians and people having unprotected sex. AIDS Care 2023; 923-33.
| Crossref | Google Scholar |
35 Conway DP, Holt M, Couldwell DL, Smith DE, Davies SC, McNulty A, et al. Barriers to HIV testing and characteristics associated with never testing among gay and bisexual men attending sexual health clinics in Sydney. J Int AIDS Soc 2015; 18(1): 20221.
| Crossref | Google Scholar |
36 Lyons A, Pitts M, Grierson J, Smith A, McNally S, Couch M. Sexual behavior and HIV testing among bisexual men: a nationwide comparison of Australian bisexual-identifying and gay-identifying men. AIDS Behav 2012; 16(7): 1934-43.
| Crossref | Google Scholar |
37 Zablotska I, Holt M, de Wit J, McKechnie M, Mao L, Prestage G. Gay men who are not getting tested for HIV. AIDS Behav 2012; 16(7): 1887-94.
| Crossref | Google Scholar |
38 Chan C, Broady TR, Bavinton BR, Mao L, Prestage GP, Holt M. Assessing the HIV prevention needs of young gay and bisexual men in the PrEP era: an analysis of trends in Australian behavioural surveillance, 2014–2018. AIDS Behav 2020; 24(8): 2382-6.
| Crossref | Google Scholar |
39 Borsa A, Siegel K. Barriers to treatment as prevention adoption among sexual and gender minority individuals who have sex with men in the United States. AIDS Patient Care STDS 2023; 37(5): 268-77.
| Crossref | Google Scholar |
40 Philpot SP, Prestage G, Ellard J, Grulich AE, Bavinton BR, For the Opposites Attract study group. How do gay serodiscordant couples in Sydney, Australia negotiate undetectable viral load for HIV prevention? AIDS Behav 2018; 22(12): 3981-90.
| Crossref | Google Scholar |
41 Grulich AE, de Visser RO, Badcock PB, Smith AMA, Heywood W, Richters J, et al. Homosexual experience and recent homosexual encounters: the second Australian study of health and relationships. Sex Health 2014; 11(5): 439-50.
| Crossref | Google Scholar |
42 Grace D, Nath R, Parry R, Connell J, Wong J, Grennan T. ‘… if U equals U what does the second U mean?’: sexual minority men’s accounts of HIV undetectability and untransmittable scepticism. Cult Health Sex 2021; 23(9): 1270-86.
| Crossref | Google Scholar |
43 Persson A. ‘The world has changed’: pharmaceutical citizenship and the reimagining of serodiscordant sexuality among couples with mixed HIV status in Australia. Sociol Health Illn 2016; 38(3): 380-95.
| Crossref | Google Scholar |


