Improving digital partner notification for sexually transmitted infections and HIV through a systematic review and application of the Behaviour Change Wheel approach
Will Kocur A , Julie McLeod
A , Julie McLeod  A , Sonja Charlotte Margot Bloch
A , Sonja Charlotte Margot Bloch  B , Jennifer J. MacDonald
B , Jennifer J. MacDonald  A , Charlotte Woodward B , Amelia McInnes-Dean B , Jo J. Gibbs
A , Charlotte Woodward B , Amelia McInnes-Dean B , Jo J. Gibbs  B , John J. Saunders
B , John J. Saunders  B C , Ann A. Blandford
B C , Ann A. Blandford  D , Claudia Estcourt
D , Claudia Estcourt  A and Paul Flowers
A and Paul Flowers  E *
E *
A
B
C
D
E
Abstract
Partner notification (PN) is key to controlling sexually transmitted infections (STIs) and human immunodeficiency virus (HIV). Digital PN options (e.g. social media, short message service (SMS), emails) are promising in increasing PN behaviour. However, their implementation is often challenging and studies report varied levels of acceptability and uptake of PN, highlighting the need to optimise digital PN interventions.
A systematic review of barriers and facilitators to digital PN interventions for STIs, including HIV, across eight research databases (from 2010 to 2023) identified eight relevant studies, two of which addressed HIV. Data extraction identified 98 barriers and 54 facilitators to the use of digital PN interventions. These were synthesised into 18 key barriers and 17 key facilitators that were each deemed amenable to change. We then used the Behaviour Change Wheel approach, the Acceptability, Practicability, Effectiveness, Affordability, Side-effects and Equity criteria, and multidisciplinary expert input, to systematically develop practical recommendations to optimise digital PN.
Thirty-two specific recommendations clustered around three themes. Digital PN interventions should: (1) empower and support the index patient by providing a range of notification options, accompanied by clear instructions; (2) integrate into users’ existing habits and the digital landscape, meeting contemporary standards and expectations of usability; and (3) address the social context of PN both online and offline through normalising the act of PN, combating STI-related stigma and stressing the altruistic aspects of PN through consistent messaging to service users and the public.
Our evidence-based recommendations should be used to optimise existing digital PN interventions and inform the co-production of new ones.
Keywords: behaviour, Behaviour Change Wheel, community interventions, contact tracing, health promotion, health services, interventions, LGBT, men who have sex with men, partner notification, psychology, public health, STIs.
Introduction
Partner notification (PN), also known as contact tracing, is the process by which the sexual contacts of a patient with a sexually transmitted infection (STI) or human immunodeficiency virus (HIV) are informed that they may be at risk of infection and are offered screening and treatment if indicated.1 PN is a key tool in STI/HIV control, as positivity rates among notified partners are often high (30–40%2,3). However, rates of engaging in PN are often low (8–11%2,3), risking re-infection and onward transmission to others.4,5 Digital PN interventions offer great potential for improving PN outcomes.6–8 Digital PN interventions are diverse, typically harnessing social media, short message service (SMS), email, or dedicated mobile phone or web applications (apps) to facilitate the process of notification (C. Woodard et al., unpubl. data).6 Some digital PN interventions additionally support online access to testing for sex partners and/or treatment (partner management).9,10
Digital PN interventions offer several benefits including convenience, reduced time between receiving a result and notifying partners,2 anonymous online notification without the need of a third party,4 and ease of notifying large numbers of sex partners11 potentially at lower cost than more traditional methods such as a healthcare professional phoning sexual partners. Digital PN interventions might also reduce the risk of intimate partner violence,12 may increase rates of notification,13 and may be particularly appropriate for ‘one-off’ sex partners.4 However, there is significant variation in both acceptability and use of digital PN interventions4,6 with between 5% and 92% of people in various studies indicating intention to use digital PN interventions, but between 4% and 27% of people in different studies actually using them.4,14
Given the benefits of digital PN interventions, there is disparity and variation in acceptability of and uptake of them. It is critical to understand the barriers and facilitators to using digital PN interventions and how to optimise digital PN to increase PN behaviour. Therefore, this study aimed to: (1) identify and analyse the barriers and facilitators to using digital PN interventions reported in recent literature; and (2) systematically develop evidence-based and theoretically informed recommendations for optimising digital PN interventions.
Materials and methods
Study design: we took a multi-levelled approach to systematically develop recommendations to optimise digital PN interventions using behaviour change theory and multidisciplinary expertise to inform key recommendations.
Objectives
To identify barriers and facilitators to using digital PN interventions in the published literature; to use a behavioural science approach to develop evidence based and theoretically informed recommendations.
Protocol registration
A study protocol with detailed methodology was pre-registered on PROSPERO.15 For justisfication of one deviation from this protocol, see Supplementary file S1 in Supplementary material.
Search strategy
A systematic search of articles published between January 2010 and July 2023 across eight research databases (CINAHL Plus, Cochrane Library, Embase, Medline, NHS Evidence, PsycINFO, Scopus, and Web of Science) was conducted (by SB), targeting the combination of three topics: (1) digital health; (2) STIs/HIV; and (3) PN/contact tracing. For exact terms, see Table S1 in Supplementary file.
Selection process
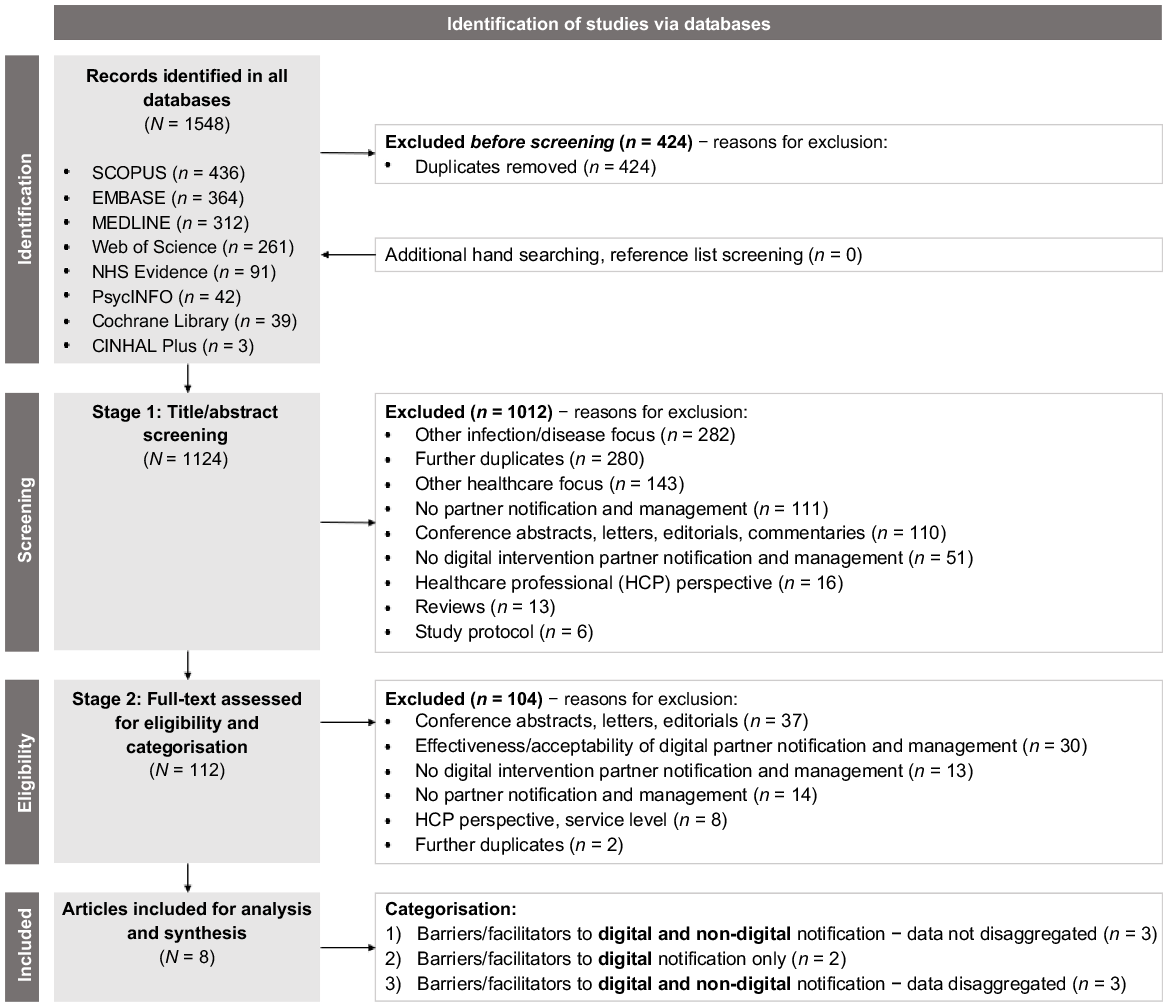
The results of the search were exported to EndNote ver. X9, and duplicates were removed. First, the titles, keywords and abstracts were screened and checked against the eligibility criteria in Table 1 (by SB and JS). Second, full texts were assessed against the criteria in Table 1 (see Fig. 1 for additional details). Uncertainty about studies meeting the inclusion criteria was discussed with JM and PF until a consensus was reached. The final included studies were categorised into: (1) barriers and facilitators for online notification of partners; and (2) barriers and facilitators for online management of partners (such as their testing and treatment following index patient testing positive).
Inclusion criteria | Exclusion criteria | |
|---|---|---|
|
Digital methods were defined as those conducted via the internet (emails, websites, online sexual health clinics), text/SMS messages, and smartphone applications (apps). Telephone (voice calls) were not considered a digital method. PN was defined as an index patient informing sex partner(s) of exposure to an STI or HIV. Partner management was defined as an index patient linking sex partner(s) to testing and/or treatment.
Quality of contributing studies
The Mixed Methods Appraisal Tool ver. 2018 (MMAT)16 was used (by CW, JG, SB, PF) to assess the quality and appropriateness of the study methods.
Data extraction
The following data was extracted by SB in a data extraction table in Excel: data on country; scenario (hypothetical or implemented intervention); study objectives; the type of STI/HIV; main method of data collection; and details of the digital aspects of the intervention were extracted by SB into a table in Excel.
Individual barriers and facilitators were copied verbatim into an Excel spreadsheet by JM. Barriers and facilitators were identified from reported positives and negatives about a digital PN intervention; reasons for, or for not, notifying partners; reasons for choosing a PN method; and any PN preferences or concerns. Where papers reported barriers and facilitators to PN but it was not possible to distinguish digital and non-digital (e.g. face-to-face) methods, these findings were included. Where papers reported barriers and facilitators to using both digital and non-digital methods of PN, any exclusively non-digital barriers and facilitators were excluded.
Data analysis
Research Question 1: to generate evidence concerning the main barriers and facilitators to using digital PN interventions, verbatim barriers and facilitators were synthesised based on their similarity (by JM and SB). For example, ‘Did not have contact details’, ‘Tried to contact partner with no success’, ‘Not having email addresses for partners’ were synthesised into ‘Problems contacting partners’. Synthesised barriers and facilitators were then de-duplicated and recorded in a separate spreadsheet. This was reviewed by PF and disagreements were resolved by discussion until consensus was reached.
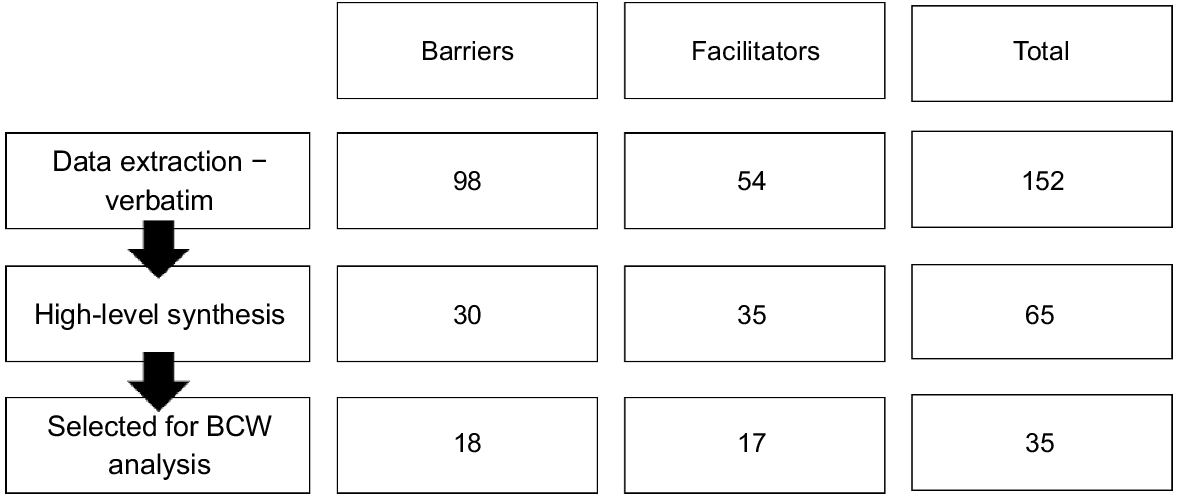
Extracting only data relating to digital PN, we identified 98 barriers and 54 facilitators. Many more individual barriers to PN were extracted than facilitators, as one paper reported only barriers.17 The individual barriers and facilitators were then synthesised to generate 30 high-level barriers and 35 high-level facilitators, of which 18 and 17, respectively, were selected (using selection criteria, see Supplementary file S2 in Supplementary file) to be taken forward to Behaviour Change Wheel (BCW) analysis to develop recommendations for future digital PN interventions. See Fig. 2 for an overview.
Research Question 2: the BCW approach,18 which incorporates the theoretical domains framework (TDF),19 was then used to generate theoretically informed recommendations on how to improve the use of digital PN interventions. The BCW approach is a way of systematically developing theoretically informed intervention content from a detailed understanding of the behavioural drivers of a particular behaviour18); in this case, using a digital PN intervention. Here, the de-duplicated, synthesised barriers and facilitators were critically appraised (by WK, JM and PF) for selection for BCW analysis using selection criteria (see Supplementary file S2 in Supplementary file).
Selected synthesised barriers and facilitators were coded (by JM and SB) with appropriate TDF19 domains. This coding was reviewed by WK. Disagreements were resolved by discussion until consensus was reached. The TDF brings together a plethora of behaviour change theories to classify drivers of behaviour into 14 domains (e.g. ‘Beliefs about capability’, ‘Knowledge’, or ‘Social influences’). It enables the theorisation of the drivers of behaviour in a pragmatic and useful way that allows subsequent work to systematically generate recommendations for future intervention content.
To generate recommendations, WK matched the theorised barriers and facilitators to intervention functions, using the BCW,18 and Behaviour Change Techniques (BCTs), using the Behaviour Change Technique Taxonomy ver. 1 (BCTT ver. 1; a set of 93 unique active ingredients of behaviour change interventions20). BCTs were then operationalised (by WK) considering Acceptability, Practicability, Effectiveness, Affordability, Side-effects and Equity (APEASE criteria).18 These operationalised recommendations were then reviewed by JM. Disagreements were resolved by discussion until consensus was reached.
Finally, considering the APEASE criteria once more18 recommendations were further assessed and reviewed by a wider multidisciplinary team (JS, CE, JG) including sexual health clinicians, a medical sociologist and a principal health advisor (sexual healthcare professional responsible for PN within a large geographical area).
All BCW coders completed the UCL Centre for Behaviour Change BCTT Online Training (http://www.bct-taxonomy.com/). All stages of analysis were additionally reviewed by PF, a senior behavioural scientist with considerable expertise in using these tools across a range of diverse topics.
Results
Study selection
The search identified 1548 studies, 1124 remained after de-duplication. After screening titles and abstracts, 112 studies were assessed for full-text eligibility, following which eight studies remained. For an overview of the study selection process, see the PRISMA flow diagram in Fig. 1.
Study characteristics
A summary of the article characteristics is in Table 2. Populations addressed included HIV pre-exposure prophylaxis (PrEP) users,21 cisgender men and transwomen,22 men who have sex with men (MSM),17,23,24 people recently diagnosed with chlamydia9,25 and the general population.26 The eight articles used a range of qualitative and quantitative approaches. Five studies related to hypothetical digital PN interventions;17,21–23,26 only one reported solely on an intervention that had been delivered25 and two concerned both real and hypothetical interventions.9,24
Author (year), Country | Participants | Scenario | Study objectives | Type of STI | Study methods of data collection | Details of the PN intervention(s) addressed | |
|---|---|---|---|---|---|---|---|
Bilardi et al. (2010),9 Australia | 202 men and women recently diagnosed with chlamydia | Real/hypothetical | To describe the PN experiences of individuals diagnosed with chlamydia and to determine what supports might best assist them | Chlamydia | Telephone survey | ||
Carnicer-Pont et al. (2015),26 Spain | 1578 Spanish residents | Hypothetical | To explore the intention to use new communication technologies for PN in Spain | All STIs in general | Two cross-sectional surveys | ||
Contesse et al. (2019),23 United States of America | 28 cisgender men who have sex with men (MSM) using GSN (geosocial networking) apps to meet partners | Hypothetical | To examine how MSM across the United States of America use geosocial networking apps and their perspectives regarding delivery of HIV/STD PN | All STIs in general | Online focus group | ||
Hopkins et al. (2010),25 Australia | 40 people with recent chlamydia diagnosis | Real | Use and acceptability of different PN methods (face-toface, phone, email, SMS, letter) to help inform strategy development to increase number of partners notified | Chlamydia | Semi-structured telephone interviews | ||
Kutner et al. (2021),22 United States of America | 59 cisgender men and transgender women | Hypothetical | To explore the interest in disclosing test results through a smartphone app dedicated to self and partner testing for HIV/syphilis | Syphilis and HIV | In-person survey and interview | ||
Lessard et al. (2019),21 France | 21 PrEP users, 10 community mediators, 5 × 1–1 interviews with prescribers, 4 × HIV/STI management decision-makers | Hypothetical | To describe stakeholders’ perspectives on the acceptability of a digital smartphone STI PN tool (WeFLASH©) | All STIs in general | 2-h focus groups; 1–1 interviews | ||
Wang et al. (2016),17 People’s Republic of China | 372 MSM | Hypothetical | To examine willingness and preferences for PN among MSM to measure feasibility and optimise uptake | Syphilis | Factorial survey; socio-demographic questionnaire | ||
Yan et al. (2022),24 People’s Republic of China | 53 people including 32 MSM and six men living with HIV and 11 healthcare professionals | Real/hypothetical | To identify the challenges of current HIV partner services and provide insight on possible interventions that can enhance partner services for MSM in China | HIV | Qualitative analysis of crowdsourced data |
PN, partner notification; MSM, men who have sex with men; STI, sexually transmitted infection; PrEP, HIV pre-exposure prophylactic; SMS, short messaging service; STD, sexually transmitted disease.
Quality appraisal
Most articles satisfied all, or the majority, of MMAT criteria, as detailed in Table S2 in Supplementary file. As such, none were excluded from further analysis. All eight studies focused on PN (chlamydia, n = 2; HIV, n = 1, syphilis, n = 1; HIV and syphilis, n = 1; and STIs in general, n = 3) and none focused on partner management. Understanding the barriers and facilitators to using digital PN interventions was complicated because PN was addressed in different ways in different studies. In three studies, it was not possible to distinguish whether barriers and facilitators to PN related specifically to digital or non-digital modalities.9,17,26 In three other studies, it was possible to distinguish barriers and facilitators related specifically to digital or non-digital modalities.23–25 Finally, two studies reported only barriers and facilitators to digital PN interventions21,22 (Table 2).
Table 3 presents the final list of selected synthesised barriers and facilitators in order of decreasing frequency, including barriers and facilitators which solely related to digital aspects of PN. Synthesised barriers were wide ranging. Some concerned the nature and affective context of sexual relationships (e.g. the index patient believes that digital modes of PN are inappropriate for established relationships), whereas others were concerned with the technological aspects of digital PN interventions (e.g. concerns about the privacy of STI status). Further barriers were not exclusive to digital PN (e.g. concerns about their partners’ reactions). Synthesised facilitators were equally diverse, for example, including beliefs about the positive consequences of digital PN (e.g. protection from embarrassment) and beliefs about the technology underpinning digital PN interventions (e.g. digital PN interventions makes it practically easier to contact partners).
Numbers in brackets refer to the frequency of individual verbatim barrier and facilitator statements. Those unique to digital are in bold and italicised. Barriers and facilitators not appearing in bold were indistinguishable between digital or non-digital PN in the original studies.
Using the BCW, we systematically developed a list of specific recommendations to enhance the content of future digital PN interventions and optimise their use (see Supplementary Table S3). These stem directly from the barriers and facilitators identified above (Table 3). These recommendations provide theoretically-based ‘work-arounds’ to the reported barriers, and enhance the reported facilitators we synthesised from the original published studies. To aid usability of the 32 detailed recommendations, we synthesised them into three themes (and associated key recommendations) (Table 4) described in the text that follows. As there were no studies identified relating to partner management, no recommendations could be developed for this.
| Main themes | Key recommendations | |
|---|---|---|
| 1. Digital PN interventions should be empowering and support the index patient Digital PN systems should enable notification choices tailored to the individual and their circumstances and provide information in varying formats to be consumed at a pace and time suited to the index patient. | 1.1. Provide the information needed to choose the most appropriate notification method (digital and non-digital) for each sexual partner Digital PN interventions should clearly present options for PN, both digital and face-to-face/phone, to allow index patients to find the method that best suits them and their partner(s). They should be encouraged to consider emotional, privacy or practical factors, including the speed of PN. A comparison table or interactive decision tool that guides the index patient to find their preferred method could be offered [8]. Digitally mediated descriptions, examples and/or demonstrations of how each digital notification method would appear from the sex partner’s perspective could enable the index patient to consider the appropriateness of different methods for each of their partners [7]. | |
| 1.2. Provide clear instructions, guides and demonstrations of how to notify partners using each available method. Any intervention content that enables PN should be simple and contain clear instructions. The addition of Gif/video demonstrations could take advantage of the digital medium [6]. Information and guidance on face-to-face PN, such as through pre-recorded demonstrations should also be provided [10]. Such PN demonstrations, can be complemented by short, pre-set and persuasive messages about PN containing links to health information and services, it should be possible to copy and share these easily with partners [25]. | ||
| 1.3. Provide and/or clearly signpost practical and emotional support. Digital PN interventions need to provide access to emotional and practical support to reduce emotional barriers to PN, such as anxiety [9, 13]. Additionally, digital PN interventions should provide health information [14] and practical support in using the given intervention for those that may struggle, for example, due to low digital literacy [29]. | ||
| 1.4. Reinforce the simplicity of the core PN process. Any intervention content that enables PN should be simple and contain only essential information and messaging. Further information should be provided in dedicated and signposted sections or when the need is indicated, for instance, after clicking on ‘How does PN work?’ or in a FAQs section [24]. | ||
| 2. Digital PN interventions should be convenient and integrate with other systems Effective PN systems should integrate well with and make use of the existing digital landscape and technologies. | 2.1. Use familiar digital norms and make the most of digital efficiency and convenience. The experience of using a digital PN intervention should feel simple, convenient and familiar. User interfaces should conform to standard expectations for digital tools to help reduce the digital literacy requirements [28]. Digital PN interventions should allow rapid PN, including for multiple sex partners [22], whilst allowing customisation and notification choices to be made separately for different partners [21]. Sensitive and discreet prompts, compliant with data protection regulations, could be useful to prompt and encourage an index patient to notify partners; these should be used sparingly and occur within a limited timeframe [25]. Reassure sex partners that the notification is legitimate/authentic by providing directions to care which do not require clicking on a link, such as providing potentially useful search terms [2]. | |
| 2.2. Explore integration with geosocial networking apps (dating/hook-up apps) or methods for anonymously linking sex partners. Digital PN interventions could be integrated into dating/hook-up apps providing the option for automated notification without external contact details. This may also enable access to health information or support from a healthcare professional through the app [23]. The authenticity of healthcare services within the app should be asserted, for example, by using branding or a domain name associated with a trusted institution [1]. Apps could further facilitate later notification by anonymously linking the accounts/devices of people who have sex without any contact method or exchange of details. WeFLASH© is an example of such technology and could be particularly useful for people with multiple low-commitment sex partners or who engage in anonymous or group sex. | ||
| 3. Digital PN interventions should normalise PN as an act of caring and as socially responsible Strong and consistent messaging about the normative and altruistic aspects of PN should be core parts of digital PN interventions. | 3.1. Normalise notification and combat stigma. Digital PN interventions should expose users to positive messages, figures and peer-led personal stories about PN. These can create a sense of community, reducing stigma and normalising PN, which cannot be done as easily in an in-person setting. The system should highlight that many people test positive for an STI and PN is a routine part of STI health care. For example, ‘Every year around half a million people in the UK test positive for an STI and partner notification is a normal part of the treatment process’ [16]. Positive videos or written stories showing contributions from people who have notified partners or been partner-notified about an STI can help create a sense of peer approval and normality [31] and similar videos could extend to peers modelling the notification process itself in a positive light [18]. These should represent the diversity of the intervention’s potential users and, if possible, be tailored and relevant to the index patient. Digital PN interventions could signpost existing, credible resources that provide peer support to those who have received a diagnosis or been notified by partners of risk [12]. Finally, FAQs submitted to the site by real people can be displayed. | |
| 3.2. Frame partner notification as an act of caring. Digital PN interventions should present PN as an act of caring. This can be done by using language to this effect (e.g. ‘Help your partner get tested’ as opposed to ‘Complete partner notification details’) [26] and by explaining that notifying a partner early can help protect them from longer-term health consequences [19]. Digital PN interventions should avoid potentially stigmatising language, including that which can be read as signifying blame, or that suggests the direction of infection transmission [27]. Videos and stories of people who have engaged in PN [12, 18, 31] should also be used within a website or app as an opportunity to depict PN as an act of caring for the health of partners as well as for the health and wellbeing of the index patient’s wider communities [32]. |
The numbers in square brackets represent the unique recommendation ID. This can be used to find the original recommendation from analyses found in (Table S4).
To improve digital PN interventions, we should enable index patient choice by providing a range of PN options, and instructions on how to use each of them, using varying communication formats. Digital PN interventions should be designed so they can be used at a place, pace and time suited to diverse index patients without the involvement of third parties. There should be clear demonstrations of how to do PN using a range of examples (e.g. short videos showing what to say, or the provision of simple adaptable scripts) with simple guidance on how to access practical and emotional support if and when it is needed (e.g. listing available helplines or websites). The simplicity of the core PN process should be emphasised throughout and also depicted visually (e.g. simple graphics and links to frequently asked questions (FAQs) that can provide further levels of detail if they are needed).
Digital PN interventions should be integrated within the existing digital landscape, technologies, and users’ expectations and habits (e.g. dating/hook-up apps). This will ensure they feel familiar and convenient for most people and are available in digital locations already regularly used. Familiar digital norms, culture and ‘industry standards’ should be replicated within digital PN interventions (e.g. high quality of interface and graphics). The functionality of digital PN interventions should enable the user to tailor PN processes to different types of sexual partner (e.g. ‘casual’ and ‘established’ partners27) quickly and easily. Digital PN systems should include the proportionate use of discreet prompts for the index patient to notify their partners should they not do so, as well as providing directions to further sexual health care that do not require clicking on a link (e.g. suggested search terms).
The social context of PN must be addressed. Intervention content needs to normalise the act of PN, combat STI and HIV-related stigma, and emphasise the altruistic aspects of PN. Strong and consistent messaging about the positive value of PN for communities, couples and individuals is needed and should be reinforced both within PN systems and in wider communications. Written text as well as images, videos, figures and animations should be used to convey the positive social value of PN (explaining that it is the ‘right thing to do’). Throughout, it is important to consider ways of reframing PN as an act of caring and emphasising its positive role in minimising the risk of potential negative health consequences via the onward transmission of STIs and HIV for all.
Discussion
To our knowledge, this is the first study to synthesise the published literature regarding barriers and facilitators to using digital PN interventions and use them to systematically develop a set of recommendations for improving digital PN interventions. The development of the recommendations draws on evidence (i.e. the key barriers and facilitators identified from the literature), theory (i.e. the TDF and the BCW), and expert input (multidisciplinary staff that used the APEASE criteria). The findings of the study, if operationalised effectively with relevant stakeholders (such as industry partners, community-based organisations (CBO)s, service users and service providers), have great potential to improve the quality and uptake of digital PN interventions.
Main findings
Few studies have focused on digital PN interventions and there are considerable gaps in the literature around partner management, HIV, and non-hypothetical studies within digital PN. Of the eight studies identified as relevant, all focused solely on notification and not on partner management (i.e. testing and treatment), and are consistent with the narrative review by Golden et. al.6 on partner services for HIV/STIs in high-income nations. Here, most studies investigated bacterial STIs, with only two examining HIV; and there was a large proportion of hypothetical preference studies. There was also a high degree of heterogeneity in relation to study participants and STIs addressed. Further, the reporting of specific barriers and facilitators to using digital PN interventions was poor, with many studies amalgamating barriers and facilitators across both digital and non-digital modalities (e.g. face-to-face, phone calls, SMS, email).
There were multiple, diverse, re-occurring barriers and facilitators to using digital PN interventions with considerably more barriers than facilitators reported in the literature. Key barriers and facilitators to using digital PN interventions included factors associated with index patients’ levels of knowledge of PN itself or of STIs and HIV, or beliefs about the health risks associated with STIs/HIV and the imagined consequences of PN; and factors associated with the technological aspects of digital PN interventions such as concerns about safeguards and imagined links into future face-to-face sexual health care. These barriers may help to explain why acceptability of, intention to use, and uptake of digital PN interventions is often low and highly varied.4,6,14 Many of these important barriers and facilitators were amenable to change and were reflected in the wide-ranging, multi-levelled recommendations our behavioural analysis generated.
Our evidence and theory-based recommendations include that digital PN interventions should enable and empower index patients to make choices about the kinds of PN that work for them and their partner(s). This means ensuring that digital PN interventions educate and model how to notify partners and also enable access to psychosocial support when doing so if it is needed. Digital PN interventions need to be as simple, convenient and usable as possible, complying with explicit and implicit ‘industry’ standards (e.g. the quality of visual content) and where possible, integrating into other existing digital systems (e.g. dating apps). Our recommendations also emphasise that unless the social and cultural context of PN is addressed, future digital PN interventions are unlikely to gain traction or be effective in the long term. Reinforcing messages about the positive aspects of PN (for individuals, partners and communities) and our collective responsibility to enact it will be crucial going forwards. If these upstream psychosocial and sociocultural issues are not addressed, downstream technological innovation has little chance of increasing the use of digital PN interventions and improving PN outcomes. These recommendations are designed to directly overcome the barriers and enhance facilitators to engaging with digital PN interventions identified in the literature, to improve the uptake of digital PN interventions.
Implications for practice
Using these recommendations could considerably enhance digital PN interventions. However, the multi-levelled nature of the recommendations means that delivering them will necessarily involve working in partnership with a variety of stakeholders with diverse skill sets and expertise. The recommendations are relatively systemic, speaking simultaneously to both the upstream (e.g. social context) and downstream (e.g. digitally mediated prompts) determinants of using digital PN interventions. A piecemeal approach where any one recommendation is enacted is unlikely to gain traction or deliver substantial change in PN outcomes. Given the heterogeneity of contexts in which the contributing studies were conducted, we suggest that our recommendations should be explored locally and with relevant stakeholders (e.g. industry partners, diverse patient groups, healthcare professionals and CBOs). This should ensure they are operationalised in coherent, culturally appropriate, locally tailored and co-produced ways.
Strengths and limitations of the current study
The paper has many important strengths. Throughout the study, we used multiple experts to code, review and audit data and analysis (e.g. quality appraisal, data extraction, and coding using the TDF, Intervention Functions, and BCTT ver. 1). We also used a wide range of disciplinary, and professional perspectives, to ensure the translation of our behavioural science findings into practical recommendations. We drew upon well established, theoretically-based ways of developing recommendations18 and have provided an auditable account of our analytic steps.
However, we restricted inclusion to articles in the English language, which may have excluded some relevant studies. In addition, the specifications of barrier and facilitators statements from a particularly heterogeneous set of original studies required some interpretative work and we did not weight barriers and facilitators according to the original study design or quality. Equally, although the studies identified were conducted across five different countries, we combined their findings into one data set without any sub-population analyses. It is feasible that important cultural or societal differences that may be important are overlooked in our synthesis of barriers and facilitators.28 Additionally, the tools used to develop our recommendations for future intervention content are undergoing revision, including the content of the BCTTv1 and the way in which theoretical mechanisms can be theorised (https://theoryandtechniquetool.humanbehaviourchange.org/).
Future research
As new digital PN interventions are developed, it is crucial to compile a detailed evidence-base to evaluate their efficacy. This would include information about their content, the barriers and facilitators to their use, their population reach, the types of sexual partner for which they are used, and their impact on health inequalities. Furthermore, we should aim to understand the effects of digital PN interventions on non-digital sexual health services (e.g. changes in the pattern of their use and provision). Several of the behavioural science tools used here may be very helpful in achieving these evaluative goals.18 Research using high quality frameworks29 is also needed to deliver cumulative insights into the implementation of digital PN interventions across diverse settings and nations as well as a deep understanding of the effects of such interventions, both positive and negative. Studies of new digital PN interventions should also develop and evaluate comprehensive partner management by the inclusion of testing and treatment, and opportunities for prevention, as appropriate. Future research should also address any similarities and differences in approaches needed for the different infections for which we use PN, notably curable bacterial STIs versus long-term treatable infections such as HIV. PN for HIV, for example, while poorly addressed within the literature reviewed here, presents particular benefits (e.g. the elimination of HIV transmission) yet simultaneously particular challenges (e.g. the criminalisation of HIV transmission, psychosocial impacts of potential HIV exposure).
Conclusion
Our results bring the field a step closer to understanding how to improve future digital PN interventions. We detailed a list of barriers and facilitators to using digital PN interventions and a set of practically oriented, theory-based and evidence-based recommendations that should be taken into consideration by those designing future digital PN interventions. These recommendations are focussed on empowering and supporting the index patient, facilitating index patient choice; integrating digital PN interventions with the existing dating/hook-up digital landscape; enhancing the convenience of digital PN interventions, and perhaps most importantly, normalising PN while presenting it as an act of caring. Together, the recommendations generated here provide a comprehensive systemic solution to improving future digital PN interventions and increasing both acceptability and uptake.
Data availability
The data used to generate the results in the paper are available. Please contact Paul.Flowers@strath.ac.uk for a copy.
Declaration of funding
The work is funded by the UK’s National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (award number NIHR200856).
Acknowledgements
We acknowledge the work of the wider SEQUENCE digital team, Vanessa Apea, Andew Copas, Karen Lloyd, Fiona Mapp, Jonathan O’Sullivan, Tracy Roberts, Jonathan Ross, Pam Sonnenberg, Merle Symonds, Roos van Greevenbroek, Caroline Ward, Andrew Winter and Melvina Woode Owusu and our sponsor Central and North West London NHS Foundation Trust.
References
1 Ward H, Bell G. Partner notification. Medicine 2014; 42(6): 314-317.
| Crossref | Google Scholar | PubMed |
3 van Aar F, van Weert Y, Spijker R, Götz H, Op de Coul E, for the Partner Notification Group. Partner notification among men who have sex with men and heterosexuals with STI/HIV: different outcomes and challenges. Int J STD AIDS 2015; 26(8): 565-573.
| Crossref | Google Scholar | PubMed |
4 Pellowski J, Mathews C, Kalichman MO, Dewing S, Lurie MN, Kalichman SC. Advancing partner notification through electronic communication technology: a review of acceptability and utilization research. J Health Commun 2016; 21(6): 629-637.
| Crossref | Google Scholar | PubMed |
5 Althaus CL, Turner KME, Mercer CH, Auguste P, Roberts TE, Bell G, Herzog SA, Cassell JA, Edmunds WJ, White PJ, Ward H, Low N. Effectiveness and cost-effectiveness of traditional and new partner notification technologies for curable sexually transmitted infections: observational study, systematic reviews and mathematical modelling. Health Technol Assess 2014; 18(2): 1-100.
| Crossref | Google Scholar |
6 Golden MR, Gibbs J, Woodward C, Estcourt CS. Priorities in the implementation of partner services for HIV/STIs in high-income nations: a narrative review of evidence and recommendations. Sex Health 2022; 19(4): 309-318.
| Crossref | Google Scholar | PubMed |
7 Tucker JD, Hocking J, Oladele D, Estcourt C. Digital sexually transmitted infection and HIV services across prevention and care continuums: evidence and practical resources. Sex Health 2022; 19(4): 278-285.
| Crossref | Google Scholar | PubMed |
8 Kachur R, Hall W, Coor A, Kinsey J, Collins D, Strona FV. The use of technology for sexually transmitted disease partner services in the United States: a structured review. Sex Transm Dis 2018; 45(11): 707-712.
| Crossref | Google Scholar | PubMed |
9 Bilardi JE, Fairley CK, Hopkins CA, Hocking JS, Temple-Smith MJ, Bowden FJ, Russell DB, Pitts M, Tomnay JE, Parker RM, Pavlin NL, Chen MY. Experiences and outcomes of partner notification among men and women recently diagnosed with chlamydia and their views on innovative resources aimed at improving notification rates. Sex Transm Dis 2010; 37(4): 253-258.
| Crossref | Google Scholar | PubMed |
10 Estcourt CS, Gibbs J, Sutcliffe LJ, Gkatzidou V, Tickle L, Hone K, Aicken C, Lowndes CM, Harding-Esch EM, Eaton S, Oakeshott P, Szczepura A, Ashcroft RE, Copas A, Nettleship A, Sadiq ST, Sonnenberg P. The eSexual Health Clinic system for management, prevention, and control of sexually transmitted infections: exploratory studies in people testing for Chlamydia trachomatis. Lancet Public Health 2017; 2(4): e182-e190.
| Crossref | Google Scholar | PubMed |
11 Hottes TS, Gilbert M. Evaluation of online partner notification services like inSPOT requires starting with the client, not the clinic. Sex Transm Dis 2012; 39(5): 348.
| Crossref | Google Scholar | PubMed |
12 John SA, Walsh JL, Cho YI, Weinhardt LS. Perceived risk of intimate partner violence among STI clinic patients: implications for partner notification and patient-delivered partner therapy. Arch Sex Behav 2018; 47(2): 481-492.
| Crossref | Google Scholar | PubMed |
13 Clark JL, Segura ER, Oldenburg CE, Salvatierra HJ, Rios J, Perez-Brumer AG, et al. Traditional and web-based technologies to improve partner notification following syphilis diagnosis among men who have sex with men in Lima, Peru: pilot randomized controlled trial. J Med Internet Res 2018; 20(7): e9821.
| Crossref | Google Scholar |
14 Folke T, Menon-Johansson AS. An evaluation of digital partner notification tool engagement and impact for patients diagnosed with gonorrhea and syphilis. Sex Transm Dis 2022; 49(12): 815-821.
| Crossref | Google Scholar | PubMed |
15 Bloch S, Flowers P, Woodward C, McLeod J, Estcourt C, Gibbs J, Lloyd K, Saunders J. Barriers to and facilitators of online partner notification and management pathways for people with sexually transmitted infections (STIs) and HIV and their sex partners: a systematic review and behaviour change wheel analysis. PROSPERO; 2021. Available at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021201746
16 Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, Vedel I, Pluye P. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ for Inform 2018; 34(4): 285-291.
| Crossref | Google Scholar |
17 Wang AL, Peng R-R, Tucker JD, Chakraborty H, Cohen MS, Chen X-S. Optimizing partner notification programs for men who have sex with men: factorial survey results from South China. PLoS ONE 2016; 11(7): e0157749.
| Crossref | Google Scholar | PubMed |
19 Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, Foy R, Duncan EM, Colquhoun H, Grimshaw JM, Lawton R, Michie S. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implementation Science 2017; 12(1): 77.
| Crossref | Google Scholar |
20 Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46(1): 81-95.
| Crossref | Google Scholar | PubMed |
21 Lessard D, Aslan A, Zeggagh J, Morel S, Michels D, Lebouché B. Acceptability of a digital patient notification and linkage-to-care tool for French PrEPers (WeFLASH©): key stakeholders’ perspectives. Int J STD AIDS 2019; 30(14): 1397-1407.
| Crossref | Google Scholar | PubMed |
22 Kutner BA, Pho AT, López-Rios J, Lentz C, Dolezal C, Balán IC. Attitudes and perceptions about disclosing HIV and syphilis results using Smarttest, a smartphone app dedicated to self-and partner testing. AIDS Educ Prev 2021; 33(3): 234-248.
| Crossref | Google Scholar | PubMed |
23 Contesse MG, Fredericksen RJ, Wohlfeiler D, Hecht J, Kachur R, Strona FV, Katz DA. Attitudes about the use of geosocial networking applications for HIV/STD partner notification: a qualitative study. AIDS Educ Prev 2019; 31(3): 273-285.
| Crossref | Google Scholar | PubMed |
24 Yan X, Xu Y, Tucker JD, Miller WC, Tang W. Facilitators and barriers of HIV partner notification services among men who have sex with men in China: a qualitative analysis using a socioecological framework. Sex Transm Dis 2022; 49(8): 541.
| Crossref | Google Scholar | PubMed |
25 Hopkins CA, Temple-Smith MJ, Fairley CK, Pavlin NL, Tomnay JE, Parker RM, Bowden FJ, Russell DB, Hocking JS, Chen MY. Telling partners about chlamydia: how acceptable are the new technologies? BMC Infect Dis 2010; 10(1): 58.
| Crossref | Google Scholar |
26 Carnicer-Pont D, Barbera-Gracia MJ, Fernández-Dávila P, García de Olalla P, Muñoz R, Jacques-Aviñó C, Saladié-Martí MP, Gosch-Elcoso M, Arellano Munoz E, Casabona J. Use of new technologies to notify possible contagion of sexually-transmitted infections among men. Gac Sanit 2015; 29(3): 190-197.
| Crossref | Google Scholar | PubMed |
27 Estcourt CS, Flowers P, Cassell JA, Pothoulaki M, Vojt G, Mapp F, Woode-Owusu M, Low N, Saunders J, Symonds M, Howarth A, Wayal S, Nandwani R, Brice S, Comer A, Johnson AM, Mercer CH. Going beyond ‘regular and casual’: development of a classification of sexual partner types to enhance partner notification for STIs. Sex Transm Infect 2022; 98(2): 108-114.
| Crossref | Google Scholar | PubMed |
28 Lariat J, Chikwari CD, Dauya E, Baumu VT, Kaisi V, Kafata L, Meza E, Simms V, Mackworth-Young C, Rochford H, Machiha A, Bandason T, Francis SC, Ferrand RA, Bernays S. “It’s not safe for me and what would it achieve?” Acceptability of patient-referral partner notification for sexually transmitted infections to young people, a mixed methods study from Zimbabwe. Sex Reprod Health Matters 2023; 31(1): 2220188.
| Crossref | Google Scholar |
29 Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, Boyd KA, Craig N, French DP, McIntosh E, Petticrew M, Rycroft-Malone J, White M, Moore L. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021; 374: n2061.
| Crossref | Google Scholar |