The shadow pandemic: rising syphilis rates in the wake of coronavirus (COVID-19)
Rhea Ahuja A , Nilam Singh B , Kaushal K. Verma A and Somesh Gupta
A , Nilam Singh B , Kaushal K. Verma A and Somesh Gupta  A *
A *
A
B
Abstract
The coronavirus disease 2019 (COVID-19) aftermath left an alarming surge in syphilis cases, contradicting the previously stable trajectory of the infection. US Centers for Disease Control and Prevention also reported a 38% increase in primary and secondary syphilis in 2021 compared to 2019 in the United States, prompting a retrospective analysis at our tertiary care centre in New Delhi, India. There was a persistent linear rise, surpassing pre-COVID levels. Male clinic attendees, exhibit a pronounced increase, likely due to the influence of MSM. Online sexual activity during lockdowns and redirected healthcare resources have possibly contributed to this trend. Urgent measures include strengthened surveillance data collection and public health response, awareness promotion, and early, free treatment. The syphilis surge may signify a broader, undiagnosed STI pandemic, necessitating comprehensive intervention and surveillance.
Keywords: active screening, COVID-19, MSM (men who have sex with men), online sexual activity, safe sexual practices, STIs (sexually transmitted infections), surge, syphilis.
In the aftermath of the coronavirus disease 2019 (COVID-19) pandemic, an unexpected and alarming trend emerged: the resurgence of syphilis, a sexually transmitted infection (STI), previously marked by a stable trajectory. As per US Centers for Disease Control and Prevention, by the end of 2020, reported cases of primary and secondary syphilis had risen by 7% compared to 2019 in the United States. This trend continued in 2021, with the cases increasing by a staggering 38% compared to the numbers in 2019.1 This rise raises questions on the complex interplay between public health crises, sexual behaviours, and healthcare access.
In the post-pandemic era, a striking surge in syphilis cases, was also observed at our tertiary care centre at New Delhi, India. To better understand this trend, we conducted a retrospective analysis of data from our Sexually Transmitted Diseases Clinic spanning 8 years, from January 2015 to October 2023. This daily out-patient clinic, in a central governmental facility provides point-of-care testing and free medications catering to patients with sexually transmitted diseases. These syphilis cases were diagnosed using the conventional screening approach, which involved the initial venereal disease research laboratory test followed by a confirmatory Treponema pallidum haemagglutination assay. This included both clinically symptomatic patients of syphilis (primary and secondary syphilis) and other clinic attendees identified incidentally as a part of routine screening.
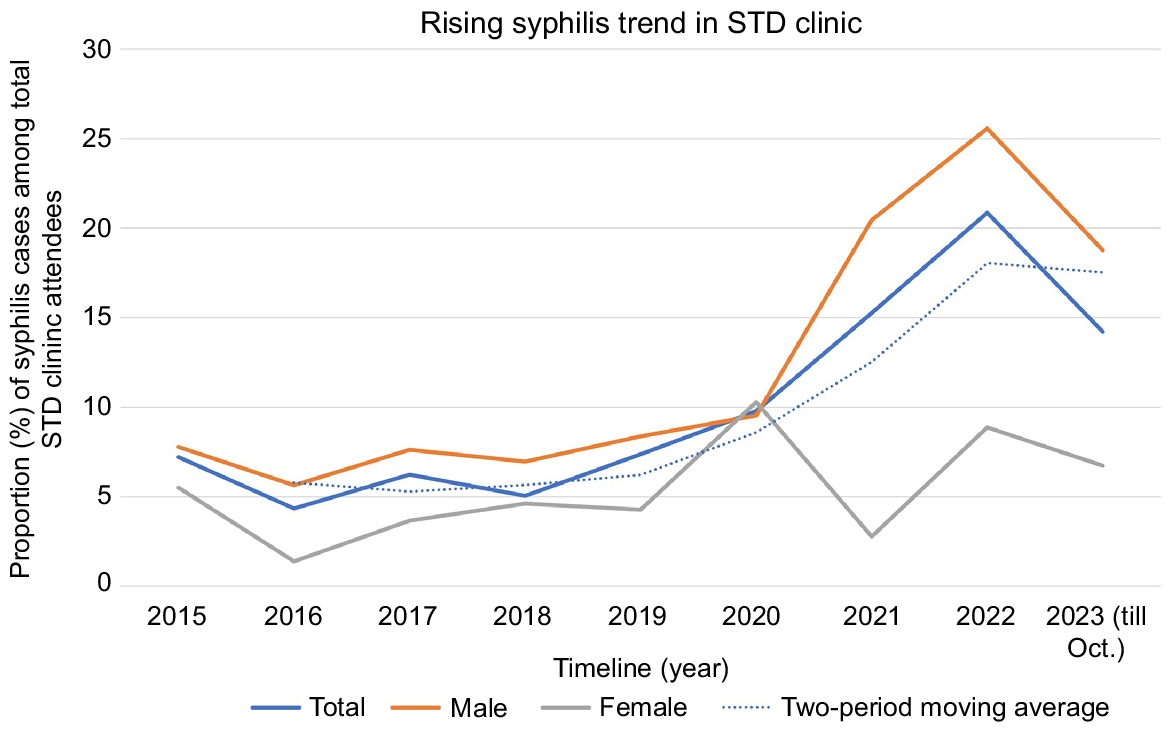
There was a linear increase in the proportion of syphilis reactive cases among all attendees, starting in 2021 (15.26%), rising in 2022 (20.86%) and continuing through to 2023 (Fig. 1). The linear increase was more pronounced when examined through a two-period moving average trendline. In 2023, although there seemed to be a plateau relative to 2022, syphilis rates consistently exceeded pre-COVID levels.
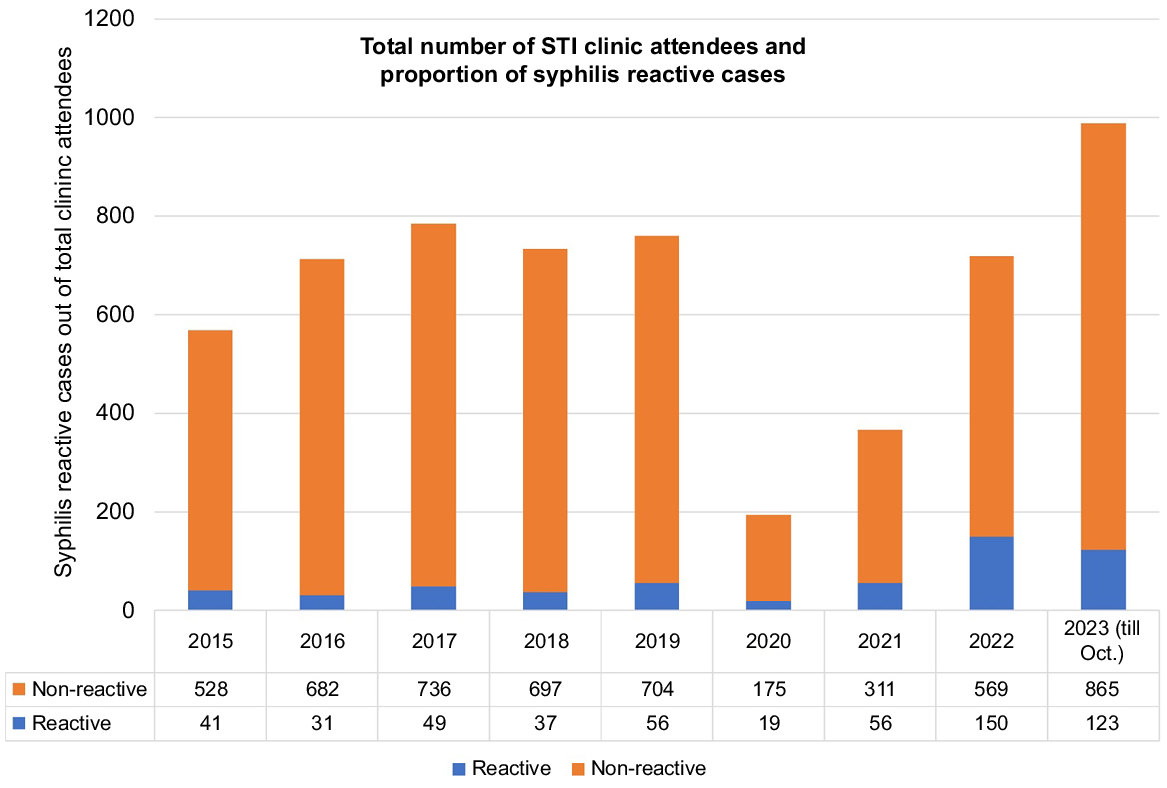
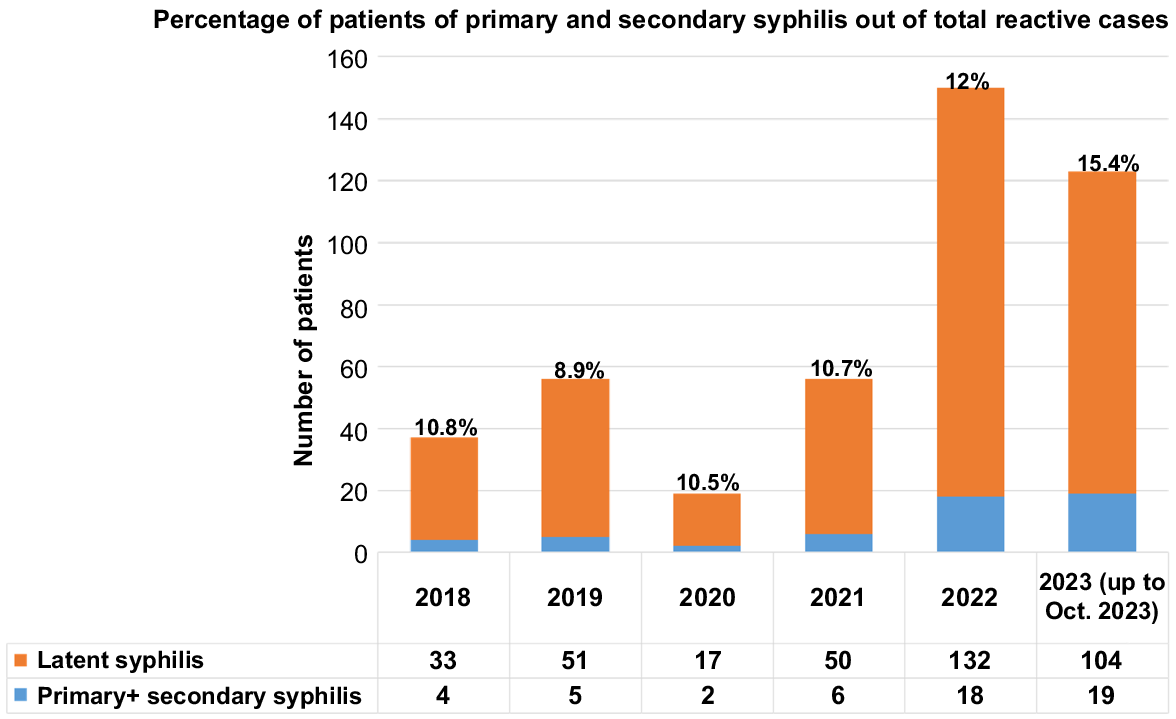
It is worth noting that there was an overall decline in total number of attendees at the STI clinic in 2020 (194 patients) and 2021 (367 patients), from the usual load of around 750 patients. Despite this decline, the proportion of syphilis-reactive cases witnessed a noteworthy increase (7.3% in 2019 to 15.3% in 2021), as shown in Fig. 2. A similar increase was also noted in the number of patients with primary and secondary (symptomatic) syphilis from 8.9% in 2019 to 15.4% in 2023, suggesting an increase in new active cases and possibly increased transmission (Fig. 3). These findings highlight a shifting landscape in the realm of STIs.
Bar diagram showing the total number of STI clinic attendees and proportion of syphilis reactive cases.
Bar diagram showing percentage of patients of primary and secondary syphilis out of total reactive cases.
The increase was more marked in the male clinic attendees compared to female attendees, possibly indicating the potential influence of MSM and their high-risk behaviour in this cohort. However, assessing this trend for MSM specifically posed challenges as they often do not readily disclose their sexual behaviours. All male patients in the STI clinic are routinely asked about high-risk behaviour including engaging in any form of sexual activity with other males.
The significant rise in syphilis cases suggests that despite the implementation of social contact restrictions changes during COVID-19, syphilis transmission remained unchecked, possibly due to public non-compliance with government protective measures.2 The widespread availability of the internet and time spent in isolation likely resulted in online sexual encounters through both conventional and dark web platforms.3 A retrospective observational study on online sexual activity including patients from a STD centre in Caligari, Italy, noted a ‘steady state of syphilis contagiouness’ during lockdown, with patients reporting unprotected sexual encounters despite the restriction measures. The authors reported that the telephone hotlines and smartphone apps designed for dating and sexual interactions remained active despite the lockdown measures.2
Online sexual activity refers to seeking sexual partners online, which may be unknown. In a recent online survey in the US it was found that 705 (66.2%) of 1065 responders reported a new sex partner. Further, 255 of them had met their sex partners using online apps.4
Furthermore, STIs became a marginalised concern in the shadow of the COVID-19 pandemic. Healthcare resources were redirected to prioritise COVID-19, and the persistent fear of contracting severe acute respiratory syndrome coronavirus 2, coupled with ongoing lockdowns, acted as deterrents for individuals seeking medical care. Nagendra et al. reported that in the US only 18% of the previously available STI testing clinics were offering their services.5 This led to reduced medical attention, which may account for the decline in active screening, partner notification, and counselling aimed at promoting safe sexual practices.5
To combat rising syphilis infections, several key actions are imperative:
Strengthening surveillance and public health response: governments should reinforce sexual partner tracing and early notification.
Promoting awareness: encourage adherence to official preventive guidelines and provide education, with a focus on proper condom use, early symptom recognition, and understanding risk factors.
Early and free treatment: offer free pharmacological care for infected individuals to facilitate early treatment and interrupt the transmission chain.
The current syphilis pandemic may represent just the tip of a far-reaching iceberg. Many other STIs (asymptomatic infections such as chlamydia and bacterial vaginosis) could be silently on the rise, often showing no symptoms and escaping routine screening, thus perpetuating their transmission. As we understand the consequences of the syphilis surge, there is an urgent need for comprehensive STI surveillance and intervention, as we strive to prevent another substantial, yet undiagnosed, STI pandemic.
Ethics statement
The patients in this manuscript have given written informed consent to publication of their case details.
Data availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Conflicts of interest
Somesh Gupta is an Associate Editor of Sexual Health. To mitigate this potential conflict of interest they were blinded from the review process. All other authors declare that they have no conflicts of interest.
References
2 Bonato F, Ferreli C, Satta R, Rongioletti F, Atzori L. Syphilis and the COVID-19 pandemic: did the lockdown stop risky sexual behavior? Clin Dermatol 2021; 39(4): 710-713.
| Crossref | Google Scholar | PubMed |
3 Evangelou K, Rozani S, Pafiti M, Syrigos N. Syphilis transmission: exacerbated due to the COVID-19 pandemic? Ethics Med Public Health 2022; 22: 100782.
| Crossref | Google Scholar | PubMed |
4 Hamill MM, Yu T, Armington GS, Hsieh Y-H, Manabe YC, Melendez JH. Factors associated with new sexual partnerships during the COVID-19 pandemic: a survey of online sexually transmitted infection testing platform users. Sex Transm Dis 2022; 49(10): 695-699.
| Crossref | Google Scholar | PubMed |
5 Nagendra G, Carnevale C, Neu N, Cohall A, Zucker J. The potential impact and availability of sexual health services during the COVID-19 pandemic. Sex Transm Dis 2020; 47(7): 434-436.
| Crossref | Google Scholar | PubMed |