Syphilis in pregnancy: a qualitative investigation of healthcare provider perspectives on barriers to syphilis screening during pregnancy in south-east Queensland
Sarah Warzywoda A * , James A. Fowler
A * , James A. Fowler  A , Clare Nourse
A , Clare Nourse  B C , Mandy Wu
B C , Mandy Wu  B D , Sumudu Britton
B D , Sumudu Britton  B E , Diane Rowling
B E , Diane Rowling  F , Paul Griffin
F , Paul Griffin  B G , Mattea Lazarou
B G , Mattea Lazarou  A D , Zoe Hamilton A and Judith A. Dean
A D , Zoe Hamilton A and Judith A. Dean  A
A
A The University of Queensland, Faculty of Medicine, School of Public Health, 288 Herston Road, Herston, Qld 4006, Australia.
B The University of Queensland, Faculty of Medicine, School of Medicine, 288 Herston Road, Herston, Qld 4006, Australia.
C Infection Management and Prevention Service, Queensland Children’s Hospital, Children’s Health Queensland Hospital and Health Service, 501 Stanley Street, South Brisbane, Qld 4101, Australia.
D Queensland Children’s Hospital, Children’s Health Queensland Hospital and Health Service, 501 Stanley Street, South Brisbane, Qld 4101, Australia.
E Department of Infectious Diseases, Royal Brisbane and Women’s Hospital, Metro North Hospital and Health Service, 7 Butterfield Street, Herston, Qld 4029, Australia.
F Metro North Public Health Unit, Metro North Hospital and Health Service, Bryden Street, Windsor, Qld 4030, Australia.
G Mater Health Brisbane, Raymond Terrace, South Brisbane, Qld 4101, Australia.
Sexual Health 20(4) 330-338 https://doi.org/10.1071/SH22193
Submitted: 7 December 2022 Accepted: 8 May 2023 Published: 29 May 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: Increasing rates of syphilis in pregnancy (SiP) in Australia and other high-income countries, has led to the resurgence of congenital syphilis. Suboptimal syphilis screening during pregnancy has been identified as a key contributing factor.
Methods: This study aimed to explore, from the perspective of multidisciplinary healthcare providers (HCPs), the barriers to optimal screening during the antenatal care (ANC) pathway. Semi-structured interviews conducted with 34 HCPs across multiple disciplines practising in south-east Queensland (SEQ) were analysed through a process of reflexive thematic analysis.
Results: Barriers were found to occur at the system level of ANC, through difficulties in patient engagement in care, limitations in the current model of health care delivery and limitations in the communication pathways across health care disciplines; and at the individual HCP level, through HCP knowledge and awareness of epidemiological changes in syphilis in SEQ, and adequately assessing patient risk.
Conclusion: It is imperative that the healthcare systems and HCPs involved in ANC address these barriers to improve screening in order to optimise management of women and prevent congenital syphilis cases in SEQ.
Keywords: congenital syphilis, healthcare provider, infectious syphilis, pregnancy, qualitative, sexually transmitted infection, syphilis, syphilis in pregnancy.
Introduction
Syphilis, caused by the bacterium Treponema pallidum, is predominantly a sexually transmissible infection (STI). However, untreated infection during pregnancy can result in vertical transmission from mother to child, leading to congenital syphilis and multiple obstetric and neonatal complications.1–3 Syphilis in pregnancy (SiP) results in high neonatal mortality and morbidity (intrauterine fetal death, premature birth, fetal distress, and severe neonatal multi-organ disease) and globally remains the second leading cause of stillbirth.1–6
Over the past decade, there has been a nine-fold increase (from 15.4 to 135.8 per 100 000) in notification rates of infectious syphilis in Queensland, with transmission occurring predominantly via male-to-male sexual contact.2,7,8 Since 2011, Queensland has been experiencing an as yet, uncontained epidemic among rural and remote Aboriginal and Torres Strait Islander communities.2 Occurring predominately through heterosexual transmission, this has also led to rates of SiP continuing to rise.2 However, an emerging issue is occurring among women in the south-east metropolitan region of Queensland (south-east Queensland; SEQ) where there has been a seven-fold increase in notification rates among non-Indigenous women of reproductive age since 2016.2 This increasing trend in notifications is reflected in other Australian jurisdictions and other high-income countries, including Canada and the US.3,4,8–10
Increasing rates of syphilis in women of reproductive age have corresponded with an increase in the incidence of congenital syphilis4 with Queensland recording 33 cases of congenital syphilis since 2001 with 12 resulting in infant death.2 The adverse perinatal outcomes associated with congenital syphilis are preventable through early serological detection and treatment of maternal syphilis during antenatal care (ANC)5 – the series of up to 10 planned/scheduled visits provided during pregnancy in community, primary health care and hospital-based settings by midwives, general practitioners (GPs) and specialists, to improve the wellbeing of both mother and baby.11 Despite high rates of ANC attendance across Australia (85% in 2018), the rates of congenital syphilis are continuing to rise.2,8,11 Suboptimal serological screening during pregnancy has been identified as a contributing factor.3,7,12,13
Congenital syphilis has been considered a disease of the past and therefore, its re-emergence is a sentinel health event that calls for reflection on where breakdowns in the public health and ANC systems are occurring.5,12,14,15 This paper presents the barriers to optimal syphilis screening from the perspective of multidisciplinary healthcare providers (HCPs), including GPs, midwives and specialists who provide care along the ANC pathway in primary health care and both public and private secondary and tertiary healthcare settings. The authors acknowledge the diversity of people with reproductive capacity and that not all people accessing ANC may identify as women. For the purpose of this paper, ‘woman’ and ‘women’ are respectfully used as inclusive terms by the authors and verbatim in the study participants quotes.
Materials and methods
Study participants
A convenience sample of 34 HCPs practising in SEQ, Australia, was recruited via targeted recruitment and snowball sampling. Targeted recruitment was conducted via emails to HCPs known to the research team to have previous experience providing ANC and/or experience managing SiP and/or congenital syphilis. The remainder were recruited via snowball sampling with participants asked at interviews and in a follow-up thank you emails to share study information within their broader professional networks. To be eligible participants had to be over 18 years of age and currently practicing as a licenced healthcare professional under their relevant National Registration and Accreditation Board with the Australian Health Practitioner Regulation Agency.
Data collection
Semi-structured interviews, conducted either in person (at the workplace of the HCP), via web-based platforms (Zoom) or by telephone, were led by the primary investigator (JD) a female senior research fellow with extensive experience as a registered midwife and sexual health nurse, with the assistance of an additional member of the research team with experience in qualitative research and interview methods (ML or JF). No additional individuals other than two researchers and the participant were present at the time of interviews. An interview guide was used to investigate the range of factors that can impact the screening and management of maternal and congenital syphilis, such as current practices, awareness of guidelines, clinic screening protocols and risk identification. Research information (e.g. the research aims, participant requirements, risks and benefits) was provided to participants prior to interviews. Informed consent was obtained at the time of interviews prior to commencement of recording. During interviews the experience of the interview team was provided to participants to provide context, build rapport and facilitate free exchange of clinical perspectives. Interviews were between 40 and 60 min, and participants were offered AUD$150 gift-card vouchers as a ‘thank you’ for their time. Interviews were not repeated and transcripts were not provided to participants for additional comment.
Data analysis
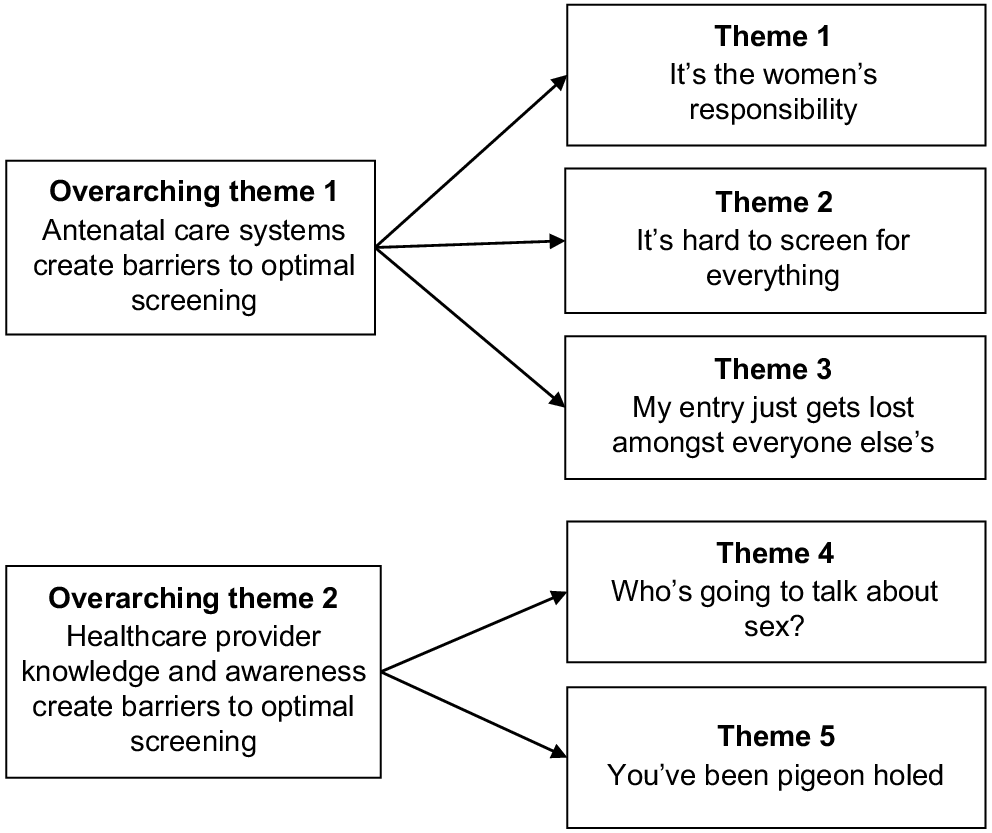
Interviews were digitally recorded and transcribed verbatim through a professional transcription service. Field notes were also made throughout interviews to assist with iterative data analysis and preliminary identification of ideas to explore in future interviews.16 Data were then coded by two of the investigators/authors (SW, JF) using inductive reflexive thematic analysis following the method developed by Braun and Clarke.17 NVivo12 qualitative data analysis software was used to store and manage data.18 Initially, eight codes were generated by SW and JF following a process of reading and re-reading interviews to explicate eight areas of interest. These were discussed with JD and following resolution of inconsistencies and discrepancies, one researcher (SW) conducted further analysis within the category of ‘screening’ to identify and develop further sub-codes. These sub-codes were developed into themes pertaining to screening for SiP through a continual process of deliberation between JF, SW, and JD. Group deliberation with all authors, many of whom have extensive clinical experience working in sexual and reproductive health and/or infectious disease and providing ANC, was undertaken during the reviewing process to help resolve biases that occurred naturally during analysis. Furthermore, group deliberation provided context to the experiences of participants with similar occupational backgrounds to help inform the connections between systems and individuals that make the crux of the analysis. A thematic map is provided in Fig. 1 to summarise the relationship between themes.
Results
As described in Table 1, our sample engaged HCPs from a diverse range of specialities practising in primary (GPs) and both private and public secondary and tertiary healthcare settings (midwives, nurses, infectious diseases physicians, obstetricians, paediatricians). Most participating HCPs reported having been involved in the clinical care of at least one case of SiP in the previous 12 months, and those that were engaged with screening reported that they conducted routine syphilis serology at first ANC visit, with repeat testing based on risk.
| Category | n | ||||
|---|---|---|---|---|---|
| Age (years) (mean = 46.21 years) | 20–29 | 6 | |||
| 30–39 | 6 | ||||
| 40–49 | 7 | ||||
| 50–59 | 10 | ||||
| 60+ | 5 | ||||
| Gender | Male | 6 | |||
| Female | 28 | ||||
| Healthcare setting | Public hospital | 18 | |||
| Private hospital | 5 | ||||
| Clinic (e.g. general practice; sexual health service) | 11 | ||||
| Specialty | Resident medical officer | 2 | |||
| Sexual health physician | 2 | ||||
| Nurse practitioner | 2 | ||||
| Public health nurse | 2 | ||||
| Obstetrician | 2 | ||||
| ID physician | 3 | ||||
| Paediatrician | 4 | ||||
| GP | 5 | ||||
| Midwife | 12 | ||||
| Years in specialty (n = 31) | 1 | 1 | |||
| 2 | 1 | ||||
| 3 | 4 | ||||
| 4 | 2 | ||||
| 5–10 | 10 | ||||
| 11–20 | 10 | ||||
| 20+ | 3 | ||||
| Number of syphilis in pregnancy patients managed in the past year (n = 30) | 0 | 10 | |||
| 1 | 7 | ||||
| 2 | 5 | ||||
| 3 | 2 | ||||
| 4 | 2 | ||||
| 5–10 | 4 | ||||
| Number of syphilis in pregnancy patients managed in the past 10 years (n = 27) | 0 | 8 | |||
| 1 | 5 | ||||
| 2 | 5 | ||||
| 3 | 3 | ||||
| 4 | 1 | ||||
| 5–10 | 4 | ||||
| >20 | 1 | ||||
| Syphilis testing practices | Routinely | As indicated by risk | No | NA | No response |
|---|---|---|---|---|---|
| 1st ANC visit | 24 | 0 | 0 | 9 | 1 |
| 1–16 weeks | 2 | 8 | 2 | 15 | 7 |
| 16–24 weeks | 0 | 10 | 2 | 14 | 8 |
| 26–28 weeks | 6 | 16 | 0 | 9 | 3 |
| 34–36 weeks | 1 | 19 | 0 | 10 | 4 |
| At birth | 0 | 19 | 0 | 9 | 6 |
n, number; ID, infectious disease physician; GP, general practitioner; NA, not applicable/not involved with antenatal care (ANC).
Several common factors that influenced screening practices and the diagnosis of syphilis during pregnancy were identified. These factors can be summarised into two overarching themes that reflect barriers to optimal testing: (1) ANC systems; and (2) HCP knowledge and awareness. Identified themes within each overarching theme, which describe the factors influencing syphilis screening, are detailed below.
Overarching theme 1: ANC systems create barriers to optimal screening
Participants described a range of scenarios that occur across the ANC system that hinder the provision of optimal syphilis screening in pregnancy. Within this broader overarching theme, HCPs describe difficulties in engaging women in care; limitations of both the current model of health care (short consultations times) and the communication systems across health care disciplines.
Participants described ANC models as generally relying on women to take ‘responsibility’ and be ‘self-directed’ in their pregnancy health care. This expectation could lead to sub-optimal testing depending on patients level of engagement, health literacy and socio-economic situation. HCPs acknowledged that women who are proactive and engaged with health care will predominantly be screened and treated at the appropriate time. However, HCPs described cases where late and/or inconsistent engagement in ANC resulted in women being absent at scheduled antenatal appointments, especially if the women were experiencing competing life ‘priorities’.
The pathologist could be just like a little walk down the road… there’s just other things going on in their life where that is not their priority… having a blood test. (Midwife)
Some women, as described by one HCP as a ‘chaotic group with difficult life circumstances’, were often among those who were considered the hardest to engage and maintain in care. While the ‘at risk’ characteristic of this group could be determined to align with the Queensland Syphilis in Pregnancy Guidelines recommendations for repeat testing throughout pregnancy,12 the challenges and/or failure to engage these women in ANC were noted as key barriers to adequate testing and follow-up.
Sometimes we give pathology out and then they don’t get it done; or if they haven’t had very much antenatal care, or if they’re not engaging, or if they’re just kind of… a bit loose around their pregnancy. (Midwife)
Across disciplines, it was generally acknowledged that short consultation times created constraints on conducting comprehensive ANC and in-depth risk assessments. The impact of these time constraints was felt within primary health care and across the shared-care arrangements (where GPs generally conduct the initial antenatal consultations and syphilis serology and then ANC is conducted across two or more HCPs19) with most HCP describing it as hard to ‘do everything’ in the allocated appointment time.
In the 15 minutes, I’m expected to cover –…the blood pressure…listen to the fetal heart, discuss any blood investigations, look at any ultrasound … discuss any birth plans, discuss any concerns. Talk about aspirin, talk about the safer baby bundle, talk about movement…make sure no bloods have been missed, explain the rationale. And this is all in 15 minutes. (Obstetrician)
It was noted by several participants practicing in the tertiary ANC setting, including midwifery care programs, that GPs were ‘really fantastic’ at screening for syphilis and other STIs; however, others considered the time constraints faced in the general practice system prevented comprehensive care. These time constraints made it ‘hard to screen for everything’, forcing HCPs to ‘stick to the important things’, meaning sexual health and STI conversations were often left out. These time constraints were not unique to general practice setting. This led to the acknowledgement across HCP disciplines and practice settings of wider inequities in the public healthcare system whereby women’s access to comprehensive care was dependent on the time afforded to various practitioners and the expectations of service delivery.
From the midwife perspective, they are given 30 to 40 minutes to do a booking in. A doctor appointment slot is 15 minutes… what they have priority [for] in 30 minutes, I’m expected to cover in 15 minutes. (Obstetrician)
Communication across the multidisciplinary teams involved with ANC was cited by several HCPs as a barrier to ‘best practice’ screening. Reliance on paper-based records and patients to deliver information between providers and shared-care facilities was also seen to have its limitations. This lack of consistency in the methods of communication across teams left room for error and missed opportunities for appropriate testing to occur:
The woman did have her bloods done but there wasn’t enough serum left to do the syphilis test. Thing on the bottom of the form from the pathologist saying please retest, not enough blood. The doctor didn’t see it and she was that baby… she was exposed… (Nurse)
Communication challenges were compounded by limitations in the Electronic Medical Record (EMR) system, especially the lack of ability to ‘flag’ important information. HCPs were required to ‘cut and paste’ information across multiple records to ensure that information was being carried across health care disciplines. Missing information could have contributed to missed or unnecessary testing.
They repeat and these poor women just do what they’re told often so they’ll repeat RPR (Rapid Plasma Reagin) you know a week later even though I’ve already done one because it’s under a different UR (patient record number). (Infectious Disease Physician)
Limitations in the ability to accurately identify and share patient records and important information such as testing history across facilities involved with ANC was also seen as a limitation of the EMR if people were accessing multiple services for care:
All the individual hospitals have a different UR. Some of these women will have eight UR’s. (Infectious Disease Physician)
Overarching theme 2: HCP knowledge and awareness create barriers to optimal screening
The second overarching theme centred around deficits in HCP knowledge and awareness of the changing epidemiology of syphilis in SEQ, as well as their ability and comfort to discuss sexual health with pregnant women. These deficits influenced HCP assumptions about women’s levels of risk and resulted in risk assessments not being conducted, leading to sub-optimal testing.
Some HCPs cited hesitation in discussing sexual health with women due to concerns around ‘scaring clients off’, and the need to build a rapport with them first, describing them as ‘uncomfortable conversations to have with a woman’. Others reported that these were ‘not the sort of questions that we ask in an antenatal booking-in’, and only asked detailed questions if prompted to when a referral ‘comes back with some red flags’. Others relied on the woman to instigate sexual health conversations, which can present challenges due to differences in perceptions of ‘normality’ and risks of sexual behaviours across various groups and cultures.
We’re presuming they have an understanding the same as us but… we know that that’s not right. So I think it’s quite hard to say ‘Okay are you having sex with six men?… How are you having it?’ You know, who’s going to ask them that? And the woman will go ‘Oh I’m just having it normal.’ What’s normal to her? I don’t know what’s normal to her. Or to that person and that one man. (Midwife).
Others expressed developing a ‘fine-tuned ESP [extrasensory perception]’ with their clients that came from experience, which may or may not lead to asking more direct questions about risks. While others showed complete avoidance of the topic, particularly around the possibility of addressing their patients’ male partners having sex with other men, despite previously managing multiple cases of SiP:
Who’s going to ask about [a woman’s male partner having] sex with men …not me, I’m not asking. (Obstetrician)
Many HCPs acknowledged a lack of awareness in the epidemiological changes of syphilis in SEQ. This resulted in women being ‘pigeon-holed’ as high risk through the assumption that ‘there’s only certain populations that have syphilis’. Some HCPs felt that this process of assuming based on demographics rather than behavioural risk was ‘judgemental’, causing some women to be unnecessarily singled-out purely for their demographic background.
They say the Aboriginal group need to be retested, but some of our Aboriginal group are not transient…they’ve got a house, they’re married, they’ve had one partner, and yet, they’re still subjected to the same – and sometimes, I think, well, I would find that offensive. (Midwife)
Just as these assumptions lead to the unnecessary testing of some women, it also led to lack of testing in others, with low sexual risks presumed based on ‘religious background’, ‘family values’, or being their ‘family doctor’. Some HCPs believed syphilis risk was not a concern for their patients, being described as ‘a bit conservative’ or residing in a ‘privileged affluent area’, resulting in perceptions that women at risk are ‘not a group I would see here’.
[It’s assumed] that they live behind a white picket fence and it’s just ma and pa and … you know that they’re monogamous… (General Practitioner)
This lack of awareness of epidemiological changes in risk profiles led to missed screening of positive cases for women, ultimately leading to congenital syphilis.
I’ve been caught out with baby who was a congenital syphilis baby…that person wasn’t, didn’t fit into those categories at risk. (Nurse)
Discussion
This study highlights barriers in syphilis screening across SEQ in ANC service systems including time constraints, communication across disciplines and patient engagement, individual HCP knowledge and awareness of epidemiological changes, and the ability to speak about sexual health and conduct risk assessments. Our findings suggest that it is important to consider the interaction between the individual and system-level barriers. For example, professional development may assist in addressing the individual barriers identified but the risk of sub-optimal syphilis testing will remain if the limitations identified within the existing model for health care are not addressed.
When this study was conducted, Queensland guidelines recommended initial syphilis serology during the first trimester (prior to 12-weeks’ gestation), and repeat testing after initial serology in the first trimester was conducted based on patient’s behavioural and demographic risk factors (including substance use, sexual risk behaviours, inadequate ANC and identifying as an Aboriginal and Torres Strait Islander person or having an Aboriginal or Torres Strait Islander partner).12,20 This need to identify risk was identified by our participants as a barrier to offering optimal screening for women at risk. For some, this was related to a lack of awareness of the changing epidemiology of syphilis and who was considered ‘at risk’ and in need of repeat testing. They also noted that syphilis occurs in women falling outside of predefined risk categories, and this has resulted in HCPs offering inadequate testing and follow-up.2,12 This gap in knowledge translation was further compounded by assumptions and judgements made about certain ‘types’ of women, the general reluctance to discuss sexual risks with pregnant women across multidisciplinary HCPs involved in this study, and a reliance on patient disclosure of ‘risky’ behaviours rather than a systematic history taking for behavioural or demographic risk. A reliance on patients’ perceptions of sexual risk and their willingness to discuss sexual behaviour is a flawed strategy, as highlighted in our research, because the perception of sexual risks can vary across different people, groups, and cultures.21–25
The practice of defining risk based on assumption rather than a risk assessment is not isolated to Queensland or Australia. Case studies from the Netherlands, Italy, and US highlight the adverse impacts of making incorrect assumptions of ‘low risk’, including delayed diagnoses of congenital syphilis.26–28 One strategy to overcome this barrier is the implementation of universal repeat syphilis serology at 28 and/or 36 weeks. Western Australia implemented universal repeat serology in March 202112,29 and Queensland has followed with an update to the Queensland Syphilis in Pregnancy Guidelines released in October 2022 now recommending routine repeat syphilis serology screening for all women at 26–28 weeks gestation.20 This recent change to Queensland guidelines may assist with overcoming inaccurate risk assessments and avoidance of sexual health conversations highlighted in our study, thereby aiding earlier detection of SiP and the reduction of potential adverse neonatal health outcomes.30 Cost–benefit analyses in other high-income countries including the US and UK have found that universal rescreening is not cost-effective when syphilis prevalence is low.31,32 However, considering recent epidemiological changes in Australia, some HCPs from our study are suggesting a need for routine re-testing to be introduced in all jurisdictions. Further research, including cost-benefit analysis, for the Australian context may be beneficial in guiding if these changes should be nationwide.
Another common perception noted in our study was that the routine 15-min consultation times limited HCP ability to provide comprehensive ANC, especially for women with complex diverse needs such as domestic violence, multiple social health problems, low health literacy, and or cultural and language barriers.33,34 This combined with our identified lack of HCP knowledge about how to assess risk in the changing epidemiological climate of syphilis in SEQ, suggests that the current models of ANC make it ‘hard to engage’ women and provide comprehensive responsive ANC. A situation that can result in potentially wider implications for health outcomes during the perinatal period.34 However, even with addressing these system and HCP level barriers, there remains a reliance on women attending ANC, and our study suggests that HCPs can face challenges keeping women with complex needs engaged and retained in care. This is supported by Australian data that report approximately 20% of Australian women in 2019 did not attend their initial ANC appointment, with these proportions increasing to over 30% for women who would be considered higher risk.11 Models of care that allow for additional time, support, and effort from HCPs are required to navigate both the HCP and individual factors affecting access to optimal testing identified in this study. For example, group ANC and midwifery-led ANC have been found to effectively increase time and support afforded to women and pregnant people, particularly those considered harder to engage.35–41 Continuity of care and caseload-midwifery models that involve outreach, home visits and culturally sensitive care from the same midwife through pregnancy, labour, and early postnatal period have also been successful in Aboriginal and Torres Strait Islander health services in Australia.40,42,43 These models are shown to increase patient-HCP trust, patient satisfaction, and retention in ANC through open communication and increased support networks, and also allow for greater adherence to screening needs by offering care in flexible, culturally safe environments that are responsive to the individual’s needs and lived experiences.35–43 Such models could readily translate to other, higher risk communities but have not been widely promulgated to date.
Early screening and treatment of syphilis during pregnancy is imperative to prevent adverse outcomes for both mother and neonate.30,44 Our study highlights that HCP’s knowledge and awareness of syphilis, and ‘best practice’ screening needs to be improved urgently. Available mechanisms include knowledge promotion, support systems such as the Queensland Syphilis Surveillance Service, clear referral pathways and clinical support services and ensuring resources such as the Queensland Syphilis in Pregnancy Guidelines and Australian Guidelines for STI Management in Primary Care are both easily accessible and regularly updated to reflect current epidemiological changes.12,20,45–47 HCPs also have a responsibility to provide the best possible care to patients and to do this they need to keep up to date with evidence, however, our study suggests that information about current best practice and up-to-date guidelines may not be adequately reaching all HCPs.
The interactions described above highlight that to overcome barriers, both system and individual levels need to be considered together rather than treated as distinct areas. For example, increasing consultation times, especially for GPs in primary care, may bring benefit, but only if women are appropriately engaged and HCPs are suitably skilled and prepared to discuss sexual risk behaviour. Additionally, increasing provider knowledge may improve screening and awareness of syphilis; however, if the limitations in effective communication across teams is not also addressed, then lack of translation of information may still result in missed diagnoses and delayed treatment. Recommendations on how to improve STI risk assessments and syphilis screening in ANC could further be explored through co-design with HCP. However, exploration into the views of at-risk populations including women diagnosed with syphilis during pregnancy would provide valuable contextualised understanding that may strengthen acceptability and uptake. Recruitment of women diagnosed with syphilis during pregnancy was attempted during this study; however, a combination of challenges including loss to follow-up of women who had expressed interest in participating in an interview, were experienced. HCP participants and the clinical investigators on this study suggest these challenges were primarily associated with women not wanting to engage in these conversations during or following treatment due to their ‘shame’ around their diagnosis and wanting to ‘leave syphilis in the past’. These challenges were exacerbated by coronavirus disease 2019 (COVID-19) public health restrictions and recruitment was ceased.
Strengths and limitations
Strengths of this study were through the broad selection of HCPs that were included, providing a range of experiences and information on the current screening practices across the various disciplines of ANC in SEQ. The various roles, experiences and expertise held by the researchers across various health care disciplines (including nursing, midwifery, medical and public health backgrounds) also provided breadth in interpretation of the results. Limitations of the study included under representation of health care disciplines (such as nurses and infectious disease specialists) with midwife’s constituting over one-third (35%) of respondents. Increased demands of the COVID-19 pandemic also potentially limited HCP provider capacity to engage in the research. Further to this, the impacts of the COVID-19 pandemic (known to have had various impacts and disruptions to ANC care delivery48) were not extensively explored in this study. As some of the sample was known to the research team, this may have induced social desirability bias, potentially motivating participants to provide answers not indicative of their usual practice. As well, participants were told the aims of the study were to explore SiP, which may have encouraged individuals to learn about screening and management guidelines that had not previously been used as part of their clinical practice. Finally, given our reliance on purposive sampling, the experiences of HCP not within the researcher’s networks may be limited in this analysis; however, the use of snowball sampling assisted in expanding the sample diversity. These factors should therefore be taken into consideration when interpreting the results of this study.
Conclusion
Over the past decade, maternal and congenital syphilis rates have been increasing, with barriers during ANC potentially contributing to inadequate screening during pregnancy and missed opportunities for early diagnosis and treatment. This qualitative exploration of HCP perspectives uncovered difficulties in the processes of syphilis screening during pregnancy occurring at the healthcare system level and in the individual HCPs knowledge and practices. To combat the continued rise in SiP and congenital syphilis cases in SEQ and to improve maternal and neonatal health outcomes for all pregnant women and people with reproductive capacity, it is imperative that the intersection of these individual barriers and the systems limitations be addressed.
References
1 World Health Organization (WHO). Data on syphilis. World Health Organization. 2020. Available at https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/data-on-syphilis
3 Victorian Government Department of Health. Congential syphils in Victoria: health advisory. 2021. Available at https://www.health.vic.gov.au/health-advisories/congenital-syphilis-in-victoria
4 Australasian Society for HIV Viral Hepatitis and Sexual Health Medicine (ASHM). Syphilis. Australian STI Management Guidelines for use in Primary Care. 2021. Available at https://sti.guidelines.org.au/sexually-transmissible-infections/syphilis/
5 Thean L, Moore A, Nourse C. New trends in congenital syphilis: epidemiology, testing in pregnancy, and management. Curr Opin Infect Dis 2022; 35(5): 452-60.
| Crossref | Google Scholar |
6 Qin J, Yang T, Xiao S, Tan H, Feng T, Fu H. Reported estimates of adverse pregnancy outcomes among women with and without syphilis: a systematic review and meta-analysis. PLoS ONE 2014; 9(7): e102203.
| Crossref | Google Scholar |
7 Wu M, Seel M, Britton S, Dean JA, Lazarou M, Safa H, et al. Addressing the crisis of congenital syphilis: key findings from an evaluation of the management of syphilis in pregnancy and the newborn in South-East Queensland. Aust N Z J Obstet Gynaecol 2022; 62(1): 91-7.
| Crossref | Google Scholar |
9 Centre for Disease Control and Prevention. Sexually transmitted infections treatment guidelines, 2021: congential syphilis 2021. Available at https://www.cdc.gov/std/treatment-guidelines/congenital-syphilis.htm
11 Australian Institute of Health and Welfare (AIHW). Australia’s mothers and babies. Australian Government; 2021. Available at https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-babies-data-visualisations/contents/antenatal-period/antenatal-care
13 Australian Government Department of Health. Pregnancy care guidelines: syphilis. Commonwealth of Australia. 2019. Available at https://www.health.gov.au/resources/pregnancy-care-guidelines/part-f-routine-maternal-health-tests/syphilis
14 Zenker PN, Berman SM. Congenital syphilis: reporting and reality. Am J Public Health 1990; 80(3): 271-2.
| Crossref | Google Scholar |
15 DiOrio D, Kroeger K, Ross A. Social vulnerability in congenital syphilis case mothers: qualitative assessment of cases in Indiana, 2014 to 2016. Sex Transm Dis 2018; 45(7): 447-51.
| Crossref | Google Scholar |
16 Srivastava P, Hopwood N. A practical iterative framework for qualitative data analysis. Int J Qual Methods 2009; 8(1): 76-84.
| Crossref | Google Scholar |
18 QSR International Pty Ltd. NVivo (Released in March 2020). 2020. Available at https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
19 Agency for Clinical Innovation. Acute shared care models/pathways. NSW Government. 2023. Available at https://aci.health.nsw.gov.au/networks/aged-health/about/building-partnerships/acute-shared-care-models
20 Queensland Health. Queensland clinical guidelines: guidline history. Queensland Government. 2022. Available at https://www.health.qld.gov.au/qcg/guidelinehistory
22 Clifton S, Mercer CH, Sonnenberg P, Tanton C, Field N, Gravningen K, et al. STI risk perception in the British population and how it relates to sexual behaviour and STI healthcare use: findings from a cross-sectional survey (Natsal-3). EClinicalMedicine 2018; 2–3: 29-36.
| Crossref | Google Scholar |
23 Gravningen K, Braaten T, Schirmer H. Self-perceived risk and prevalent chlamydia infection among adolescents in Norway: a population-based cross-sectional study. Sex Transm Infect 2016; 92(2): 91-6.
| Crossref | Google Scholar |
24 Lim MSC, Hellard ME, Aitken CK, Hocking JS. Sexual-risk behaviour, self-perceived risk and knowledge of sexually transmissible infections among young Australians attending a music festival. Sex Health 2007; 4(1): 51-6.
| Crossref | Google Scholar |
25 Harville EW, Giarratano GP, Buekens P, Lang E, Wagman J. Congenital syphilis in East Baton Rouge parish, Louisiana: providers’ and women’s perspectives. BMC Infect Dis 2021; 21(1): 64.
| Crossref | Google Scholar |
26 Keuning MW, Kamp GA, Schonenberg-Meinema D, Dorigo-Zetsma JW, van Zuiden JM, Pajkrt D. Congenital syphilis, the great imitator – case report and review. Lancet Infect Dis 2020; 20(7): e173-e9.
| Crossref | Google Scholar |
27 Bembry W, Anderson M, Nelson S. Congenital syphilis: the great pretender strikes back. A case report. Clin Pediatr 2018; 57(8): 992-6.
| Crossref | Google Scholar |
28 Onesimo R, Buonsenso D, Gioè C, Valetini P. Congenital syphilis: remember to not forget. BMJ Case Rep 2012; 2012: bcr0120125597.
| Google Scholar |
30 Hawkes SJ, Gomez GB, Broutet N. Early antenatal care: does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta-analysis. PLoS ONE 2013; 8(2): e56713.
| Crossref | Google Scholar |
31 Huntington S, Weston G, Seedat F, Marshall J, Bailey H, Tebruegge M, et al. Repeat screening for syphilis in pregnancy as an alternative screening strategy in the UK: a cost-effectiveness analysis. BMJ Open 2020; 10(11): e038505.
| Crossref | Google Scholar |
32 Albright CM, Emerson JB, Werner EF, Hughes BL. Third-trimester prenatal syphilis screening: a cost-effectiveness analysis. Obstet Gynecol 2015; 126(3): 479-85.
| Crossref | Google Scholar |
33 Brown SJ, Sutherland GA, Gunn JM, Yelland JS. Changing models of public antenatal care in Australia: is current practice meeting the needs of vulnerable populations? Midwifery 2014; 30(3): 303-9.
| Crossref | Google Scholar |
34 Fiscella K, Shin P. The inverse care law: implications for healthcare of vulnerable populations. J Ambul Care Manage 2005; 28(4): 304-12.
| Crossref | Google Scholar |
35 Higginbottom GM, Safipour J, Yohani S, O’Brien B, Mumtaz Z, Paton P, et al. An ethnographic investigation of the maternity healthcare experience of immigrants in rural and urban Alberta, Canada. BMC Pregnancy Childbirth 2016; 16(1): 20.
| Crossref | Google Scholar |
36 Hetherington E, Tough S, McNeil D, Bayrampour H, Metcalfe A. Vulnerable women’s perceptions of individual versus group prenatal care: results of a cross-sectional survey. Matern Child Health J 2018; 22(11): 1632-8.
| Crossref | Google Scholar |
37 Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016; 4(4): CD004667.
| Crossref | Google Scholar |
38 Andersson E, Christensson K, Hildingsson I. Parents’ experiences and perceptions of group-based antenatal care in four clinics in Sweden. Midwifery 2012; 28(4): 502-8.
| Crossref | Google Scholar |
39 Mazul MC, Salm Ward TC, Ngui EM. Anatomy of good prenatal care: perspectives of low income African-American women on barriers and facilitators to prenatal care. J Racial Ethn Health Disparities 2017; 4(1): 79-86.
| Crossref | Google Scholar |
40 McLachlan HL, Newton M, McLardie-Hore FE, McCalman P, Jackomos M, Bundle G, et al. Translating evidence into practice: implementing culturally safe continuity of midwifery care for First Nations women in three maternity services in Victoria, Australia. EClinicalMedicine 2022; 47: 101415.
| Crossref | Google Scholar |
41 Cummins A, Baird K, Melov SJ, Melhem L, Hilsabeck C, Hook M, et al. Does midwifery continuity of care make a difference to women with perinatal mental health conditions: a cohort study, from Australia. Women Birth 2023; 36: e270-e5.
| Crossref | Google Scholar |
42 Massi L, Hickey S, Maidment S-J, Roe Y, Kildea S, Nelson C, et al. Improving interagency service integration of the Australian Nurse Family Partnership Program for First Nations women and babies: a qualitative study. Int J Equity Health 2021; 20(1): 212.
| Crossref | Google Scholar |
43 Kildea S, Gao Y, Hickey S, Nelson C, Kruske S, Carson A, et al. Effect of a birthing on Country service redesign on maternal and neonatal health outcomes for First Nations Australians: a prospective, non-randomised, interventional trial. Lancet Glob Health 2021; 9(5): e651-e9.
| Crossref | Google Scholar |
44 Zhang X-H, Xu J, Chen D-Q, Guo L-F, Qiu L-Q. Effectiveness of treatment to improve pregnancy outcomes among women with syphilis in Zhejiang Province, China. Sex Transm Infect 2016; 92(7): 537.
| Crossref | Google Scholar |
45 Queensland Health. Communicable diseases control guidance: syphilis. 2020. Available at http://disease-control.health.qld.gov.au/Condition/779/syphilis#:~:text=The%20Queensland%20Syphilis%20Surveillance%20Service,of%20individuals%20affected%20by%20syphilis
46 Australasian Society for HIV Viral Hepatitis and Sexual Health Medicine (ASHM). Australian Guidelines for STI Management in Primary Care. The Australian Government Department of Health. 2022. Available at https://sti.guidelines.org.au/
47 Ong JJ, Bourne C, Dean JA, Ryder N, Cornelisse VJ, Murray S, et al. Australian sexually transmitted infection (STI) management guidelines for use in primary care 2022 update. Sex Health 2023; 20(1): 1-8.
| Crossref | Google Scholar |
48 Australian Institute of Health and Welfare. Antenatal care during COVID-19, 2020. 2021. Available at https://www.aihw.gov.au/reports/mothers-babies/antenatal-care-during-covid-19/contents/did-access-to-antenatal-care-change-during-the-covid-19-pandemic