A critical realist exploration of factors influencing engagement in diabetes prevention programs in rural settings
Britney McMullen A B * , Kerith Duncanson B C D , David Schmidt C , Clare Collins B D and Lesley MacDonald-Wicks B D
A B * , Kerith Duncanson B C D , David Schmidt C , Clare Collins B D and Lesley MacDonald-Wicks B D
A Northern New South Wales Local Health District, Lismore, NSW 2480, Australia.
B School of Health Sciences, College of Health Medicine and Wellbeing, University of Newcastle, Callaghan, NSW 2308, Australia.
C Health Education and Training Institute, NSW Health, St Leonards, NSW 2065, Australia.
D Food and Nutrition Research Program, Hunter Medical Research Institute, New Lambton Heights, NSW 2305, Australia.
Australian Journal of Primary Health 29(5) 510-519 https://doi.org/10.1071/PY22256
Submitted: 8 November 2022 Accepted: 4 April 2023 Published: 1 May 2023
Abstract
Diabetes prevention programs are intended to reduce progression to type 2 diabetes, but are underutilised. This study aimed to explore people with prediabetes’ knowledge and attitudes about prediabetes, and their perceptions about engagement in preventive programs in a rural setting. The findings will inform strategies and recommendations to increase preventive health program engagement.
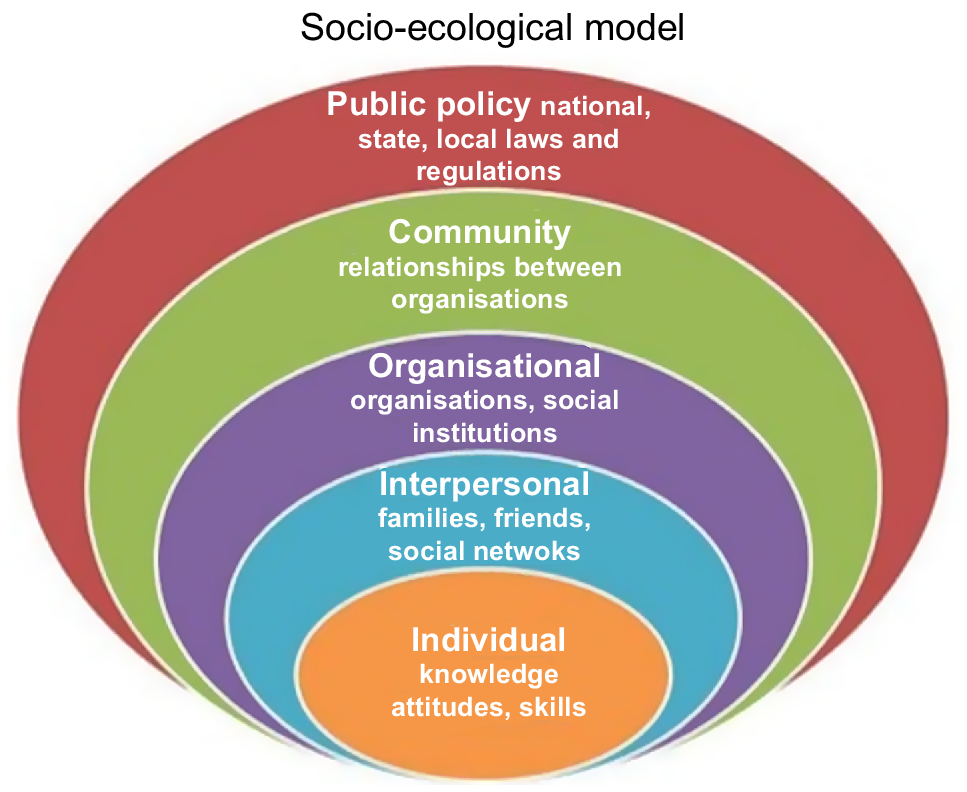
Using a qualitative approach with a critical realist methodology, semi-structured interviews were conducted with 20 rural participants with prediabetes from the Northern New South Wales Local Health District in 2021. Interviews were audio-recorded, transcribed verbatim and thematically analysed. The social-ecological model was used as a framework to interpret and action the study findings.
Factors that empowered participants and facilitated a desire to engage in preventive programs included knowledge about prediabetes, a high level of social support, trusting and supportive relationships with health professionals, and a strong desire not to progress to diabetes. Barriers to program engagement included low health literacy levels, limited support, negative experiences with health services, and social and physical constraints. The factors that influenced engagement with preventive health programs were mapped to an individual, interpersonal, organisational, community and policy level, which highlighted the complex nature of behaviour change and the influence of underlying mechanisms.
Engagement in diabetes prevention programs was dependent on individual agency factors and structural barriers, each of which related to a level of the social-ecological model. Understanding the perceptions of people with prediabetes will inform strategies to overcome multi-level barriers to preventive health program engagement in rural settings.
Keywords: barriers, critical realism, diabetes prevention, enablers, health, prediabetes, preventive programs, rural.
Introduction
A substantial proportion of the global population are at a high risk of developing type 2 diabetes mellitus (T2DM), with >352 million adults estimated to have prediabetes (Hostalek 2019). It is projected that one-quarter of people with prediabetes will develop T2DM within 5 years, and 70% will develop T2DM within their lifetime (Tabák et al. 2012). People with prediabetes have blood glucose levels that are elevated, but not high enough to be diagnosed with T2DM (Davis et al. 2018). The prevalence of prediabetes is higher in rural compared with urban populations, and 77% of people with diabetes live in low- and middle-income countries (Galaviz et al. 2018). In Australia, 6.0% of people living in rural areas have T2DM, with the prevalence being twice as high for those living in low socioeconomic areas compared with high socioeconomic areas (Australian Institute of Health and Welfare 2020).
In rural and remote Australia, 70% of adults are overweight or obese (Australian Institute of Health and Welfare 2022). Overweight or obesity are the predominant risk factors that increase the likelihood of developing prediabetes and T2DM (Australian Institute of Health and Welfare 2017). Other risk factors include physical inactivity and a family history of T2DM or cardiovascular disease (Australian Institute of Health and Welfare 2020). Globally, overweight and obesity is rapidly increasing, with >1.9 billion adults estimated to be overweight and 650 million obese (World Health Organization 2021). With the high rate of progression from prediabetes to diabetes, combined with evidence that lifestyle changes can reduce diabetes risk, diabetes prevention is an important public health issue, particularly in primary care services where considerable diabetes management occurs (Laatikainen et al. 2007).
Lifestyle interventions can play an important role in preventing diabetes onset. Randomised controlled trials have shown that T2DM can be prevented or delayed in >50% of cases through lifestyle modifications, which increase physical activity, improve diet and achieve weight loss (Miller et al. 2015). Diabetes prevention programs involving structured group or individual sessions that include education and skill development in health behaviour change are reported to reduce the risk of T2DM by 40% (Laatikainen et al. 2007). Despite evidence highlighting the effectiveness of various diabetes prevention programs, engagement in such programs is prevented by barriers at the individual, structural, organisational, health and socioeconomic level (Hawkes et al. 2020). Barriers include factors, such as patient perception of the severity of diabetes, limited knowledge of prediabetes, lack of time, comorbidities, and low income and education levels (Graziani et al. 1999; Gatewood et al. 2008; Schaefer et al. 2013; Bethancourt et al. 2014). There is a need to better understand these factors to address the complexities of preventive health program engagement.
Quantitative research has shown that rural diabetes prevention programs lead to positive health outcomes, including reduced mean weight, increased physical activity levels, and improved metabolic risk factors and psychological measures (Kilkkinen et al. 2007; Reddy et al. 2011). Challenges to implementing diabetes prevention programs within rural settings include a lack of suitable facilities, establishing credibility of primary care physicians, gaining community support, training coaches, limited resources and recruitment difficulties (Kilkkinen et al. 2007; Reddy et al. 2011).
Qualitative research examining preventive program engagement in rural areas focuses mainly on people already diagnosed with T2DM (Dunbar 2017). There is currently no published qualitative research that focuses on program engagement among people diagnosed with prediabetes in rural settings. The aim of the current study was to explore the knowledge and attitudes of people with prediabetes about their condition and their perceptions of factors that influence engagement in diabetes prevention programs in a rural setting. It is envisaged that the findings will inform the development of localised tailored strategies and recommendations to increase engagement in preventive health programs.
Methods
Setting
This study was conducted within the Northern New South Wales Local Health District (NNSWLHD), a rural area in Australia. According to HealthStats NSW, 10.6% of people in NNSWLHD have diabetes or high blood glucose (HealthStats NSW 2019). Health services available in this area for people with prediabetes include public and private organisations. The NNSWLHD is a public healthcare organisation that provides services to 290 000 people, of whom 35% are aged ≥65 years and 4.5% identify as Aboriginal or Torres Strait Islander (NSW Health 2022). The 2016 Socio-Economic Index of Disadvantage identified the Northern Rivers Region as an area of socioeconomic disadvantage (Australian Bureau of Statistics 2018). Available programs for people at high risk of developing T2DM in NNSWLHD include the ‘Get Healthy’ telephone-based coaching service; ‘Beat It’, a group lifestyle and exercise program; and ‘Reverse’, an SMS-based coaching service. These programs are free and referral can come from health professionals or self-referral. Other health services available to people with prediabetes include general practitioners and allied health professionals in primary care, and specialist services for people with comorbid conditions.
Design
This research explored the underlying causal mechanisms influencing preventive health program engagement using a critical realist methodology. Critical realism incorporates positivist and constructionist perspectives, and acknowledges that structural factors can influence an individual’s agency to affect change (Bhaskar 2014). In the context of prediabetes, factors that influence program engagement include both individual agency, such as people’s attitudes and perceptions of prediabetes, and structural mechanisms, such as healthcare settings and service delivery. Critical realism provides a framework that can be applied to health service settings to understand the complex interplay between the structural influences of the health service and the complexities experienced by health service consumers (Oladele et al. 2013). In this study, critical realism facilitated deep exploration of human factors involved in program engagement by people with prediabetes, and has the benefit of informing practice and service delivery change (Connelly 2001). This understanding will assist with building theories about why barriers and enablers to program engagement exist, and how to overcome these. A framework analysis using the social-ecological model (SEM) (Fig. 1) was conducted, which increased capacity for translation of research findings into practice (Golden et al. 2015). The SEM can be used to understand the multilevel and interrelated determinants of health behaviours (McLeroy et al. 1988). The individual level of the SEM includes characteristics, such as a person’s knowledge, attitudes, beliefs and skills. The interpersonal level focuses on relationships, including social networks and support systems. The organisational level encompasses the rules, regulations and structures that impact or influence health and wellbeing. The community level focuses on relationships between organisations, institutions and informal networks, and the policy level highlights the local, state, and national laws and policies that have a population level impact (McLeroy et al. 1988).
Socioecological model: framework for prevention, Centres for Disease Control and Prevention. Available from the Centers for Disease Control and Prevention (https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html).
Participants
A total of 20 volunteers participated in the study who self-reported having been diagnosed with prediabetes, but not T2DM. They were aged ≥18 years, living in the NNSWLHD area and were able to provide informed consent. Participants were screened via phone by the first author, and excluded if they were diagnosed with T2DM, had complex comorbidities that would limit safe participation and did not speak or understand English. No participants refused to participate or dropped out.
Sampling and recruitment
Purposive sampling was employed to ensure a defined and appropriate group of participants with prediabetes were recruited. Advertising methods for study recruitment included flyers in medical centres and chemists, social media posts, and sharing of study information by diabetes educators and dietitians from the health service. Participant information statements and consent forms were emailed to prospective participants. Based on the participant’s preference, consent was provided via a signed form or verbally prior to the interview, which was audio-recorded.
Data collection
After consent was obtained, a link to an online survey was emailed to each participant to collect sociodemographic data. Semi-structured in-depth interviews were used to gain in-depth accounts of participants’ experiences of prediabetes and perspectives about diabetes prevention programs. An interview guide was developed to provide structure while ensuring the interview process remained flexible (Supplementary file 1).
One-on-one interviews were conducted via phone by the first and second authors in the research team. The first author works within NNSWLHD and has a master’s degree. The second author has a PhD (Nutrition and Dietetics) and extensive qualitative research experience. Interviews lasted for up to 45 min with no repeat interviews conducted. Recordings were transcribed verbatim and de-identified by a professional transcription service. Participants were given the opportunity to review their transcript prior to analysis; however, all participants declined this option. Data was concurrently collected and coded by two researchers. Preliminary analysis involving discussions between all researchers commenced after 10 interviews had been conducted. No new codes were generated after 15 interviews had been coded, so data saturation was presumed to be achieved after completing 20 interviews.
Data analysis
All analyses were conducted using Microsoft Excel. Descriptive statistics were used to analyse demographic information. The interview data was inductively coded by one researcher, with a 20% subset coded by a second researcher. Each transcript was read several times to understand the data as a whole, and highlight similarities, differences and factors of interest, which were noted as comments on transcripts. Qualitative coding involved a two-stage process, with inductive coding and preliminary analysis followed by deductive framework analysis. The initial inductive component was informed by methods described by Braun and Clarke (2006). Segments of data in transcripts were highlighted, and then transferred to the Excel spreadsheet and allocated one or more codes. Each new code was added to a codebook housed in a separate Excel sheet, with a brief descriptor included for each code. This process was completed by one researcher (BM) and checked by an experienced qualitative researcher (KD). Codes, along with representative quotes, were organised into groups that contained similar or overlapping codes. The preliminary themes generated all related to individual, interpersonal, organisational, community and policy factors, which constitute the domains of the SEM. The second phase of data analysis involved mapping coded data to the SEM domains using a framework approach. One researcher (BM) conducted this analysis in an Excel table, before discussion and revision of the table following input from other research team members. This deductive analysis facilitated the development of an actionable framework for health service implementation.
Rigour
Specific intentional strategies were used to ensure study quality, reliability, validity and credibility. It is important to acknowledge the research team have conducted and written this research from the position of health care providers. The research team includes researchers with preventive health expertise and extensive dietetic research experience. Co-researchers and peer mentors reviewed and commented on the transcribed data, providing ideas to consider and suggestions about potential themes. Throughout the analysis process, the second author independently coded a subset of the transcripts, and then discussed any differing perspectives and interpretations with the first author as a means of investigator triangulation. The principal researcher kept a reflexive journal, particularly while conducting interviews and reading transcripts for the first time. This process led to discussions between co-authors that were intended to increase awareness and sincerely reflect on personal factors that may have influenced the research process and researcher approaches.
Findings and discussion
The study sample were predominantly female (13/20), white (17/20) and aged > years (16/20), with a similar distribution of employed and unemployed (Table 1). All participants reported to have been diagnosed with prediabetes by a doctor using blood test results. The themes and subthemes mapped against the SEM domains are shown in Table 2 and Supplementary Table S1.
| Participant characteristic | Category | Number (percentage) | Participant characteristic | Category | Number (percentage) | |
|---|---|---|---|---|---|---|
| Age (years) | 25–34 | 2 (10) | Level of education | Did not graduate high school | 1 (5) | |
| 35–44 | 2 (10) | High school graduate | 7 (35) | |||
| 45–54 | 6 (30) | Vocational/trade/TAFE | 7 (35) | |||
| 55–64 | 5 (25) | University degree | 5 (25) | |||
| 65–74 | 1 (5) | |||||
| 75+ | 4 (20) | |||||
| Sex | Female | 13 (65) | Marital status | Single | 4 (20) | |
| Male | 7 (35) | Married/de Facto | 9 (45) | |||
| Divorced/separated/widowed | 7 (35) | |||||
| Ethnicity | Aboriginal | 1 (5) | Level of income | <$40 000 | 9 (45) | |
| Asian | 1 (5) | $40 000–$60 000 | 4 (20) | |||
| Caucasian | 17 (85) | $60 000–$80 000 | 5 (25) | |||
| Native American | 1 (5) | >$80 000 | 1 (5) | |||
| Employment status | Employed | 9 (45) | ||||
| Unemployed | 11 (55) |
| Preliminary themes: factors influencing engagement | Critical realism mechanisms | Social-ecological model domain and description | Representative quote from participants | |
|---|---|---|---|---|
| Diagnosis | Active role in health care journey | Individual (individual knowledge, attitudes, behaviours and skills) | ‘I looked at my family history and my uncle has diabetes and my mother has diabetes. But they are both normal height and normal weight so I just thought it’s really the gene pool.’ (P5) | |
| Health literacy levels | ||||
| Attitudes and beliefs | ||||
| Socioeconomic status | ||||
| Social support | Power imbalances between clinicians and patients | Interpersonal (Interactions with others including social networks and support systems) | ‘I’m not supported, because it’s really hard to get in to see your GP. The GPs are young and fit. It’s really hard for them to understand how hard it is.’ (P4) | |
| Experience with health services | ||||
| Patient-clinician relationship | ||||
| Health service approach | Person-centred care | Organisational (rules, regulations and structures that impact or influence health and wellbeing) | ‘No one’s really said ‘Hey, won’t you do A, B and C to try to stop this.’ (P1) | |
| Cost | Overburdened health system | Community (relationships between organisations, institutions and informal networks) | ‘Use social media, because that’s where we all are, and promoting programs on different local group pages, because that’s where I find a lot of my information.’ (P10) | |
| Distance | ||||
| Availability | ||||
| Access | ||||
| Promotion | ||||
| Transportation | ||||
| Program development and implementation | Funding for prevention | Policy (local, state, and national laws and policies) | ‘It would be great to participate in a diabetes prevention program. To be in some sort of organised group to make me get off the couch and not just rely on self-motivation.’ (P5) |
Individual factors
Most participants were shocked to learn they had prediabetes. They reported being asymptomatic and were visiting the doctor for a general health check when they were diagnosed:
I was shocked, because I had absolutely no symptoms at the time, and I just ate and drank normally. (Participant 9; aged 55–64 years; male)
Almost all participants believed that their prediabetes diagnosis was predominantly hereditary and they would eventually be diagnosed with diabetes:
My mother had diabetes as did her sister … Bad genes. I mean others around me can eat all the stuff that I can’t eat and it doesn’t affect them, but that’s because I’ve got the lousy genes. (Participant 8; aged ≥75 years; female)
Participants discussed their fear around developing T2DM. They were aware of the negative impacts of diabetes, including the need to take medications and injections, and were worried about quality of life, all of which were strong motivators to make lifestyle changes:
The fact that they have to either take medication or inject themselves … I know it affects eyesight and circulation, and toes get cut off. (Participant 8; aged ≥75 years; female)
Similar to other studies (Abbott et al. 2012), feelings of shock and fear motivated participants to play an active role in making lifestyle changes. This highlights the importance of diagnosis, which presents an opportunity for health professionals to provide patients with information and support while motivation levels are high (Thankappan et al. 2018).
Participants displayed varying levels of understanding about prediabetes and lifestyle changes. Despite participants’ awareness of the hereditary nature of T2DM, most participants understood that lifestyle changes can prevent onset. Some participants described feeling confused and unsure about which lifestyle changes to make and how to make them. An understanding of prediabetes and lifestyle changes can act as an enabling structure, encouraging those with the ability to make lifestyle changes to take action:
I suppose that it’s the opportunity to turn it around … I changed my lifestyle and changed what I’m doing, because I don’t want to become a diabetic. (Participant 5; aged 55–64 years; female)
From the literature, we know that health literacy levels can be an inhibitor to making lifestyle changes. Previous research identified that low health literacy is common in people with prediabetes, and can impact their ability to understand information, use services and make informed health decisions (Luo et al. 2020).
Interpersonal factors
The dominant interpersonal theme conveyed was the need for strong social support, particularly from family, friends and health professionals. Participants perceived social support as a motivator to make changes:
I’ve got a girlfriend and we had a goal to do the Three Capes walk down in Tasmania, that’s a 4-day trek. So we worked up to that for 6 months and did that. (Participant 5; aged 55–64 years; female)
From a critical realist perspective, there was a reliance on individual agency when it came to making lifestyle changes. It was evident that those without support found it overwhelming and difficult to make changes:
I managed to stave it off until recently over the last couple of years. Well, it’s only me; I don’t have a family, I’m on my own, so everything’s up to me. (Participant 2; aged 45–54 years; female)
Participants found it difficult to know what to do next if they had limited support and encouragement from health professionals, particularly at diagnosis:
When I got diagnosed … I could have been given pamphlets “You’ve been diagnosed. Here are your options”. Really explaining the condition to people, so that they know what they’ve got, or what they could get. More support in the beginning. (Participant 2; aged 45–54 years; female)
Studies have shown that motivation to make lifestyle changes was increased through participation in a peer support program (Thankappan et al. 2018). The Kerala Diabetes Prevention Program was a peer-support lifestyle intervention whereby people diagnosed with prediabetes were assisted by peers to make lifestyle changes (Thankappan et al. 2018). The use of peer leaders to support behaviour change led to positive health and wellbeing outcomes (Thankappan et al. 2018). This highlighted the importance of supportive structures, which can influence our motivation to make healthy decisions (Abbott et al. 2012). Consistent with the literature, participants who received support described feeling empowered and motivated to make lifestyle changes, whereas limited support was a notable barrier (Begum et al. 2022).
Engagement with health professionals was cited as either a barrier or enabler, depending on the experience. Participants who experienced a positive encounter with a health professional articulated feeling supported and encouraged:
The doctor up here was really encouraging and proactive, and wasn’t so demeaning as previous experiences, where I’ve basically just been told, “It’s your fault. You’re overweight. You’ve got to do something about it, serves you right”. (Participant 4; aged 45–54 years; female)
Participants who had a negative experience with health professionals felt disheartened and demotivated to make lifestyle changes. This was often the result of a health professional not adopting a person-centred approach:
He just told me, “Go to a dietitian”, and I went to a dietitian … She just said, “Cut this out, cut that out”, which meant nearly everything that I would eat. I was disheartened with her. I lost faith with her … She didn’t give me alternatives. (Participant 6; aged 45–54 years; female)
From a critical realist perspective, there was an evident power imbalance between participants and health professionals, whereby participants felt that health professionals provided limited information, guidance and support. Participants who received limited support from health professionals described feeling confused, demotivated and found it difficult to trust the health professional. Health professionals who provided support and guidance, and actively involved patients in decision-making are highly valued by patients (Evans et al. 2007). Furthermore, according to Penn et al. (2013), patients who experienced a positive patient–clinician relationship were more likely to engage in preventive behaviours.
Organisational factors
A lack of specific resources and management led to participants feeling that the health service was waiting for them to develop T2DM. Most participants could not recall being offered services or support, because they had not yet developed T2DM:
Nothing. I think the medical world was just streamlining me into the diabetic clinic and waiting for me to become a diabetic, so that I could go on the medication. (Participant 1; aged 55–64 years; female)
Although some participants were referred to an allied health professional for follow-up care using a care plan, most participants explained they had not been referred to any available services, such as a prevention program or allied health professional. This highlighted the nature of the health service, which largely aims to treat diseases rather than prevent them:
I haven’t had any other discussions with any other doctors regarding that diagnosis or any treatment otherwise. I wasn’t given anything. Then, he just explained to me that I had to be aware of it and to keep that in mind. (Participant 7; aged 35–44 years; female)
With limited referrals being made by health professionals, participants lacked awareness of preventive programs:
No, I haven’t been referred to anything like that before. I’ve never heard of Get Healthy either. (Participant 19; aged 45–54 years; female)
At the organisational level, participants experienced differing levels of concern from health professionals. Some participants described receiving a diagnosis from their general practitioner, whereas others felt that prediabetes was overlooked by their general practitioner and was only diagnosed due to seeing a specialist:
Both times the GP said, “Looks great, nothing to worry about. Then I started seeing a respiratory specialist who referred me onto an endocrinologist … She reviewed all of my past blood work and said, “Actually, you’re prediabetes. She said she sees it a lot that the GPs are underdiagnosing prediabetes and they sort of wait till it becomes a type 2 diabetes level on the blood tests before anything happens. (Participant 20; aged 25–34 years; female)
The variability in health service approaches to prediabetes management may be influenced by their level of adoption of a person-centred approach. Person-centred care is high-quality healthcare that considers individual needs and sees patients actively involved in decision-making (Mirzaei et al. 2013). Some participants reported encounters with the health service lacked a person-centred approach. This was evident at diagnosis, whereby some participants experienced inaction and a lack of concern from their general practitioner, and felt that their diagnosis was not viewed as serious. These findings are consistent with those from a previous study whereby 20 participants were interviewed in Australia, and described their diagnosis as vague and unclear (Somerville et al. 2020). Other studies have identified that when a person-centred approach was adopted, the patient felt supported and motivated to make lifestyle changes (Jo Delaney 2018; Somerville et al. 2019) This highlights the importance of a person-centred care framework, which ensures the patients’ individual needs are met, and they are actively involved in and supported to make informed decisions regardless of whether their prediabetes needs are managed individually, in a group or in a program.
Community factors
From a critical realist perspective, there were a number of inhibiting structures that stemmed from living in a rural setting that made lifestyle changes difficult. With NNSWLHD being identified as an area of socioeconomic disadvantage, the cost of transportation; healthy food; appointments with health professionals, such as dietitians; and sign-up fees, such as gym memberships, were consistently reported by participants. Other inhibiting structures included living with comorbidities, limited transportation options and time constraints. Participants described the difficulty of living in rural areas and not having access to transportation, which limited their ability to access health services:
I’m a bit out of town. There’s none [public transport] on the weekend, and school holidays there’s hardly any. So even though it’s only 30 minutes by car, it’s not like that for a lot of pensioners out here, lower income people. So distance is very much a barrier. (Participant 14; aged ≥75 years; male)
Cost was a prominent factor among participants that reduced their ability and desire to access health services. Participants described the financial constraints that came with specialist appointments, transportation, and accessing health and exercise facilities:
I’m on a disability pension, so I can’t afford to go to the poo.ven going to the specialist, which costs me a lot of money to go to Lismore, Ballina and even to take my car on the road. (Participant 2; aged 45–54 years; female)
Another common barrier among participants was a perceived lack of time. Between working long hours, and taking care of children and elderly parents, many participants felt they did not have enough time or were too exhausted to exercise:
In my age group, unfortunately, we’re all still working, we’ve got, a lot of us have got parents that we’re looking after, we’ve still got young adult children, grandchildren; life is really pulling us in all directions. (Participant 4; aged 45–54 years; female)
Participants described experiencing a range of comorbidities that inhibited their ability to be physically active:
It’s hard, because I have psoriatic osteoarthritis. The only form of exercise I can do is probably in the pool at the moment. For me, it’s finding the energy now, and breaking through the pain, because I’ve got a lot of pain. (Participant 2; aged 45–54 years; female)
Similar to other studies, there were numerous physical and social factors at the community level that influenced participants’ ability to engage in preventive programs (Shawley-Brzoska and Misra 2018). The health system is a contributing factor to social barriers, which is evident with high health care costs, a lack of funding and resources for preventive services in the community, and limited transportation options in rural settings, which makes accessing health services challenging (Katangwe et al. 2020). To overcome such barriers, successful programs have enabled engagement through a range of strategies, including free participation, program referrals made by general practitioners, incentives, group settings both online and face-to-face, convenient program times and locations, and culturally appropriate and individually tailored activities (Delgadillo et al. 2010). People with prediabetes who experience inhibiting structures are less likely to engage in preventive programs.
Policy factors
The availability of, and access to, individual or group lifestyle programs suitable for people diagnosed with prediabetes is highly variable. After identifying social and physical barriers to engaging in a preventive program, participants offered a range of suggestions that would enable them to access and attend preventive programs. A structural design solution to address limitations in agency suggested by participants was program flexibility in location, timing and mode of delivery:
Having three or four different meetings over the week that you can choose to go to, because some of us work part-time, some work full-time, and then you’ve got shift workers, and so 5:00pm after work you can’t do. (Participant 11; aged 25–34 years; female)
Participants also emphasised the importance of free programs to reduce the cost barrier:
No reasons that I wouldn’t want to participate. Except the cost, of course. At the moment it’s just money that’s restricting me. (Participant 2; aged 45–54 years; female)
Some participants expressed that an incentive would be an effective motivator to participate:
If people think they’re getting a present or prize at the end of it, well, they’ll come. (Participant 12; aged ≥75 years; male)
Although some participants expressed feeling comfortable using technology and signing up to programs online, others felt that assistance with program enrolment was needed:
If the doctors can enrol you, that’s great, or if somebody can call you when you’re at home and you can organise it through that. (Participant 11; aged 25–34 years; female)
Participants described a range of strategies that would ensure programs meet their individual needs and barriers are reduced. Consistent with findings from other studies, programs need to be flexible to work around busy schedules, free to overcome financial barriers, and offer both face-to-face and online components, so people can choose their preferred setting (Delgadillo et al. 2010).
Strengths and limitations
This qualitative study involved 20 adults living in one rural health district, which may limit the generalisability of findings. However, preliminary analysis after 10 interviews had been conducted, and continuing interviews until no new data were obtained contributed to this study’s rigour. Factors that may influence access to programs, such as rurality and sex, were not explored in detail, and it is recommended that these be considered in future studies or program planning. The qualitative design provided in-depth information that can inform lifestyle change components of prediabetes prevention programs. Using a critical realist approach allowed exploration of the underlying issues for prediabetes care delivery. Research using maximum deviation sampling techniques could further explore the needs of more diverse samples of people with prediabetes.
Implications
Behaviour change is more likely to occur if health professionals have positive relationships with patients and recommend changes that are appropriate for the patient.
By pre-emptively considering barriers to engagement, diabetes prevention programs can be designed to meet the needs of rural community members. Program design should consider cost and accessibility barriers, a person-centred approach, flexibility, and support.
There is a need for rural health professionals to provide education and resources with a health literacy focus, and disseminate these at diagnosis to improve health literacy levels and understanding of the condition.
To complement insights of people with prediabetes, research examining the perspectives of rural health professionals and their role in preventive program engagement is needed. Interviews should be conducted with health professionals to investigate prediabetes diagnosis and management within the health service.
Conclusion
This study provides new insights into perceptions of people with prediabetes and the complexity of preventive program engagement across all social-ecological levels. The aim was to explore the knowledge and attitudes of people with prediabetes about the condition, and their perceptions about factors that influence engagement in diabetes prevention programs. This qualitative study identified that there are a range of inhibiting structures that influence program engagement. Barriers that challenged participants’ willingness and ability to engage in a program included a limited understanding of prediabetes and confusion at diagnosis, limited support, and physical and social constraints. The key enablers of program engagement were motivation to prevent diabetes, respectful and supportive patient-clinician relationships, and a positive experience with the health service. Understanding factors that influence program engagement and how they align with the SEM provides a pathway to improve program design and management, and guides the development of localised strategies to increase program engagement.
Acknowledgements
The Health Education and Training Institute provided funding for 60 days of clinical backfill through the Rural Research Capacity Building Program. The Northern NSW Local Health District provided the primary researcher with guidance and support.
References
Abbott PA, Davison JE, Moore LF, Rubinstein R (2012) Effective nutrition education for Aboriginal Australians: lessons from a diabetes cooking course. Journal of Nutrition Education and Behavior 44, 55-59.
| Crossref | Google Scholar |
Australian Bureau of Statistics (2018) Socio-economic indexes for areas (SEIFA) 2016 [Online]. Available at https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/2033.0.55.001Main+Features12016?OpenDocument [Accessed 26 January 2023]
Australian Institute of Health and Welfare (2017) Risk factors to health [Online]. Available at https://www.aihw.gov.au/reports/risk-factors/risk-factors-to-health [Accessed 26 January 2023]
Begum S, Povey R, Ellis N, Gidlow C, Chadwick P (2022) Influences of decisions to attend a national diabetes prevention programme from people living in a socioeconomically deprived area. Diabetic Medicine 39, e14804.
| Crossref | Google Scholar |
Bethancourt HJ, Rosenberg DE, Beatty T, Arterburn DE (2014) Barriers to and facilitators of physical activity program use among older adults. Clinical Medicine & Research 12, 10-20.
| Crossref | Google Scholar |
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3, 77-101.
| Crossref | Google Scholar |
Connelly J (2001) Critical realism and health promotion: effective practice needs an effective theory. Health Education Research 16(2), 115-119.
| Crossref | Google Scholar |
Davis WA, Peters KE, Makepeace A, Griffiths S, Bundell C, Grant SFA, Ellard S, Hattersley AT, Paul Chubb SA, Bruce DG, Davis TME (2018) Prevalence of diabetes in Australia: insights from the Fremantle Diabetes Study Phase II. Internal Medicine Journal 48, 803-809.
| Crossref | Google Scholar |
Delgadillo AT, Grossman M, Santoyo-Olsson J, Gallegos-Jackson E, Kanaya AM, Stewart AL (2010) Description of an academic community partnership lifestyle program for lower income minority adults at risk for diabetes. The Diabetes Educator 36, 640-650.
| Crossref | Google Scholar |
Dunbar JA (2017) Diabetes prevention in Australia: 10 years results and experience. Diabetes & Metabolism Journal 41, 160-167.
| Crossref | Google Scholar |
Evans PH, Greaves C, Winder R, Fearn-Smith J, Campbell JL (2007) Development of an educational ‘toolkit’ for health professionals and their patients with prediabetes: the WAKEUP study (Ways of Addressing Knowledge Education and Understanding in Pre-diabetes). Diabetic Medicine 24, 770-777.
| Crossref | Google Scholar |
Galaviz KI, Narayan KMV, Lobelo F, Weber MB (2018) Lifestyle and the prevention of type 2 diabetes: a status report. American Journal of Lifestyle Medicine 12, 4-20.
| Crossref | Google Scholar |
Gatewood JG, Litchfield RE, Ryan SJ, Geadelmann JDM, Pendergast JF, Ullom KK (2008) Perceived barriers to community-based health promotion program participation. American Journal of Health Behavior 32, 260-271.
| Crossref | Google Scholar |
Graziani C, Rosenthal MP, Diamond JJ (1999) Diabetes education program use and patient-perceived barriers to attendance. Family Medicine 31, 358-363.
| Google Scholar |
Hawkes RE, Cameron E, Cotterill S, Bower P, French DP (2020) The NHS Diabetes Prevention Programme: an observational study of service delivery and patient experience. BMC Health Services Research 20, 1098.
| Crossref | Google Scholar |
HealthStats NSW (2019) Diabetes prevalence in adults [Online]. Available at http://www.healthstats.doh.health.nsw.gov.au/Indicator/dia_prev_age/dia_prev_lhn [Accessed 26 January 2023]
Hostalek U (2019) Global epidemiology of prediabetes – present and future perspectives. Clinical Diabetes and Endocrinology 5, 1-5.
| Crossref | Google Scholar |
Jo Delaney L (2008) Patient-centred care as an approach to improving health care in Australia. Collegian 25, 119-123.
| Crossref | Google Scholar |
Katangwe T, Family H, Sokhi J, Kirkdale CL, Twigg MJ (2020) The community pharmacy setting for diabetes prevention: a mixed methods study in people with ‘pre-diabetes’. Research in Social and Administrative Pharmacy 16, 1067-1080.
| Crossref | Google Scholar |
Kilkkinen A, Heistaro S, Laatikainen T, Janus E, Chapman A, Absetz P, Dunbar J (2007) Prevention of type 2 diabetes in a primary health care setting. Interim results from the Greater Green Triangle (GGT) Diabetes Prevention Project. Diabetes Research and Clinical Practice 76, 460-462.
| Crossref | Google Scholar |
Laatikainen T, Dunbar JA, Chapman A, Kilkkinen A, Vartiainen E, Heistaro S, Philpot B, Absetz P, Bunker S, O’Neil A, Reddy P, Best JD, Janus ED (2007) Prevention of type 2 diabetes by lifestyle intervention in an Australian primary health care setting: Greater Green Triangle (GGT) Diabetes Prevention Project. BMC Public Health 7, 249.
| Crossref | Google Scholar |
Luo H, Chen Z, Bell R, Rafferty AP, Gaskins Little NR, Winterbauer N (2020) Health literacy and health behaviors among adults with prediabetes, 2016 behavioral risk factor surveillance system. Public Health Reports 135, 492-500.
| Crossref | Google Scholar |
McLeroy KR, Bibeau D, Steckler A, Glanz K (1988) An ecological perspective on health promotion programs. Health Education Quarterly 15, 351-377.
| Crossref | Google Scholar |
Miller CK, Weinhold KR, Marrero DG, Nagaraja HN, Focht BC (2015) A translational worksite diabetes prevention trial improves psychosocial status, dietary intake, and step counts among employees with prediabetes: a randomized controlled trial. Preventive Medicine Reports 2, 118-126.
| Crossref | Google Scholar |
Mirzaei M, Aspin C, Essue B, Jeon Y-H, Dugdale P, Usherwood T, Leeder S (2013) A patient-centred approach to health service delivery: improving health outcomes for people with chronic illness. BMC Health Services Research 13, 251.
| Crossref | Google Scholar |
NSW Health (2022) Northern NSW – local health districts [Online]. Available at https://www.health.nsw.gov.au/lhd/Pages/nnswlhd.aspx [Accessed 26 January 2023]
Oladele D, Clark AM, Richter S, Laing L (2013) Critical realism: a practical ontology to explain the complexities of smoking and tobacco control in different resource settings. Global Health Action 6, 19303.
| Crossref | Google Scholar |
Penn L, Ryan V, White M (2013) Feasibility, acceptability and outcomes at a 12-month follow-up of a novel community-based intervention to prevent type 2 diabetes in adults at high risk: mixed methods pilot study. BMJ Open 3, e003585.
| Crossref | Google Scholar |
Reddy P, Hernan AL, Vanderwood KK, Arave D, Niebylski ML, Harwell TS, Dunbar JA (2011) Implementation of diabetes prevention programs in rural areas: Montana and south-eastern Australia compared. Australian Journal of Rural Health 19, 125-134.
| Crossref | Google Scholar |
Schaefer I, Kuever C, Wiese B, Pawels M, van den Bussche H, Kaduszkiewicz H (2013) Identifying groups of nonparticipants in type 2 diabetes mellitus education. The American Journal of Managed Care 19, 499-506.
| Google Scholar |
Shawley-Brzoska S, Misra R (2018) Perceived benefits and barriers of a community-based diabetes prevention and management program. Journal of Clinical Medicine 7, 58.
| Crossref | Google Scholar |
Somerville M, Ball L, Sierra-Silvestre E, Williams LT (2019) Understanding the knowledge, attitudes and practices of providing and receiving nutrition care for prediabetes: an integrative review. Australian Journal of Primary Health 25, 289-302.
| Crossref | Google Scholar |
Somerville M, Burch E, Ball L, Williams LT (2020) ‘I could have made those changes years earlier’: experiences and characteristics associated with receiving a prediabetes diagnosis among individuals recently diagnosed with type 2 diabetes. Family Practice 37, 382-389.
| Crossref | Google Scholar |
Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M (2012) Prediabetes: a high-risk state for diabetes development. The Lancet 379, 2279-2290.
| Crossref | Google Scholar |
Thankappan KR, Sathish T, Tapp RJ, Shaw JE, Lotfaliany M, Wolfe R, Absetz P, Mathews E, Aziz Z, Williams ED, Fisher EB, Zimmet PZ, Mahal A, Balachandran S, D’Esposito F, Sajeev P, Thomas E, Oldenburg B, Gregg E (2018) A peer-support lifestyle intervention for preventing type 2 diabetes in India: a cluster-randomized controlled trial of the Kerala Diabetes Prevention Program. PLoS Medicine 15, e1002575.
| Crossref | Google Scholar |
World Health Organization (2021) Obesity and overweight [Online]. Available at https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Accessed 26 January 2023]


