Enhancing global health communication during a crisis: lessons from the COVID-19 pandemic
Scott Ratzan A B * , Silvia Sommariva C and Lauren Rauh AA
B
C
Abstract
Background/objective:The understanding and practice of public health crisis communication are improved through the study of responses to past crises, but require retooling for present challenges. The ‘Addressing Ebola and other outbreaks’ checklist contains guiding principles built upon maxims developed from a World Health Organization consultation in response to the mad cow (bovine spongiform encephalopathy) crisis that were later adopted for Ebola. The purpose of this article is to adapt the checklist for the health communication challenges and public health practices that have emerged during the coronavirus disease 2019 (COVID-19) pandemic. The communication challenges of promoting vaccine acceptance are used to illustrate a key area that requires strengthened communication. Type of program or service: Effective communication principles for application during the COVID-19 pandemic. Results: The COVID-19 pandemic has introduced unique challenges for public health practitioners and health communicators that warrant an expansion of existing health communication principles to take into consideration: the new infodemic (or mis/disinfodemic) challenge – particularly as treatments and vaccines are being developed; communication of risk and uncertainty; health-information behaviours and the instantaneous nature of social media, and the relationship between media literacy and health literacy; the effects of the pandemic on other health issues; and the need for a flexible communication strategy that adapts to the different stages of the pandemic. Lessons learnt: Principles discussed in this article will help build preparedness capacity and offer communication strategies for moving from the acute phase to the ‘next normal’ with likely prevention (e.g. herd immunity achieved through vaccination) and societal COVID-19 resilience.Background
On 30 January 2020, the World Health Organization (WHO) declared the outbreak of coronavirus disease 2019 (COVID-19) a Public Health Emergency of International Concern.1 Since then, in a 24-hour media environment, the topic has been covered without interruption and in real-time. The rapid escalation of the disease has been accompanied by confusing, and often contradictory communication messages.2 Questions contributing to the ‘communication chaos’ relating to COVID-19 range from individual prevention measures (e.g. effectiveness of masks in containing contagion3) and treatment availability (e.g. reports on hydroxychloroquine4).
In an interview with the New Yorker in April 2020, Dr. Francis Riedo, a Seattle-based infectious-disease specialist, acknowledged “a pandemic is a communication emergency as much as a medical crisis”.5 The experiences of countries like South Korea and Singapore corroborate this analysis, where aggressive testing, tracking and containment policies were boosted by timely communication from central authorities. These countries built a robust infrastructure for crisis communication in the wake of the severe acute respiratory syndrome (SARS) outbreak in 2002–2004 and the H1N1 pandemic in 2009, and were able to launch into the same playbook for COVID-19.6-9
The COVID-19 pandemic has introduced unique challenges for health communicators. One of these challenges is the increasing amount of false content circulating on social media platforms. Even though some of this information is spread without malicious intent, the language, sentiments and tactics are similar to that observed from antivaccination proponents (e.g. emotionally charged false narratives of vaccine side effects), conspiracy theorists (e.g. COVID-19 was started in a Chinese laboratory) or climate change deniers (e.g. COVID-19 is a hoax). No aspect of the COVID-19 pandemic – from origin, to symptoms, to prevention – has been left untouched. Particularly concerning is the spread of misinformation relating to a potential vaccine for the disease, even well before a vaccine is available for public use. Rumours of safety scares and conspiracies relating to a COVID-19 vaccine have swirled throughout social media, leading to social media outlets taking active measures to limit misinformation.10,11 These measures, although important, have not prevented a saturated information system nor blocked harmful misinformation from undermining science-backed sources. Similarly, WHO has boosted its own efforts to address a “second ‘disease’” that is spreading parallel to the virus, one of an infodemic – when excessive amounts of information become detrimental to addressing a certain issue.12
These features of the media environment and the way people engage with the news call for a revision of the risk communication guidance during a public health crisis. This article adapts key principles of health communication in light of the challenges that have emerged during the COVID-19 pandemic and offers points for consideration. Two previous works written for the 2014 Ebola crisis and the transmissible spongiform encephalopathies (nvCJD or mad cow disease) outbreak in the mid-1990s act as a framework.13,14 We also report and reflect on recent findings from our CUNY COVID-19 Tracking Survey15, which assesses how people in New York State are responding to the pandemic, including their attitudes towards a potential vaccine – a key area that calls for strengthened communication. The phone, online and mobile SMS-to-online survey involves a representative sample of 1000 adults in both New York City and a sample of 1000 for the entire state, surveyed at regular intervals over 16 weeks from 13 March 2020.
The perspectives offered in this paper reflect challenges presented –y the communication environment in the US in particular, with the acknowledgement that many platforms have international reach and the checklist will also have relevance elsewhere.
Considerations regarding communication during the COVID-19 pandemic
Three general areas of capacity building for health communication emerge from the ongoing pandemic: the need for communicators to be proactive and to take preventive actions at times; the importance of–planning ahead while also acknowledging the unpredictability of the situation; and the call to focus on people.
1) Be proactive
Compete for attention
Health communicators may need to compete for attention of their audience while they position their messages in the context of a diverse media environment. In the case of the COVID-19 pandemic, this challenge has reached an unprecedented level due to the high volume of information being circulated both by media outlets and private citizens.16 Furthermore, the loudest voices in the room may in fact be perpetrators of false information, which is often the case with anti-vaccination disinformation.
Health communicators need to proactively seek ways to be louder by speaking to those most vulnerable to misinformation with the information most meaningful to them. In our COVID-19 Tracking Survey conducted in late May 2020, 66% of respondents reported that the side effects of a potential COVID-19 vaccine were worrisome for them.15 This vulnerability to mis/disinformation about vaccine safety is both an important target and argument for proactive health communications to stand out.
In an earlier Tracking Survey conducted in late March, 62% of respondents said they would accept a COVID-19 vaccine, 19% said they would decline it and 19% were unsure.17 These results indicate that not enough people would be willing to be vaccinated to achieve herd immunity against COVID-19 in New York City. These findings show that governments and public health sectors worldwide need to deeply understand emerging public attitudes to COVID-19 vaccination, and plan and act now, well before a vaccine is available.
Establish trusted leadership
Having a clear voice within government helps avoid a ‘talking heads’ dynamic that undermines the development of a cohesive strategy. WHO communicated the “lowest common denominator” early on with a commitment to member states’ sovereignty for policy actions.18 In the US, director of the National Institute of Allergy and Infectious Diseases Dr. Anthony Fauci became a leading voice without a clearly defined inter-agency task force and with a seemingly absent Centers for Disease Control and Prevention. This shows that the news media and the public self-select key leadership figures if left devoid of one.
In contrast, countries that have established strong responses early with one firm voice as the source for accurate and clear information, have had less severe outcomes. German Chancellor Angela Merkel and Taiwan President Tsai Ing-wen have continuously stood as examples of the influence of trusted leadership on the containment, spread and severity of the COVID-19 pandemic within their respective countries. Similarly, in Australia, following a muddled response to the bushfire crisis that tore through the country in early 2020, Prime Minister Scott Morrison has taken a firm science-based approached to confronting COVID-19. Medical experts were placed early at the centre of the response and Mr Morrison has been cited as placing unity and even-handedness before partisan decision making.19
Findings from the CUNY tracking survey highlight the importance of establishing trust between governments and the public, with respondents indicating that they had grown extremely suspicious of the COVID-19 situation. Almost two-thirds (65%) of respondents believed that the statement: “the spread of the COVID-19 pandemic or the response to it are influenced by the private influence of powerful but hidden groups” is definitely or probably true. Government and public health leaders will face challenges in persuading the public to accept a potential COVID-19 vaccine when or if it becomes available.
Fight false information
Although the infodemic includes both accurate and inaccurate content, it is the false content that has the potential to severely harm the public. In March 2020, hundreds of Iranian citizens died after ingesting alcohol in a bid to treat COVID-19 as a result of misinformation circulating on social media.20 Actors spreading misinformation or disinformation provide content that fills data voids and addresses urgent concerns that the public expresses. As a result, health communicators are called to revise their strategies to respond to inaccuracies that are already circulating, while also picking up on early signals of rumours and prevent them from spreading further. For example, during the COVID-19 pandemic, WHO has launched an initiative called ‘Myth busters’, where the organisation directly addresses misconceptions and fake information.21
2) Plan ahead (but acknowledge the uncertainty)
Consider growing scientific evidence
Since January 2020, evidence relating to COVID-19 and its spread has evolved rapidly. In the case of COVID-19, uncertainty due to a rapidly changing context has been compounded by the scarce knowledge the scientific community had of this particular virus. The increasing number of articles published before undergoing traditional peer-review processes has also been problematic. In some instances, media outlets have not interpreted findings from these papers with caution and reported on them as if they were widely accepted knowledge.22
When uncertainties are not acknowledged clearly, benign, or unfortunately even detrimental recommendations, for instance related to treatments, can find their way into the news stream. This has been the case particularly with hydroxychloroquine in which early and largely unsubstantiated findings led to an overhyped promise of the drug’s effects on reducing the severity of COVID-19 symptoms and was met again with unsubstantiated questioning of the drug’s safety.23 The result of this ‘back and forth’ creates confusing public-facing messaging and undermines trust in scientific evidence. This urgency for more information on COVID-19 creates a dangerous environment in which the wrong information can spread rapidly while people seek answers. In our COVID-19 Tracking Survey, 75% of those unwilling to take a COVID-19 vaccine claimed they wished to wait to find out whether or not it is effective.15 Imagine if every week a new study was published claiming effectiveness only to be debunked the following week. This would have a disastrous effect on vaccine uptake.
3) Focus on people
Health literacy is (also) media literacy
Given the role of social media users in creating and disseminating information, it is crucial to engage them in positive health information seeking and sharing behaviours. In the age of social media (with each platform being distinct in patrons and content), the definition of health literacy23 is expanded to make sure that users know how to navigate online platforms in order to access and accurately judge the information they see.24 To this end, interventions that boost media literacy and teach emotional skepticism25 can help users distinguish between accurate and inaccurate content and, thus, have the potential to reduce the pollution of the media ecosystem.
Checklist for global health communication strategies in response to COVID-19
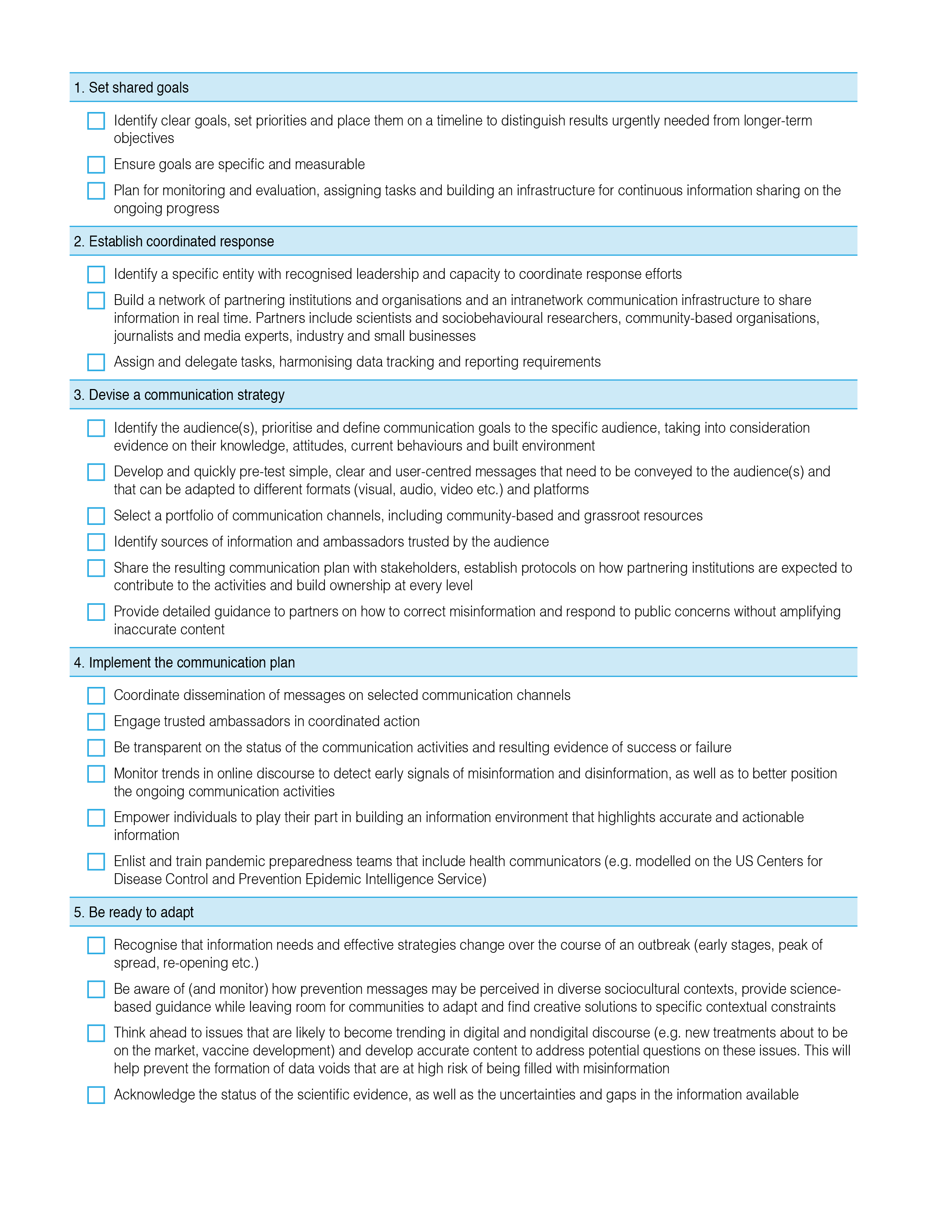
In light of the health communication challenges and practices that have emerged during the COVID-19 pandemic, we propose the following principles for effective global health communication practices (Figure 1).
Conclusion
The COVID-19 crisis has been the first pandemic to be almost ‘livestreamed’ on social media and digital platforms. Drawing on the lessons learnt from this situation and contextualising the new media environment that health communicators are called to operate in, the checklist presented in this paper is intended to be used as a tool for preparation as well as a tool for implementation of communication strategies to move from the acute phase of the pandemic to the ‘next normal’. It is critical that health communicators worldwide are more proactive in tackling risk communication challenges related to COVID-19, with likely prevention achieved through vaccination and societal COVID-19 resilience.
References
1 World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) Geneva, Switzerland: WHO; 2020 [cited 2020 Jun 24]. Available from: www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
2 Fielding J. Good communication will help beat COVID-19. The Hill; 2020 31 Mar [cited 2020 Jun 24]. Available from: thehill.com/opinion/healthcare/490410-good-communications-will-help-beat-covid-19
3 COVID-19: How much protection do face masks offer. Mayo Clinic. Rochester Minnesota; Mayo Clinic; 2020 [cited 2020 Jun 22]. Available from: www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-mask/art-20485449
4 Shaywitz D. Three recent reversals highlight the challenges of COVID science. Washington DC: American Enterprise Institute; 2020 Jun 22 [cited 2020 Jun 22]. Available from: www.aei.org/articles/three-recent-reversals-highlight-the-challenges-of-covid-science/
5 Duhigg C. Seattle’s leaders let scientists take the lead. New York’s did not. The New Yorker; 2020 Apr 26 [cited 2020 Jun 22]. Available from: www.newyorker.com/magazine/2020/05/04/seattles-leaders-let-scientists-take-the-lead-new-yorks-did-not
6 Hsu LY, Tan M-H. What Singapore can teach the U.S. about responding to COVID-19. StatNews; 2020 Mar 23 [cited 2020 Jun 24]. Available from: www.statnews.com/2020/03/23/singapore-teach-united-states-about-covid-19-response/
7 Hou C-Y. How South Korea is handling the coronavirus outbreak better than other countries. The Hill; 2020 Mar 13 [cited 2020 Jun 24]. Available from: thehill.com/changing-america/well-being/prevention-cures/487465-how-south-korea-is-handling-the-coronavirus
8 Woodward A. South Korea controlled its coronavirus outbreak in just 20 days. Here are the highlights from its 90-page playbook for flattening the curve. Business Insider; 2020 Apr 18 [cited 2020 Jun 24]. Available from: www.businessinsider.com/how-south-korea-controlled-its-coronavirus-outbreak-2020-4?r=AU&IR=T
9 Adam R. Singapore was ready for COVID-19 – other countries, take note. Wired; 2020 Mar 12 [cited 2020 Jun 24]. Available from: www.wired.com/story/singapore-was-ready-for-covid-19-other-countries-take-note/
10 Rosen G. An update on our work to keep people informed and limit misinformation about COVID-19. Facebook; 2020 Apr 16 [cited 2020 Jun 24]. Available from: https://about.fb.com/news/2020/04/covid-19-misinfo-update/
11 Silverman C. Pinterest Is blocking coronavirus searches, and people are very happy about it. Buzzfeed News; 2020 Mar 13 [cited 2020 Jun 24]. Available from: www.buzzfeednews.com/article/craigsilverman/pinterest-is-blocking-coronavirus-searches-and-people-are
12 World Health Organization. Infodemic Management – Infodemiology. Geneva: WHO; 2020 [cited 2020 Jun 24]. Available from: www.who.int/teams/risk-communication/infodemic-management
13 Ratzan S. Maxims for effective communication on health and risk Issues. In: Global surveillance, diagnosis and therapy of human transmissible spongiform encephalopathies: report of a WHO consultation. p. 26–7. Geneva: World Health Organization; 1998 [cited 2020 Jun 24]. Available from: www.who.int/csr/resources/publications/bse/whoemczdi989.pdf?ua=1
15 CUNY New York City COVID-19 Survey Week 12 – Part 2: Vaccines NYC: CUNY School of Public Health; 2020 [cited 2020 Jun 22]. Available from: sph.cuny.edu/research/covid-19-tracking-survey/week-12-part-2-vaccines/
17 CUNY New York City COVID-19 Survey Week 3. NYC: CUNY School of Public Health; 2020 [cited 2020 Jun 22]. Available from: sph.cuny.edu/research/covid-19-tracking-survey/week-3/
18 Ratzan SC, Gostin LO, Meshkati N, Rabin K, Parker RM. COVID-19: An urgent call for coordinated, trusted sources to tell everyone what they need to know and do. National Academy of Medicine Commentary; 2020 Mar 5 [cited 2020 Jun 24]. Available from: doi.org/10.31478/202003a
19 Glover R. Australia’s leader is winning the argument on the coronavirus. Washington Post; 2020 Apr 21 [cited 2020 Jun 4]. Available from: www.washingtonpost.com/opinions/2020/04/21/australias-leader-is-winning-argument-coronavirus/
20 False belief poison cures virus kills over 700 in Iran. AP NEWS; 2020 Apr 27 [cited 2020 Jun 16]. Available from: apnews.com/fece5d0e017849911aa86c0c07799e6b
21 World Health Organization. Coronavirus disease (COVID-19) advice for the public: Myth busters. Geneva: WHO; 2020 [cited 2020 Jun 24]. Available from: www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters
22 Bajak A., Howe J. A study said COVID wasn’t that deadly. The right seized it. The New York Times; 2020 May 14 [cited 2020 Jun 24]. Available from: www.nytimes.com/2020/05/14/opinion/coronavirus-research-misinformation.html
25 Wardle C. Fake news. It’s complicated. First Draft; 2017 Feb 16 [cited 2020 Jun 24]. Available from: medium.com/1st-draft/fake-news-its-complicated-d0f773766c79