Health service approaches to providing care for people who seek treatment for obesity: identifying challenges and ways forward
Michelle Gooey A * , Catherine Bacus B , Divya Ramachandran C D E , Milan Piya F G and Louise Baur E HA
B
C
D
E
F
G
H
Abstract
Objective: This paper aims to identify challenges in current health service approaches to providing optimal care for people who seek treatment for obesity. Type of program or service: Health service management of obesity in Australia Methods: Drawing on lived experience, clinical and academic perspectives, and available evidence, we reflect on the current state of the healthcare system to support people seeking treatment for obesity. We suggest actions to enable effective, acceptable and equitable care for this group of people. Results: Identified challenges include the complexity of care required to adequately manage obesity, existing service capability and capacity, and high out-of-pocket patient costs. Lessons learnt: To address these challenges, a comprehensive response is required at all levels of the healthcare system. As a starting point, we propose eight a–eas of action: partner with people living with obesity; eliminate weight stigma; increase healthcare professional education, guidelines and resources; establish clear referral pathways and working partnerships; scale services to meet demand; ensure flexible and accessible service delivery; implement changes to the Medicare Benefits Schedule to increase service provision and pursue opportunities for subsidised medicines.Introduction
Healthcare services in Australia fail to meet the needs of people seeking treatment for obesity. Obesity is underdiagnosed and undertreated amongst children1,2 and adults3, taking, on average, almost 9 years for an adult with obesity to seek healthcare professional help for obesity management.3 Most weight management does not occur within a healthcare setting until it increases in severity and results in complications, whether metabolic, mechanical or psychosocial.
The Australian National obesity strategy 2022–234, released in March 2022, highlights the importance of healthcare in addressing the high rates of obesity in Australia and acknowledges the urgent need for change. However, further clarity is needed regarding how this strategy will translate into practical changes at a policy and budgetary level and, more specifically, the impact on how health services and treatments will be funded and delivered.
Objectives and methods
This paper aims to identify challenges in Australia’s health service approaches to providing optimal care for people seeking treatment for obesity. Drawing on published evidence as well as personal perspectives and experiences, we reflect on the current state of the healthcare system for people seeking treatment for obesity. However, we also acknowledge that many people living with obesity require an approach that is non-medical and beyond weight loss. Additionally, given the large proportion of the population impacted by obesity, health service action should complement the community and social efforts addressing the broader social and commercial determinants of health.
As an authorship group, DR brings lived experience and research perspectives on self-directed weight loss. LB is a paediatrician with expertise in establishing and running a major paediatric weight management servic–, undertakes research on health services for paediatric and adult obesity and has worked on models of care for obesity management at the local and state level. MP is a clinical academic endocrinologist with over 14 years’ experience in the management of adults with severe obesity and bariatric surgery across multiple centres in the UK and Australia. CB is a general practitioner (GP) focusing on obesity management, has developed obesity training for primary care, and is founder of a group of general practice-based weight loss clinics for adults. MG is a public health physician currently undertaking a PhD focusing on preventing childhood obesity in healthcare settings. –
We discuss three key areas of challenge – complexity of care, service capability and capacity and out-of-pocket costs – and suggest eight areas for action to enable effective, acceptable and equitable care for people who seek treatment for obesity.
Complexity of care
Management of obesity requires multicomponent lifestyle intervention, with adjunctive pharmacotherapy and/or bariatric surgery appropriate for some people. Care is optimally delivered by a multi-disciplinary team, while also addressing relevant physical and mental health comorbidities. While the vast majority of obesity can ideally be managed in primary care, increasing severity and co-morbidities require secondary or tertiary care treatment.
Additionally, complex reasons drive gender disparities, with most patients seen both in clinics4 and undergoing bariatric surgery5 being women, despite comparable obesity rates in men and women.6 Obesity stigma, as discussed by Lawrence et al.7, is pernicious in health systems too.8,9 It negatively impacts patients’ wellbeing and engagement with the healthcare system10 and should be addressed in healthcare provision.
Despite these complexities, no current national obesity treatment guidelines are available, and there is a lack of service coordination and referral pathways across primary, secondary and tertiary care8, exacerbated by budgetary tensions between state-funded hospitals and federally-funded primary care.
Service capability and capacity
There is a paucity of services at every level of the Australian healthcare system.1,8,11,12 For example, public hospital waiting lists for speciality obesity services are months11 to years12, and there is an inadequate distribution of such services, the vast majority being in major cities.11,12 Furthermore, very few multidisciplinary specialist obesity services are available8,11, and these often restrict eligibility criteria to people with increasing complexity to manage the increasing demand.4 There is also insufficient capacity in the Australian public and private health systems to treat adults potentially eligible for bariatric surgery.13
The real-world impact of the lack of access to service is significant. For example, there is a huge gap in the provision of care for people with severe obesity who have not developed significant physical co-morbidities, thereby missing the opportunity to provide care and potentially preventing requirements for more intensive or complex treatment.
Although this paper has focused on obesity treatment, the role of prevention in ameliorating service gaps for any chronic disease is known. However, complexities unique to obesity and weight stigma raise questions about preventive services within healthcare facilities.14 Also, impacting capability and capacity are recognised barriers for preventive care within health services, such as resourcing and lack of confidence or knowledge amongst staff.15,16
Out-of-pocket costs
People seeking treatment for obesity often have significant out-of-pocket costs.8 Such costs exacerbate existing societal inequities, as increased obesity prevalence is associated with increasing levels of disadvantage as discussed elsewhere in this issue.17,18
The increasing prevalence of obesity requiring intervention and long waiting lists for bariatric surgery in the public health system have been cited as key drivers of people seeking early access to superannuation to fund bariatric surgery themselves.19 Additionally, there are obesity medications that are not subsidised by the Pharmaceutical Benefits Scheme (PBS), the mechanism by which the Australian government subsidises some medicines. For example, liraglutide (Saxenda), a medication approved for use in Australia for weight management but not PBS-subsidised, costs patients about $387 a month.20
How can we address the health service challenges?
Our health service system, with its traditional ways of service delivery and funding models, is currently not geared to manage many noncommunicable diseases, including obesity. To address this challenge, a comprehensive response is required at all healthcare system levels. As a starting point, we propose eight areas of action to address the healthcare service challenges, as summarised in Figure 1.
Actions required to address challenges in health services for people who seek treatment for obesity
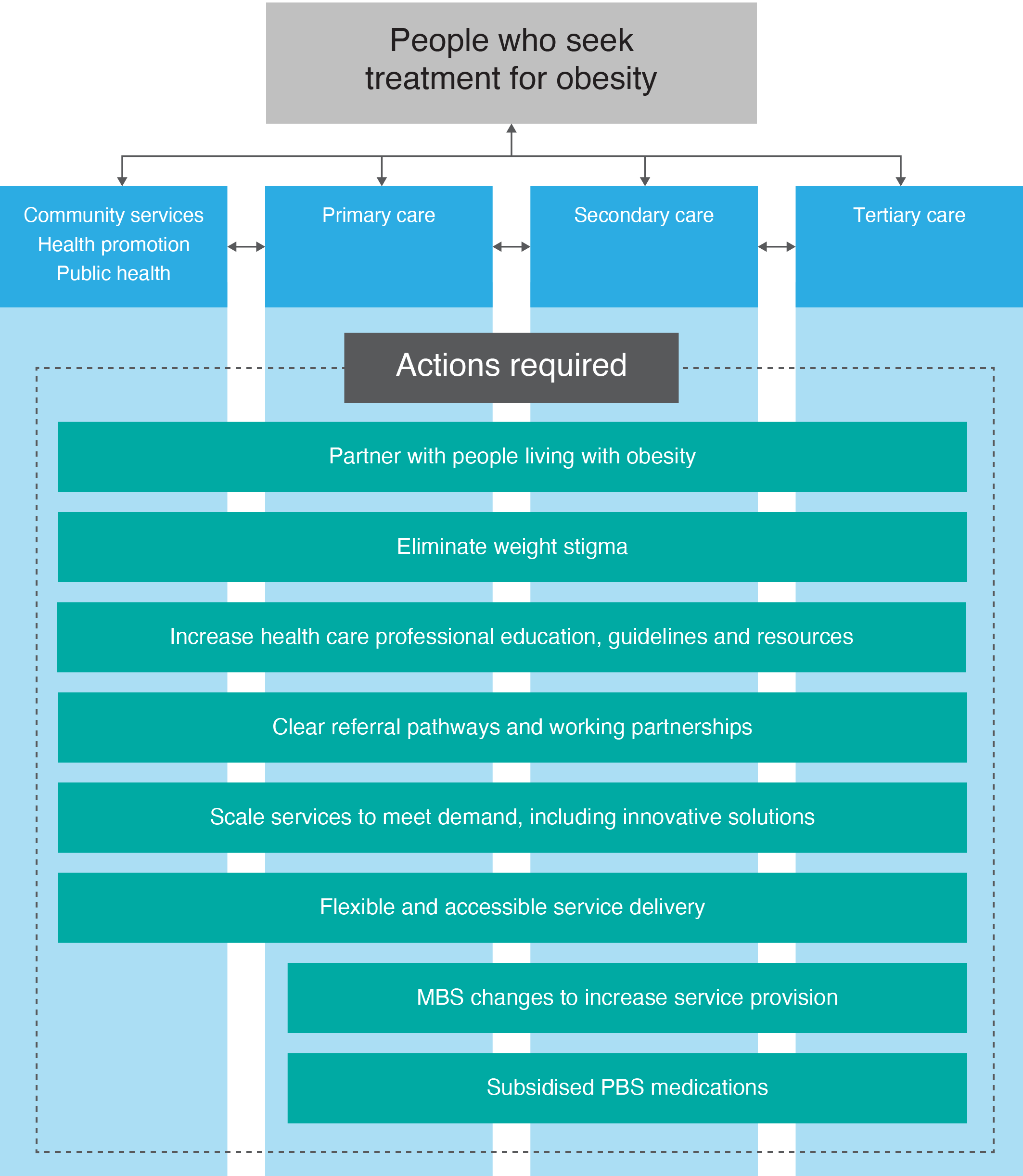
1. Partner with people living with obesity, for example, via the Weight Issues Network (WIN).21 Leveraging lived experience perspectives in all stages of healthcare intervention, service design, and delivery helps to improve and develop approaches that reach the target population and effectively meet their needs to improve treatment outcomes.
2. Eliminate weight stigma. Anti-stigma policies and resources targeted at health providers and health services are urgently needed to enable respectful and supportive interactions between people living with obesity and their healthcare providers.9
3. Increase healthcare professional education, guidelines and resources. Health professionals receive inadequate education in obesity.5 Clinical obesity management should be integrated across the syllabus for undergraduate and postgraduate levels, along with addressing any entrenched weight bias. Examples include free e-learning and resources such as NSW Health’s Weight4KIDS22, Queensland’s Clinicians Hub23 and the World Obesity Federation training program, SCOPE.24 Health services subsidised by the Australian Government are outlined by the Medical Benefits Schedule (MBS). Access to specific MBS funding for obesity care could be linked to relevant training, similar to existing mental health provisions which provide a higher rebate for GPs with further training.
Updated national obesity treatment guidelines need to be developed and disseminated to help healthcare providers navigate the complexity of obesity treatment; the utility of living guidelines could be considered to keep pace with advances in management techniques.
4. Establish clear referral pathways and working partnerships. As the frontline of the Australian healthcare system, primary care should be enabled and empowered to manage people seeking treatment for obesity, in conjunction with adequately resourced secondary and tertiary care. Readily accessible and clear referral options in both community level and secondary/ tertiary healthcare services are needed, including funding for bariatric surgery as necessary. Links between primary, secondary and tertiary healthcare to promote continuity of care and support for patients with severe obesity can be built – for example, through formal partnerships between local GPs with a special interest in obesity management and hospital-based endocrinologists in obesity clinics.
5. Scale up services to meet the demand, including innovative solutions. More innovative approaches are needed to manage the scale of the issue. For example, self-directed weight loss and maintenance interventions via smartphone apps are scalable and can empower patients. Technology can be leveraged for delivering lifestyle advice, and health professionals can monitor self-reported data. In primary care, this may include the use of practice nurses and/or health coaches who may be funded through practice incentive programs or the MBS and shared medical appointments with General Practitioners to facilitate group programs.25
6. Ensure flexible and accessible service delivery. More flexible telehealth options would enable service delivery, especially for people who cannot access services near where they live. Stronger linkages between health promotion, public health, clinical services and community services are needed to partner in obesity management, prevention and early intervention. Examples of existing partnerships include NSW Get Healthy telephone-based health coaching26 and Go4Fun27, a program for children aged 7–13 years.
7. Implement MBS changes to increase service provision. The MBS provides inadequate remuneration and/or options for relevant service provision considering the complexity of care and level of healthcare service required. For example, people with obesity who are managed under an MBS Chronic Disease Management plan can only access a total of five allied health visits per year in contrast to eating disorder plans or mental health plans that allow higher numbers of visits. People seeking treatment for obesity would greatly benefit from increased accessibility to allied health visits and higher reimbursement of allied health services. Shared medical appointments and online group programs can help meet the increased demand, yet the MBS funding model does not cater for group health delivery.
8. Seek opportunities for subsided PBS medications. Although the primary focus of obesity management is lifestyle intervention, some people require adjunctive pharmacotherapy. As new data for anti-obesity medications emerge, future opportunities for PBS subsidisation can facilitate broader and more equitable access to effective medications.
Conclusion
Our reflections on the management of obesity in the Australian health system highlight challenges that need to be addressed to provide optimal care for people seeking treatment for obesity. In partnership with patients, multilevel action is required to improve opportunities for access to adequately funded, well-integrated care. The proposed areas for action are a starting point to ensure equitable, effective and acceptable care for people seeking treatment for obesity.
Acknowledgements
MG is supported by a National Health and Medical Research Council (NHMRC) grant (GNT2005401). LB is supported by an NHMRC Leadership Fellowship (GNT2009035).
This paper is part of a special issue of the journal focusing on obesity prevention, which has been produced in partnership with the Health and Social Care Unit, School of Public Health and Preventive Medicine, Monash University, with support from VicHealth. LB and MG are guest editors for the special issue, but had no involvement in decisions about this paper.
Author contributions
All authors contributed to the content, drafting and revision of the manuscript.
Competing interests
CB reports funding from Novo Nordisk, as a member of the semaglutide advisory board and for lectures on anti-obesity medication, and from iNova Pharmaceuticals for lectures on anti-obesity medications. She is a founder and director of Alevia Medical Weight Loss, a primary-care led obesity management service in Melbourne and Adelaide and founder and director of Valita Pty Ltd which produces obesity training and management software for GPs. DR is an unpaid chairperson and board member of the Weight Issues Network (WIN). WIN receives funding from Australian government grants and not-for-profit organisations including the Australian & New Zealand Obesity Society (ANZOS), Australian & New Zealand Metabolic and Obesity Surgery Society (ANZMOSS) and The Obesity Collective. MP has received funding from Johnson & Johnson for consultancy work, staff support from Counterweight UK and meeting expenses from iNova Pharmaceuticals. He reports speakers fees from Novo Nordisk, Lilly Australia, Takeda Australia and UCB Australia. LB has received funding from Novo Nordisk as a member of a study steering committee and speakers bureau.
References
5 Backman B, Brown D, Cottrell J, Campbell A, Clancy W, Shah YH, et al. Bariatric Surgery Registry 2019/2020 annual report. Melbourne: Monash University, Department of Epidemiology and Preventive Medicine; 2020 [cited 2022 Sep 15]. Available from: www.monash.edu/__data/assets/pdf_file/0004/2582131/2021-Bariatric-Surgery-Registry_8th-Annual-Report_Amended_May.pdf
6 Australian Institute of Health and Welfare. Overweight and obesity: an interactive insight: Canbera: AIHW; 2020 [cited 2022 Aug 15]. Available from: www.aihw.gov.au/reports/overweight-obesity/overweight-and-obesity-an-interactive-insight/contents/what-is-overweight-and-obesity.
7 Lawrence BJ, de la Piedad Garcia X, Kite J, Hill B, Cooper K, Flint SW, Dixon JB. Weight stigma in Australia: a public health call to action. Public Health Res Pract. 2022;32(3):e3232224. Crossref
8 National Association of Clinical Obesity Services. National framework for clinical obesity services. Victoria: NACOS; 2020 [cited 2022 Sep 15]. Available from: www.nacos.org.au/base/wp-content/uploads/NACOSFrameworkupdated24022020.pdf
9 The Weight Issues Network. The personal costs of weight issues in Australia. Australia: WIN; 2020 [cited 2022 Sep 15]. Available from: weightissuesnetwork.org/wp-content/uploads/2022/04/revWIN-FINAL-Report-Dec2020.pdf
17 Kelly R, Hatzikiriakidis K, Kuswara K. Inequities in obesity: Indigenous, culturally and linguistically diverse, and disability perspectives. Public Health Res Pract. 2022;32(3):e3232225. Crossref
18 Petre T, Bauman A, Sumithran P, Sacks G, Lobstein T, LeRoux C, et al. A better understanding of the science and reality of obesity is urgently needed. Public Health Res Pract. 2022:32(3):e3232220. Crossref
19 The Treasury, Australian Government. Review of early release of superannuation benefits. Canberra: Australian Government the Treasury; 2018.[cited 2022 Sep 15]. Available from: treasury.gov.au/consultation/c2018-t341625
20 Colyer S. Accessibility, cost of game-changing obesity drugs problematic. Sydney: MJA Insight; 2022 [cited 2022 Sep 3]. Available from: insightplus.mja.com.au/2022/24/accessibility-cost-of-game-changing-obesity-drugs-problematic
21 Weight Issues Network. Weight Issues Network. Australia: WIN; 2022 [cited 2022 Aug 25]. Available from: weightissuesnetwork.org
22 Weight4KIDS e-Learning Portal. 2022 [cited 2022 Sep 3]. Available from: weight4kids.learnupon.com/users/sign_in?next=%2Fdashboard
23 Health and Wellbeing Queensland. Clinicians hub. Helping clinicians identify, prevent and manage obesity in children. Queensland: Queensland Government; 2020 [cited 2022 Sep 3]. Available from: https://hw.qld.gov.au/hub/
24 World Obesity Federation. SCOPE. UK: WOF; 2022 [cited 2022 Sep 3]. Available from: www.worldobesity.org/training-and-events/scope
26 NSW Government. Get Healthy. Free telephone-based health coaching. Sydney: NSW Government; 2022 [cited 2022 Sep 3]. Available from: www.gethealthynsw.com.au
27 NSW Government. Go4Fun Healthy active happy kids. Sydney; NSW Government; 2018 [cited 2022 Sep 3]. Available from: https://go4fun.com.au


