Agreement of and discussion with clients about Undetectable equals Untransmissible among general practitioners in Australia: a cross-sectional survey
Jason Wu A B * , Christopher K. Fairley
A B * , Christopher K. Fairley  B C , Daniel Grace
B C , Daniel Grace  D , Eric P. F. Chow
D , Eric P. F. Chow  B C E § and Jason J. Ong
B C E § and Jason J. Ong  B C F §
B C F §
A Kings Park Medical Centre, General Practice, 40 Gourlay Road, Hillside, Melbourne, Vic., Australia.
B Melbourne Sexual Health Centre, Alfred Health, Melbourne, Vic., Australia.
C Central Clinical School, Faculty of Medicine, Nursing and Health Sciences, Monash University, Melbourne, Vic., Australia.
D University of Toronto, Dalla Lana School of Public Health, Toronto, ON, Canada.
E Melbourne School of Population & Global Health, The University of Melbourne, Melbourne, Vic., Australia.
F Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, UK.
Sexual Health - https://doi.org/10.1071/SH23051
Submitted: 12 March 2023 Accepted: 4 May 2023 Published online: 29 May 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: The message of undetectable HIV viral load equals untransmissible (U=U) is important to reduce HIV stigma. We examined Australian general practitioner (GP)s’ agreement of and discussion with clients about U=U.
Methods: We conducted an online survey through GP networks from April to October 2022. All GPs working within Australia were eligible. Univariable and multivariable logistic regression analyses were performed to identify factors associated with: (1) agreement of U=U; and (2) discussing U=U with clients.
Results: Of 703 surveys, 407 were included in the final analysis. Mean age was 39.7 years (s.d.: 8.4). Most GPs (74.2%, n = 302) agreed with U=U, but only 33.9% (n = 138) had ever discussed U=U with clients. Key barriers to discussing U=U were lack of relevant client presentations (48.7%), lack of understanding about U=U (39.9%), and difficulty identifying those who would benefit from U=U (6.6%). Agreement with U=U was associated with greater odds of discussing U=U (adjusted odds ratio (AOR) 4.75, 95% confidence interval (CI): 2.33–9.68), younger age (AOR 0.96 per additional year of age, 95%CI: 0.94–0.99), and extra training in sexual health (AOR 1.96, 95%CI: 1.11–3.45). Discussing U=U was associated with younger age (AOR 0.97, 95%CI: 0.94–1.00), extra training with sexual health (AOR 1.93, 95%CI: 1.17–3.17), and negatively associated with working in a metropolitan or suburban area (AOR 0.45, 95%CI: 0.24–0.86).
Conclusion: Most GPs agreed with U=U, but most had not discussed U=U with their clients. Concerningly, one in four GPs were neutral or disagreed with U=U, suggesting that further qualitative research to understand this finding, and implementation research to promote U=U among Australian GPs, is urgently needed.
Keywords: barriers, general practitioners, GP, HIV, primary care, U=U, undetectable, untransmissible.
Introduction
The concept that an undetectable viral load equals untransmissible HIV infection (U=U) is supported by robust evidence from several large studies. The PARTNER1 study1 involved 548 men who have sex with men (MSM) and heterosexual HIV serodiscordant couples who reported 58 000 condomless sexual acts with no phylogenetically linked transmission of HIV. This was followed up by the PARTNER2 study,2 which had a sample of 782 MSM serodiscordant couples who reported 76 088 condomless sexual acts with no phylogenetically linked transmission. The OPPOSITES attract study3 provided further evidence, with 343 MSM couples who reported 16 800 condomless sexual acts with no linked HIV transmission. This is clear evidence that U=U, and this messaging of 100% efficacy should not be replaced with doubt-provoking comments such as ‘next to zero’ or ‘extremely low’ risk.4 These studies were completed in 2016 and 2018; however, there has still been no documented case of phylogenetically linked transmission of a person with undetectable viral load to a HIV-negative partner.
U=U has the potential to improve several health outcomes for clients living with HIV. A study from 25 countries5 showed that 718 people living with HIV who had discussed U=U with their healthcare provider were less likely to have suboptimal adherence to medications (adjusted odds ratios (AOR) = 0.59, 95% CI: 0.44–0.78), have self-reported optimal sexual health (AOR = 1.48, 95% CI: 1.14–1.92), and more likely to disclose their HIV status with other people in their life (AOR = 2.06, CI 1.50–2.84). This was compared to clients living with HIV who were completely unaware of U=U. There was a greater chance of suboptimal medication adherence when clients obtained U=U information from sources other than a healthcare provider compared to receiving information from a healthcare provider (AOR = 0.94, CI: 0.68–1.30, compared to 0.59).
Qualitative and quantitative studies have assessed healthcare providers giving information about U=U. Healthcare providers are in a prime position to inform clients about U=U and to provide reassurance of its validity. Okoli et al.5 found that approximately 34% of people living with HIV (PLHIV) have never had a U=U discussion with their healthcare providers. This study involved 25 countries (N = 2389), with 120 (5%) respondents from Australia. A study from Brazil identified that 74% of healthcare providers agreed with U=U; however, only 66% strongly agreed or agreed that PLHIV should be informed about U=U.6 Studies have reported barriers to communicating U=U from the healthcare providers’ perspective. A UK study7 identified the following barriers: hesitation with communicating zero transmission risk of HIV; and perceptions that clients may not want to hear this message. A study from Kenya8 also reported some healthcare providers were fearful that clients would blame them if HIV transmission were to occur. A Korean study9 described health providers taking a paternalistic approach and withholding U=U discussions through fear of clients taking legal action against them for transmission of HIV to others, which is unethical as it goes against the four key principles of medical ethics: respect for client’s autonomy, non-maleficence, beneficence, and justice. There are no Australian studies examining health professionals’ agreement with and discussion of U=U.
In Australia, general practitioners (GPs) can prescribe PrEP, but cannot prescribe HIV medications unless they undergo additional training to obtain accreditation as an S100 prescriber. GPs would be the most ideally placed to provide the U=U message to the key populations (clients living with HIV and partners of people with HIV), as most Australians visit a GP (84%) compared to all other medical specialities (39%).10 We conducted this study to understand what proportion of GPs in Australia was aware of and agreed with U=U and how many were discussing this with their clients. We also aimed to identify the barriers to discussing U=U to inform continuing medical education training curricula to address these barriers.
Methods
Study population and recruitment
This anonymous online survey was distributed among GPs who practised within Australia at the time of the survey (14 April−13 October 2022), including GP registrars and trainees. Surveys were ineligible if their GeoIP location was outside Australia. GeoIP location is mapping an IP address that an internet user is utilising, to a real-world location. The survey link was disseminated via a Facebook group for Australian GPs, the The Royal Australian College of General Practitioners, and through the Melbourne Sexual Health Centre (MSHC)’s website and newsletters. Consent was obtained if participants selected the ‘Agree’ button on the front page of the survey. A participant information sheet explaining the study was available on the first page. Participants who completed the survey were offered a 1 in 100 chance to win a AU$300 voucher.
Survey instrument
The survey, hosted on the Qualtrics platform (Qualtrics, North Sydney, NSW, Australia), collected data on sociodemographic characteristics, one question on agreement with U=U (‘People living with HIV who have been taking ART (antiretroviral therapy) regularly enough to achieve an undetectable viral load, cannot sexually transmit the virus to others?’) and whether they had discussed U=U with their clients (‘Have you ever discussed U=U with your patients before?’). Participants had a choice of five options from a Likert scale (strongly disagree, disagree, neutral, agree and strongly agree). For the logistic regression, we grouped the responses into a binary outcome by grouping ‘agree’ and ‘strongly agree’ as ‘Yes’ and the other responses (neutral, disagree, strongly disagree) as ‘No’. We also asked about what led to bringing up U=U with clients, the barriers associated with having a conversation about U=U, and resources they were aware of that could help with the conversation about U=U. Participants had to select from a pre-defined list of options that we felt were most likely, but they were also allowed to write down their suggestions.
Statistical analysis
We used descriptive statistics to summarise the characteristics of the study participants. Logistic regression analyses were used to identify variables associated with two outcomes: (1) agreement with U=U; and (2) discussion of U=U with clients. Variables were initially included in the multivariable model if the P-value was <0.20 in the univariable analysis. We used a backward elimination approach to derive the final multivariable model using complete case analysis. Statistical significance was defined as having a P-value of <0.05. Statistical analyses were performed using Stata (ver. 17; StataCorp, College Station, TX, USA).
Results
We received 703 survey responses, but 296 were excluded if they only had a few questions answered, were non-sensical, and/or were completed in countries outside of Australia. In 2021–2022, there were 39 259 GPs working in Australia.11
We summarised the sociodemographic characteristics of the 407 study participants included in the analysis (Table 1). The median age of the participants was 38 years, with an interquartile range (IQR) of 33–44. The median number of years of practising as a GP was six, with an IQR of 4–12.
| Characteristics | n (%) |
| Gender | |
| Male | 114 (28.0) |
| Female | 287 (70.5) |
| Non-binary | 2 (0.5) |
| I use a different term | 1 (0.3) |
| Prefer not to answer | 3 (0.7) |
| Area of practice | |
| Inner city | 83 (20.4) |
| Metropolitan or suburban | 188 (46.2) |
| Regional | 86 (21.1) |
| Rural | 47 (11.6) |
| No answer given | 3 (0.7) |
| State worked in | |
| Victoria | 160 (39.3) |
| New South Wales | 85 (20.9) |
| Queensland | 64 (15.7) |
| Western Australia | 34 (8.4) |
| South Australia | 39 (9.6) |
| Northern Territory | 6 (1.5) |
| Tasmania | 13 (3.2) |
| Australian Capital Territory | 0 (0) |
| No answer given | 6 (1.5) |
| Extra training or rotation in sexual health | |
| Yes | 161 (40) |
| No | 242 (59) |
| No response | 4 (1) |
| S100A prescriber | |
| Yes | 73 (18) |
| No | 330 (81) |
| No response | 4 (1) |
AS100 accreditation allows GPs in Australia to prescribe specialised medications such as antiretrovirals.
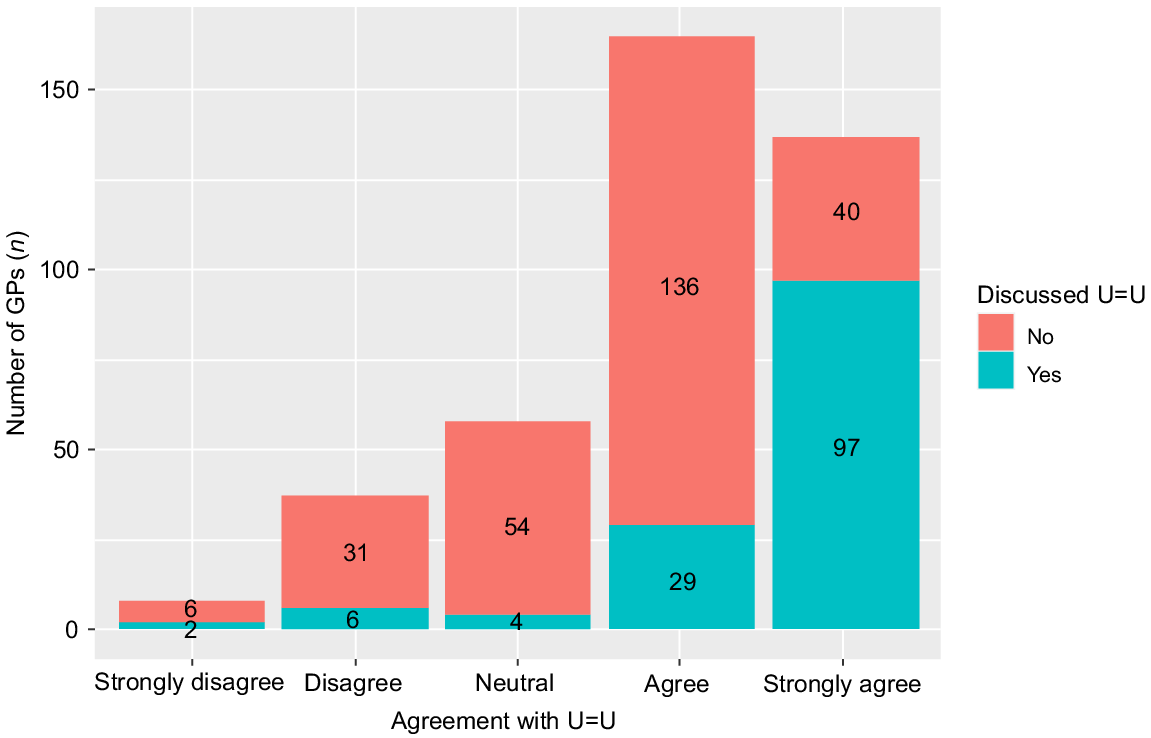
The majority (74%, 302/407) of GPs strongly agreed or agreed with U=U (33.7% strongly agreed, 40.5% agreed); however, only 33.9% (138/407) had ever discussed U=U with their clients. Fig. 1 demonstrates that the majority (70.8%, 97/137) of those who strongly agreed with U=U had ever discussed U=U with their clients; however, only a minority (17.6%, 29/165) of those who agreed with U=U had ever discussed U=U with their clients.
Number and proportion of Australian GPs who agreed with U=U and whether they had ever discussed U=U with their clients.
Facilitators among participants who discussed U=U
The situations that led to bringing up U=U included 25.9% (75/290) stating that they were talking about sexual health at the time, 23.4% (68/290) had a client who was living with HIV, 20.7% (60/290) had a client with a partner who was living with HIV, 15.5% (45/290) had a client who mentioned they would avoid having sex with someone who was living with HIV, 13.8% (40/290) had a client who had casual sex with a person living with HIV, and 0.7% (2/290) selected ‘Other’. Other included ‘Needlestick injury’ and ‘patient requested to go onto PrEP’.
Barriers to discussing U=U
The main barriers to having a conversation about U=U with their clients related to perceiving there being a lack of relevant patient presentations (48.7%, 155/318), lack of understanding (39.9%, 127/318), and difficulty identifying clients (6.6%, 21/318). Participants were allowed to describe their own barriers; in total, 13 such responses were made, with some examples including:
It makes consultations even longer when COVID time has been so stressful.
I baulk at saying ‘never’. Could it be remarkably unlikely without being impossible to transmit?
Other barriers included the client already being aware of U=U (0.3%, 1/318) and 0.6% (2/318) selected ‘I do not believe in U=U’. For a list of all written responses, refer to the Supplementary data.
Resources for U=U
The majority (59.7%, 190/318) of participants could not identify a resource to help with conversations of U=U (Supplementary Fig. S1). The response ‘sexual health website’ was recorded if the participant used this phrase or similar. However, if a more specific sexual health website was listed, this would be recorded separately. Of those who identified a resource, the most popular was from the Australasian Society of HIV, Viral Hepatitis and Sexual Health Medicine (ASHM; 15.7%, 50/318), a sexual health website (10.1%, 32/318) and the MSHC website (6%, 19/318).
Factors associated with discussing and agreeing with U=U
Table 2 demonstrates that agreement with U=U was associated with greater odds of discussing U=U (adjusted odds ratio (AOR) 4.75, 95% confidence interval (CI): 2.33–9.68), younger age (AOR 0.96 per additional year of age, 95%CI: 0.94–0.99), and received extra training in sexual health (AOR 1.96, 95%CI: 1.11–3.45). Table 3 demonstrates that discussing U=U was associated with younger age (AOR 0.97, 95%CI: 0.94–1.00), extra training in sexual health (AOR 1.93, 95%CI 1.17–3.17), and negatively associated with working in a metropolitan or suburban area (AOR 0.45, 95%CI: 0.24–0.86).
| Factors | n/N (%) | Odds ratio (95% CI) | P-value | aOR (95% CI) | P-value |
| Ever discussed U=U | |||||
| No | 163/247 (66) | 1 | 1 | ||
| Yes | 114/125 (91) | 5.34 (2.73–10.46) | <0.001 | 4.75 (2.33–9.68) | <0.001 |
| Age (years) | 0.96 (0.94–0.99) | 0.005 | 0.96 (0.94–0.99) | 0.011 | |
| Gender | |||||
| Female | 198/272 (73) | 1 | |||
| Male | 79/100 (79) | 1.4 (0.81–2.44) | 0.225 | ||
| Location | |||||
| Inner city | 55/74 (74) | 1 | |||
| Metropolitan or suburban | 132/175 (75) | 1.06 (0.57–1.98) | 0.854 | ||
| Regional | 57/77 (74) | 0.98 (0.47–2.04) | 0.967 | ||
| Rural | 33/46 (72) | 0.88 (0.38–2.01) | 0.765 | ||
| State | |||||
| Victoria | 113/147 (77) | 1 | |||
| New South Wales | 54/78 (69) | 0.68 (0.37–1.25) | 0.214 | ||
| Queensland | 44/59 (75) | 0.88 (0.44–1.78) | 0.727 | ||
| Western Australia | 22/34 (65) | 0.55 (0.25–1.23) | 0.146 | ||
| South Australia | 29/36 (81) | 1.25 (0.50–3.10) | 0.635 | ||
| Northern Territory | 4/5 (80) | 1.20 (0.13–11.13) | 0.870 | ||
| Tasmania | 11/13 (85) | 1.65 (0.35–7.83) | 0.525 | ||
| Duration of practise (years) | 0.97 (0.94–5.50) | 0.046 | |||
| Extra training | |||||
| No | 158/229 (69) | 1 | 1 | ||
| Yes | 119/143 (83) | 2.22 (1.32–3.75) | 0.003 | 1.96 (1.11–3.45) | 0.021 |
| S100 prescriberA | |||||
| No | 229/312 (73) | 1 | |||
| Yes | 48/60 (80) | 1.45 (0.73–2.86) | 0.285 | ||
| Last sexual history taken | |||||
| Less than a week ago | 202/259 (78) | 1 | 1 | ||
| Less than a month ago | 48/73 (66) | 0.54 (0.31–0.95) | 0.034 | 0.65 (0.36–1.19) | 0.162 |
| A few months ago | 26/37 (70) | 0.67 (0.31–1.43) | 0.299 | 0.94 (0.41–2.14) | 0.884 |
| A few years ago | 1/3 (33) | 0.14 (0.01–1.58) | 0.112 | 0.032 (0.002–0.51) | 0.015 |
CI, confidence interval; aOR, adjusted odds ratio. Empty cells indicate no data/analyses not run.
AS100 accreditation allows GPs in Australia to prescribe specialised medications such as antiretrovirals.
| Factors | n/N (%) | Odds ratio (95% CI) | P-value | aOR (95% CI) | P-value |
| Strongly agree or agree with U=U | |||||
| No | 11/95 (12) | 1 | 1 | ||
| Yes | 114/277 (41) | 5.34 (2.73–10.46) | <0.001 | 5.39(2.58–11.25) | <0.001 |
| Age (years) | 0.96 (0.94–0.99) | 0.007 | 0.97 (0.94–1.00) | 0.030 | |
| Gender | |||||
| Female | 81/272 (30) | 1 | |||
| Male | 44/100 (44) | 1.85 (1.15–2.97) | 0.011 | ||
| Location | |||||
| Inner city | 36/74 (49) | 1 | 1 | ||
| Metropolitan or suburban | 46/175 (26) | 0.38 (0.21–0.66) | 0.001 | 0.45 (0.24–0.86) | 0.015 |
| Regional | 25/77 (32) | 0.51 (0.26–0.98) | 0.044 | 0.72 (0.34–1.53) | 0.395 |
| Rural | 18/46 (39) | 0.68 (0.32–1.43) | 0.309 | 0.86 (0.37–1.98) | 0.716 |
| State | |||||
| Victoria | 43/147 (29) | 1 | |||
| New South Wales | 27/78 (35) | 1.28 (0.71–2.30) | 0.409 | ||
| Queensland | 18/59 (31) | 1.06 (0.55–2.05) | 0.858 | ||
| Western Australia | 14/34 (41) | 1.69 (0.78–3.66) | 0.180 | ||
| South Australia | 14/36 (39) | 1.54 (0.72–3.29) | 0.265 | ||
| Northern Territory | 3/5 (60) | 3.63 (0.59–22.48) | 0.166 | ||
| Tasmania | 6/13 (46) | 2.07 (0.66–6.53) | 0.213 | ||
| Duration of practise (years) | 0.97 (0.95–1.00) | 0.082 | |||
| Extra training | |||||
| No | 58/229 (25) | 1 | 1 | ||
| Yes | 67/143 (47) | 2.60 (1.67–4.05) | <0.001 | 1.93 (1.17–3.17) | 0.010 |
| S100 prescriberA | |||||
| No | 85/312 (27) | 1 | 1 | ||
| Yes | 40/60 (67) | 5.34 (2.96–9.65) | <0.001 | 4.35 (2.24–8.44) | <0.001 |
| Last sexual history taken | |||||
| Less than a week ago | 99/259 (38) | 1 | |||
| Less than a month ago | 16/73 (22) | 0.45 (0.25–0.83) | 0.011 | ||
| A few months ago | 8/37 (22) | 0.45 (0.20–1.01) | 0.054 | ||
| A few years ago | 2/3 (67) | 3.23 (0.29–36.11) | 0.341 | ||
CI, confidence interval; aOR, adjusted odds ratio. Empty cells indicate no data/analyses not run.
AS100 accreditation allows GPs in Australia to prescribe specialised medications such as antiretrovirals.
Discussion
This online survey among 407 Australian GPs demonstrated that although a majority agreed with U=U, only a minority had discussed U=U with clients. We add to the growing literature on promoting U=U, specifically among healthcare providers. Our study highlights the current gaps in Australian GPs’ attitudes and practice regarding U=U, providing helpful data to inform further education to improve the dissemination of the U=U message.
Our study found that only 34% of Australian GPs had ever discussed U=U with their clients. We could not identify any other study examining the proportion of doctors who discussed U=U with their clients. There was a UK study5 that reported 34% of clients living with HIV had discussed U=U with their healthcare provider, although this is not directly comparable as it involved the client perspective rather than the healthcare provider perspective. The main barriers to having the U=U conversation in our study related to the perceived lack of exposure to clients living with HIV and a lack of understanding of U=U. It is possible that GPs have a narrow view of which client groups would be suitable for a U=U conversation. For the U=U message to be the most effective, it should be shared with all clients; however, this may not be practical in a busy GP setting. So, at the minimum, it should be shared with all clients living with HIV and clients with a partner living with HIV. A public health campaign reducing stigma would be helpful to encourage more clients to disclose their HIV status with a GP. Clinics could place posters with inclusive language and positive messages regarding HIV to help encourage clients to initiate these discussions.
The other significant health communication barrier was a lack of understanding of U=U. Our study identified 26% of GPs were neutral towards or disagreed with U=U. Nunes et al.6 reported a similar result of 26% of health professionals in Brazil being neutral or disagreeing with U=U. The messages from doctors regarding HIV have been about using condoms since the 1980s, and this is entrenched, so it is difficult for GPs, especially with no training on the most updated science of HIV transmission, to believe in the accuracy of U=U. We found that agreement with U=U resulted in a doctor being 5.3-fold more likely to discuss U=U, so there is a need for better education and promotion of the U=U message to doctors for more GPs to discuss U=U with their clients. Our study also reported that two-thirds of respondents could not identify resources to learn about U=U. Together, this evidence suggests an urgent need for further training on U=U for all Australian GPs.
Interestingly, some GPs who disagreed with U=U still discussed this HIV prevention message. A possible reason might be due to them having some belief in U=U, but not 100% belief, as it is difficult in medicine to advise a client there is a ‘100% guarantee’ that something will happen. This was described by Grace et al.7: health providers describing U=U as ‘99% effective’ rather than 100%, and by Ngure et al.8 where providers used terms such as a ‘very low’ and ‘minimal’ chance of transmitting HIV. This indicates the need for training about U=U to involve presenting the data and evidence on U=U; for example, 76 088 sexual acts, with zero of these resulting in HIV transmission.2 As described by a practitioner in the study by Grace et al.,7 ‘we never talk about anything as ‘zero risk’ (in medicine)’,there needs to be an emphasis in training about how to be confident in advising that undetectable equals zero risk of transmission. As mentioned in the ASHM U=U guidance, there are risks with using terms such as ‘extremely low’ and ‘negligible’.12
For GPs who discussed U=U, the main reason they brought up the topic was that the GP was already talking about sexual health at the time (26%). It is useful for GPs to initiate discussions about sexual health with clients so it can permit the clients to bring it up. Historically, GPs have found it challenging to start conversations about sexual health with clients and/or take a sexual history: one study13 found 39% of GPs thought their clients would be very embarrassed if they were to take a sexual history. Further training should be provided on how to bring up and continue a sexual health history within a GP consult. One of the most effective ways to increase the uptake of an intervention in a GP practice is to provide a medicare item number.14 There should be a specific Medicare item for U=U discussions or more detailed sexual health discussions in general.
The strength of this study was it involved GPs working in a range of settings (metropolitan, regional and rural) and from different states and territories within Australia. Our study should be read in light of some limitations. First, we only included GPs, but there could be a benefit in future studies to include other medical specialties. Second, there could be a potential for recall or social desirability bias, although we mitigated this by the survey being anonymous. Third, this was a cross-sectional study, so we cannot infer causality. Fourth, the sample may not be representative of all GPs in Australia as it is likely that participants who had some interest in the topic of sexual health were more likely to participate and, therefore, more likely to be aware of U=U. The results may be biased by a female predominance as 70.5% of the participants were female, whereas for 2021–2022, there were 20 168 male GPs and 19 083 female GPs. This makes for a ratio of about 1.06–1.11 Future studies planned include a qualitative study to understand better how and why GPs communicate about U=U in a methodology similar to that presented by Grace et al.7 Our study identified that GPs with extra HIV training, S100 prescribers, were more likely to discuss U=U (AOR 4.35, 95%CI: 2.24–8.44); however, applying this same survey to more HIV medicine experts in Australia would be useful as a comparison. There is also a need for a study to look at what messages clients are actually receiving from services, and their understanding and use of these messages. This will help provide a better picture of U=U communication in Australia.
Conclusion
Most GPs agreed with U=U (74%), but had not discussed U=U with their clients. Concerningly, one in four GPs were neutral or disagreed with U=U, suggesting that further qualitative research to understand this finding and implementation research to promote U=U among Australian GPs is urgently needed. Detailed training on U=U is crucial to address the barriers identified by GPs: lack of ability to identify relevant client groups and lack of understanding of U=U. The most effective way to increase the proportion of GPs discussing U=U might be to increase their confidence in the evidence of U=U.
Data availability
The data that support this study are available in the article and accompanying online supplementary material.
Conflicts of interest
Jason Ong is the Editor-In-Chief and Eric Chow is a Joint Editor of Sexual Health. They were both blinded from the peer review process for this paper. There are no other competing interests.
Declaration of funding
DG is supported by a Canada Research Chair in Sexual and Gender Minority Health. EPFC and JJO are each supported by an NHMRC Emerging Leadership Investigator Grant (GNT1172873 and GNT1193955, respectively). CKF is supported by an Australian NHMRC Leadership Investigator Grant (GNT1172900).
Acknowledgements
The authors would like to thank the following organisations for their help with distributing our survey: GPs Down Under (GPDU) Facebook Group, North Western Melbourne Primary Health Network, Brisbane North Primary Health Network, Victorian primary care practice-based Research and Education Network (VicREN), the University of Melbourne, Dr Richard Teague, and Murray City Country Coast GP Training.
References
[1] Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, van Lunzen J, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA 2016; 316 171–81.| Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy.Crossref | GoogleScholarGoogle Scholar |
[2] Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet 2019; 393 2428–38.
| Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study.Crossref | GoogleScholarGoogle Scholar |
[3] Bavinton BR, Pinto AN, Phanuphak N, Grinsztejn B, Prestage GP, Zablotska-Manos IB, et al. Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. Lancet HIV 2018; 5 e438–e47.
| Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study.Crossref | GoogleScholarGoogle Scholar |
[4] Grace D, Nath R, Parry R, Connell J, Wong J, Grennan T. ‘… if U equals U what does the second U mean?’: sexual minority men’s accounts of HIV undetectability and untransmittable scepticism. Cult Health Sex 2021; 23 1270–86.
| ‘… if U equals U what does the second U mean?’: sexual minority men’s accounts of HIV undetectability and untransmittable scepticism.Crossref | GoogleScholarGoogle Scholar |
[5] Okoli C, Van de Velde N, Richman B, Allan B, Castellanos E, Young B, et al. Undetectable equals untransmittable (U = U): awareness and associations with health outcomes among people living with HIV in 25 countries. Sex Transm Infect 2021; 97 18–26.
| Undetectable equals untransmittable (U = U): awareness and associations with health outcomes among people living with HIV in 25 countries.Crossref | GoogleScholarGoogle Scholar |
[6] Nunes NN, Vasconcelos R, Cortez AL, Ferreira-Filho E, Kobayasi R, Willets C, et al. Is U=U consistently known and implemented? A survey among different medical specialists in Brazil. Int J STD AIDS 2023; 34 395–401.
| Is U=U consistently known and implemented? A survey among different medical specialists in Brazil.Crossref | GoogleScholarGoogle Scholar |
[7] Grace D, Stewart M, Blaque E, Ryu H, Anand P, Gaspar M, et al. Challenges to communicating the Undetectable equals Untransmittable (U=U) HIV prevention message: healthcare provider perspectives. PLoS ONE 2022; 17 e0271607
| Challenges to communicating the Undetectable equals Untransmittable (U=U) HIV prevention message: healthcare provider perspectives.Crossref | GoogleScholarGoogle Scholar |
[8] Ngure K, Ongolly F, Dolla A, Awour M, Mugwanya KK, Irungu E, et al. “I just believe there is a risk” understanding of undetectable equals untransmissible (U = U) among health providers and HIV-negative partners in serodiscordant relationships in Kenya. J Int AIDS Soc 2020; 23 e25466
| “I just believe there is a risk” understanding of undetectable equals untransmissible (U = U) among health providers and HIV-negative partners in serodiscordant relationships in Kenya.Crossref | GoogleScholarGoogle Scholar |
[9] Choi J-P, Seo BK. HIV-related stigma reduction in the era of undetectable equals untransmittable: the South Korean perspective. Infect Chemother 2021; 53 661–75.
| HIV-related stigma reduction in the era of undetectable equals untransmittable: the South Korean perspective.Crossref | GoogleScholarGoogle Scholar |
[10] Australian Bureau of Statistics. Patient experiences. ABS. 2021-22. Available at https://www.abs.gov.au/statistics/health/health-services/patient-experiences/latest-release
[11] Department of Health and Aged Care. General practice workforce (2015-2016 to 2021-2022 Financial Years). 2023. Available at https://hwd.health.gov.au/resources/data/gp-primarycare.html
[12] The Australasian Society of HIV, Viral Hepatitis and Sexual Health Medicine. U=U ASHM guidance for healthcare professionals. 3rd edn. (In: Allan B, editor). The Australasian Society of HIV, Viral Hepatitis and Sexual Health Medicine; 2020. Available at https://ashm.org.au/wp-content/uploads/2022/04/Resource_ASHMuuguidancehandbookFAweb.pdf
[13] Temple-Smith MJ, Mulvey G, Keogh L. Attitudes to taking a sexual history in general practice in Victoria, Australia. Sex Transm Infect 1999; 75 41–4.
| Attitudes to taking a sexual history in general practice in Victoria, Australia.Crossref | GoogleScholarGoogle Scholar |
[14] Holden L, Williams ID, Patterson E, Smith JW, Scuffham PA, Cheung L, et al. Uptake of Medicare chronic disease management incentives – a study into service providers’ perspectives. Aust Fam Physician 2012; 41 973–77.
§ Co-senior authors


