Understanding the health care needs of transgender and gender diverse people engaging with rural Australian sexual health centres: a qualitative interview study
Ava Del Tufo A * , Rosalind Foster A B , Bridget Haire A , Christy E. Newman
A * , Rosalind Foster A B , Bridget Haire A , Christy E. Newman  C , Anthony K. J. Smith
C , Anthony K. J. Smith  C , Margaret Crowley D , Donna Burn E and Anna McNulty B F
C , Margaret Crowley D , Donna Burn E and Anna McNulty B F
A Kirby Institute, Wallace Wurth Building, Corner of High Street & Botany Street, UNSW Sydney, Sydney, NSW 2052, Australia.
B Sydney Sexual Health Centre, Level 3, Nightingale Wing, Sydney Eye Hospital, 8 Macquarie Street, Sydney, NSW 2000, Australia.
C Centre for Social Research in Health, UNSW Sydney, Sydney, NSW 2052, Australia.
D Dubbo Sexual Health Centre, 203 Brisbane Street, Dubbo, NSW 2830, Australia.
E Orange Sexual Health Centre, 96 Kite Street, Orange, NSW 2800, Australia.
F School of Population Health, UNSW, Samuels Building, F25, Samuel Terry Avenue, Kensington, NSW 2033, Australia.
Sexual Health 20(4) 339-346 https://doi.org/10.1071/SH22159
Submitted: 23 September 2022 Accepted: 8 May 2023 Published: 5 June 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: Although there is a presumption that LGBTQ+ people living in rural Australia will have poorer health outcomes than those living in metropolitan areas, minimal research has focused specifically on the perspectives of transgender and gender diverse (henceforth referred to as ‘trans’) people living in these regions. The purpose of this study was to understand what health and wellbeing means to trans people in a regional or rural community and identify their health needs and experiences.
Methods: A total of 21 trans people were recruited through two regional sexual health centres (SHC) and interviewed between April and August 2021. Data were analysed via reflexive thematic analysis. This paper focuses on participants’ accounts of health and wellbeing regarding gender affirmation, the experience of rural living, respectful holistic care, safety in rural communities, isolation, loneliness, and employment.
Results: The experience of living rurally can have both positive and negative impacts on the experiences of trans people. Participants reported experiences of stigma and discrimination, reduced employment opportunities and limited social interactions, which led to feelings of isolation and loneliness; however, they also reported high quality of care, particularly with the specific SHCs which supported this research.
Conclusion: Living rurally can impact both positively and negatively on the health and wellbeing of trans peoples, and the experiences of living in this environment are diverse. Our findings challenge the perception that rural trans people experience only poor health outcomes and shows the difference that key health services such as SHCs can make in supporting trans health.
Keywords: Australia, gender affirming care, gender diversity, LGBTQ+ health and wellbeing, qualitative analysis, rural and regional health, sexual and reproductive health, transgender health.
Introduction
Transgender and gender diverse (henceforth referred to as ‘trans’) people face a variety of barriers to accessing health care including discrimination, mental health challenges and challenges accessing healthcare providers willing and able to provide appropriate forms of gender affirming care.1,2 These specific barriers could be compounded for trans people living in rural communities, wherein access to health across a range of indicators are recognised as a challenge.3 Currently, there is little to no research into the trans experience in rural Australia.4,5 This paper aims to address the trans experience in rural New South Wales to gain a better understanding of their specific health and wellbeing needs.
Trans people face increased stigma and discrimination that often leads to increased rates of self-harm, suicide and risk-taking behaviour compared to the general population. The need for increased support is particularly relevant during a trans individual’s ‘coming out’ process. A study of trans youth mental health and abuse in Australia found 79.7% have self-harmed, 82.4% have considered suicide and 48.1% have attempted suicide, with 74.6% diagnosed with depression, and 72.2% diagnosed with anxiety (data was not collected about geographical location within states or territories).6 Lack of early education, workplace discrimination and consequent under- or unemployment can make trans individuals more susceptible to situations and behaviours where their health and wellbeing may be compromised, such as sex work, substance abuse and deliberate self-harm.7,8
Specific research looking at trans experiences of stigma and discrimination in rural areas is lacking. Studies in metropolitan areas showed that when compared to cisgender lesbian, gay and bisexual (LGB) identifying individuals, trans individuals reported more discrimination and lower levels of acceptance in the community and environments such as workplaces, and higher rates of homelessness.9 This demonstrates the increased discrimination that trans peoples can face when compared to other members of LGBTQ+ communities9 and the persistent negative impact this discrimination has on mental health and wellbeing.10
One study demonstrated that LGB individuals living in rural areas report being stigmatised and discriminated against substantially more than their metropolitan counterparts.2 However in the majority of studies addressing rural populations, which are already low in number, trans participants are often grouped under the same umbrella as LGB individuals, making issues specific to trans populations difficult to separate from issues related to sexuality or sexual orientation.9
At a population level, LGBTQI+ in Australia report poorer health outcomes compared to the general population. These health disparities can be exacerbated by living in a rural area, leading to a cycle of poor health outcomes within this community.5,8,9,11 ‘Private Lives 3’, the largest national survey of LGBTQI+ individuals living in Australia, showed that LGBTQI+ populations within Australia generally report lower self-rated health and a higher burden of disease than the general population.9 Other studies have demonstrated a bi-directional link between physical and mental health and wellbeing,12 such that poor health in either domain can lead to a self-perpetuating cycle of negative outcomes in both. Rural communities often have poorer health outcomes compared with their metropolitan counterparts.5 A 2014 survey of 1032 ‘gender variant and sexually diverse’ Australian youth between the ages of 16–27 years concluded that stigma and discrimination was a systemic societal issue for these young people.8 Living in a rural area was found to have exacerbated these issues, as individuals had access to fewer support options, which may lead to social isolation and loneliness.8,11 Of the young people surveyed (who were from both rural and urban backgrounds), 41% considered self-harm or suicide, 33% had harmed themselves and 16% had attempted suicide.8
The theory of minority stress provides an explanation of why a minority group (trans people) within a minority population (LGBTIQ+ populations) may experience health disparities. ‘Minority stress’7 is the theory that a minority group’s health disparities can be explained by the stressors they experience, such as a hostile culture, victimisation, abuse and heteronormative and cisnormative assumptions.1,13 In the context of the healthcare system, these stressors often present as cumulative experiences of maltreatment, harassment, stigma, and discrimnation, which ultimately leads to decreased willingness among many trans people to access healthcare services, and poorer experiences when they do.1,7 With both rural and LGBT+ communities already facing poorer health outcomes compared to metropolitan and non-LGBT+ populations9 it does bring into question whether the culmination of minority status in the rural trans population will impact further on health status. This paper draws on qualitative interviews with trans people living in rural NSW who engage with sexual health centres (SHCs) to provide insight into the needs of this community and the impact rural living has upon trans populations.
Materials and methods
Research design
The material presented here was collected as part of a qualitative interview study of trans people and key stakeholders. The primary aim was to understand what health and wellbeing meant to trans individuals living in rural NSW, the most populous Australian state located in eastern Australia. During the development of this project, the research team consulted extensively with ACON, a non-government LGBTQ+ organisation in NSW, formerly known as the AIDS Council of NSW and the SHCs located in the Western NSW Local Health District (LHD) to ensure that the goals of the research would be of value to and in alignment with community and clinical interests. For example, while this project initially focused on the sexual health of trans people, during the consultation period it became apparent that a broader focus encompassing overall health and wellbeing were areas warranting critical attention. This article only reports on the data collection and analysis of trans participants, but interviews were also conducted with key stakeholders.
Recruitment and interview process
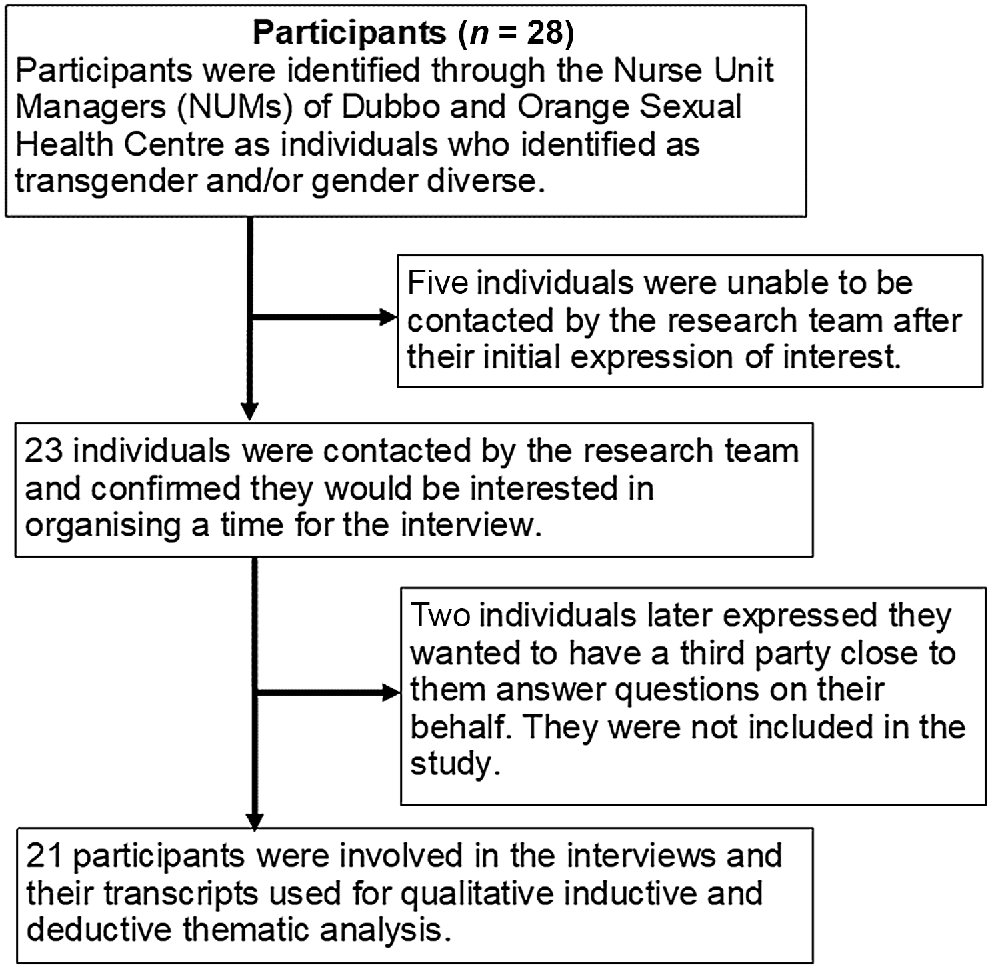
Adults identifying as transgender and/or gender diverse attending Western NSW SHCs were recruited for this study. Prospective participants were identified and invited to participate by Nurse Unit Managers from SHCs. SHCs in NSW are publicly funded sexual health services providing access to sexually transmissible infection and blood-borne virus prevention and management for identified priority populations.14 This study utilised convenience sampling as there was only a short period of time available for data collection. Participants were contacted via phone and email and if they consented to the study their details were passed on to the research team. Inclusion and exclusion criteria for these individuals as well as the recruitment process is included in Fig. 1. Nineteen of the interviews were face-to-face; however, due to coronavirus disease lockdowns in Sydney in June/July 2021, the final two interviews were conducted via Zoom. A copy of the interview guide is included in the Appendix. Interviews were conducted in person over 2 weeks in June 2021, the interview guide was developed in consultation with the authorship group and ACON, and explored experiences of living rurally, access to health care, and perspectives about health and wellbeing. Demographic questions included sex at birth, gender, sexuality, age, and highest level of education. Interviews lasted from 20 min to 2 h with the average interview time being 1 h.
Analysis
Ava Del Tufo (ADT) conducted interviews and kept a reflective journal following each interview, which included initial analytical thinking and notes about any personal perspectives or external factors shaping the interview. The audio recordings were transcribed by ADT using NVivo (QSR) Transcription, and transcripts were checked against the original recordings for accuracy. Transcripts were then de-identified, to ensure that any information, such as names, places, and organisational roles had been removed.
Data were analysed following the approach of reflexive thematic analysis.15 Initially the interviews were deductively analysed via codes developed from the original study objectives. As analysis progressed, codes were inductively added based on the meaning within interviewee responses, and previous interviews were then recoded. Coding entailed collating recurring words, ideas, and phrases and systematically ‘coding’ common themes in the interviews line-by-line and then clustering them into broader themes, managed through NVivo software. Codes were then checked for consistency and depth, as well as sufficient differentiation from each other, and then further grouped into dominant themes. Recruitment was halted when the research team identified that they had rich data that answered the research question. Attention was paid to any unusual or disconfirming cases, which provide greater nuance to the data. When 75% of the transcripts had been analysed, the investigators met to discuss and refine interpretations of themes and current findings. Saturation, member checking and triangulation were not used in this study in line with Braun and Clarke’s method of qualitative analysis as they discourage the application of these processes as incompatible with reflexive thematic analysis.16,17
Reflecting on the positionality of the researcher is an important component of reflexivity; a key aspect of rigour in qualitative research.15 The coding, data analysis and initial report were undertaken during honours research by ADT (she/her), a cisgender, non-Indigenous woman of Italian, American and Australian descent who spent 12 years of her life on a farm on the south coast of Australia. During the interview process, she kept a reflexive journal, which helped identify her positionality and how it could impact the analysis, recruitment, and interviewing. To ensure a richer and more culturally appropriate analysis, the team of trans and cisgender researchers consulted with ACON to design the study and analyse the findings.
Ethics statement
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethics approval was received from the Greater Western Human Research Ethics Committee, application number 2020/ETH02864 and the ACON Research Ethics Review Committee. Informed consent was obtained from all individual participants included in the study. Feedback was sought from ACON and staff at the regional SHCs. They provided feedback which allowed the research team to better develop the study design and interview questions while ensuring the research was needed and welcomed by the trans community and the SHCs.
Results
Personal demographic information for participants is in Table 1. Participants were transgender or gender diverse peoples who resided predominantly in Western or Far Western NSW LHDs. Twenty-one participants took part in interviews and together shared a range of experiences involving health care and their rural community. Individuals ranged in age from 18 to 60 years and there was a mix of non-binary and binary gender identities. Most participants were of Anglo-Australian descent and non-Indigenous. The following themes describe key issues related to the trans experience in rural NSW. The overarching theme was navigating gender affirmation, with the subsequent five themes reflecting key aspects of this experience: (1) lack of respectful holistic care; (2) accessibility of healthcare services; (3) safety and belonging; (4) isolation and loneliness; and (5) employment issues.
| Participant demographics (n = 21) | |
| Age range (years) | |
| 18–25 | 11 |
| 26–35 | 3 |
| 36–45 | 3 |
| 46–60 | 4 |
| Pronouns | |
| He/him | 9 |
| She/her | 7 |
| They/them | 3 |
| He/they | 2 |
| GenderA | |
| Male/man/trans man | 11 |
| Female/woman/trans woman | 7 |
| Non-binary | 5 |
| Sex assigned at birth | |
| Male | 10 |
| Female | 11 |
| Employment | |
| Employed | 13 |
| Unemployed | 7 |
| Retired | 1 |
| Sexual orientation | |
| Heterosexual | 4 |
| Pansexual | 7 |
| Gay | 4 |
| Queer | 2 |
| Asexual | 1 |
| Don’t know | 3 |
| Cultural and language background | |
| Non-Indigenous Australian | 16 |
| First Nations background (Australia and other) | 4 |
| Migrant, non-English speaking background | 1 |
| Location (postcode) | |
| Dubbo (2830) | 14 |
| Other (2395, 2800, 2820, 2850, 2866, 2870, 2873) | 7 |
| Highest qualification | |
| Year 9–11 | 6 |
| Year 12 | 4 |
| Certificate 2 | 2 |
| Certificate 3 | 6 |
| Diploma | 1 |
| Bachelor’s degree | 2 |
ATwo individuals identified as male and non-binary.
Implicit across all themes was the complexity of navigating gender affirmation. The following quote by P-3 exemplifies some of the complex range of emotions participants discussed feeling in relation to their health and body.
Well, the fact that I care about my body now and the fact that I’m not just a flesh construct, this isn’t just a vessel. I quit smoking and I’ve been smoking for 14 years, and I quit to better myself… You get depressed when certain things stop working and you get elated when certain things start growing... It [transitioning] is a wavy cycle. But you want to take care of your body, you turn from not caring to oh let’s give this a go that looks alright. (P-3, aged 26–35 years).
For trans peoples in this study, health and wellbeing meant being able to affirm their gender either socially or medically, coupled with a subsequent acceptance by society, those closest to them, and in relation to self-acceptance and affirmation.
Lack of respectful, holistic care
Access to respectful and holistic care was found to be lacking outside of the SHCs, especially regarding allied health services.
More respectful doctors, more respectful people in the system... We don’t have anyone [who] really understands what a trans person is going through. That is [a] psychologist or psychiatrist. There’s none of that up this way there’s nothing. We need that. And we need organisation… that can facilitate in this area to find out what is good for the individual… We got no social workers... that really do understand [trans people]. (P-6, aged 46-60 years).
As P-6 explained, it is not just access to care, but also access to expert or inclusive care that matters; ensuring that when trans individuals access services, they are cared for by someone who understands their needs and that these services are readily available.
Accessibility of healthcare services
In some cases, participants reported service access to be easier in rural towns because of decreased waiting times. Some spoke of waiting months to get into specialist services in Sydney and found that in western NSW they were able to access treatment comparatively quickly:
It’s been easier to get things like hormones. Originally, I went to somebody in Sydney… and that was a 4-5 month wait just to get an appointment [with an endocrinologist]. But then here [Sexual Health Centre] they were like; we can get you into a sexual health specialist. You can have hormones within three weeks. And it’s not really like known that you can do that kind of thing. I mean, they don’t advertise it [the centre] because of confidentiality and stuff. (P-5, aged 18-25 years).
Many participants were associated with the western NSW SHCs, and all of them expressed the profound positive impact the service and the staff have had and continued to have on their lives and experiences of gender affirmation:
I love everyone at the sexual health clinic. They’re like a family away from your family… You know, you get some joy out of the good and the bad with, you know, gender dysphoria and that but with them, they just make it great. (P-20, aged 18–25 years).
Safety and belonging
Participants explained that in rural communities, other people mind their own business, which strongly benefited the mental health of study participants and feelings of safety within the community:
You can make friends and get a lot more support, it’s less suffocating… (P-11, aged 18–25 years).
It’s not too bad [living rural] I think the good thing about the community out this way is they’re pretty accepting... the people I work with… have been so supportive and behind me … I’ve really struck it rich regarding the community. They’re open, they’re friendly. It does make it a lot easier. (P-21, aged 36–45 years).
Although some participants reported feeling safer in rural communities due to a smaller population and the feeling of ‘knowing everyone’, some individuals reported the opposite, citing a fear of violence:
This is not a town where I feel comfortable to go out on my own and party to four o’clock in the morning and walk home. (P-9, aged 46–60 years).
In some instances, participants even experienced physical threats of violence from members of the public, making them feel unsafe and often unwelcome in public settings:
In [town] we were outside a pub… me and my partner we weren’t even next to each other. And he started calling us faggots and poufs. And then he started saying that if we are gay, he’s going to kill us and hurt us. And then he tried to punch me. So, we bolted…It’s mostly people just saying faggot… When I go into the men’s bathroom, then the trans stuff comes out… ‘oh, you can’t use this’, ‘you can’t be in here because it’s not allowed’, ‘if you go in here, we’ll hurt you’. I only just started using men’s bathrooms two months ago and I’ve been trans for five years. I was terrified to use a men’s bathroom and getting beat up and going to a women’s bathroom and getting yelled at. (P-14, aged 18–25 years).
Isolation and loneliness
Isolation and loneliness were common themes discussed by participants. These experiences seemed more common in those who were under 25 years of age compared to those over 25 years who had begun their gender affirmation many years prior. However, both groups identified it as an issue.
You… struggle to find other [trans] people, so you feel isolated, even though there are some out there, but you just don’t know it. I don’t know what advantages there are [to living rural], if any. (P-8, aged 26–35 years).
P-12 (aged 36–45 years): Back in [capital city], I chose to be with my gay friends…I can be more myself…my gay friends they would be embracing me the way I am for who I am. .
Interviewer: Do you find it kind of lonely and isolating out here?
P-12: Yes, that’s what I miss… having friends.
Many participants reported a lack of connection to the transgender community in Sydney, as well as the broader rural communities they lived in.
Employment issues
Multiple participants reported issues concerning maintaining employment as someone who is openly trans:
I was fired from three jobs after I came out as trans. (P-19, aged 18–25 years).
Participants under the age of 25 years had experienced more frequent workplace related bullying and discrimination, which often made it difficult to maintain their employment. For example, one participant experienced multiple grievances related to employers.
My boss was so disgusted by the idea of me that she made me use the disabled bathroom… My job after that, my manager, she wouldn’t use pronouns or gender me she used to call me it. (P-20, aged 18–25 years).
Discussion
This study sought to understand trans peoples’ experiences of health and wellbeing in rural communities. While there appeared to be some advantages to living in a rural setting, participants also reported discrimination and stigma that impacted on their health and wellbeing. Our findings regarding feelings of loneliness and the impacts of stigma align to some extent with previous studies that have found that transgender identity was associated with higher odds of discrimination and depressive symptoms such as loneliness.18 In accessing health services, our findings suggest that it is vital for trans people to see evidence that they are being treated in an affirming manner by those providing healthcare services. However, such support and affirmation might not always be readily available in rural and remote settings. Many participants spoke about the need for support services and easier access to allied health services, as well as a lack of access to mental health services with staff that had training in transgender health care.
Gender-affirming and supportive health care and environments can offset the negative psychological effects of ‘minority stress’ and associated poor health outcomes.1,7,19,20 For example, Glynn et al. found that in populations of transgender women, medical, psychological and social gender affirmation was linked to lower rates of depression and higher levels of self-esteem.20 These studies, although based outside of Australia, further support the findings of our analysis. In Australia however, accessing specialist services, which includes access to gender affirming care, becomes more difficult as remoteness increases. In 2017, it was found that the proportion of allied health professionals and pharmacists was lower in regional areas and lowest in remote and very remote areas compared to major cities, and that the number of healthcare professionals as a percentage of the population decreases as remoteness increases.5 This provides a barrier to accessing gender affirming treatment, which as P-6 explained, was having a particularly detrimental impact on rural-based trans communities.
However, some participants in our study reported that smaller communities allow patients to forge a stronger relationship with service providers, which they said is unlikely to occur in metropolitan clinics. This confirmed pre-existing conclusions that although there can be poorer health outcomes for some, there can be increased comfort in social settings for others in non-urban areas when compared to metropolitan cities.21,22 Another positive impact on the community is the readily accessible care through SHCs as previously mentioned, when compared with accessing other specialist pathways, and the positive impact this is having on the community, as seen in P-20’s quote. Unfortunately, there are few studies around positive health outcomes in rural communities as published research often demonstrates a bias towards investigating and reporting negative health outcomes.21,23
A lack of acceptance of the LGBTQI+ community in rural areas was also found in a Beyond Blue study, which reported that 43% of transgender individuals did not feel safe on the street.24 During our study, we often noticed these threats of violence were due to homophobia, rather than transphobia, and the assumption that interviewees were ‘gay’. Lack of education and exposure to LGBTQ+ communities may have led to negative perceptions of transgender individuals in rural communities, providing further evidence of the need for increased awareness and education on inclusion of people of both diverse genders and sexualities. These findings contrasted with quotes by P-11 and P-21 about the positive aspect of living in a rural area; that people ‘mind their own business’ and how this promotes safety. There appears to be tension within the community regarding the narrative of trans acceptance in rural NSW. P-14 and P-9 discuss a lack of safety in their community, a direct contrast to prior quotes. Further research should explore trans people’s experiences of safety and community belonging in rural communities.
Studies have shown significant disparities between homophobic attitudes in rural areas versus metropolitan regions. By way of example, a recent poll of rural central south-west Queensland found that 50% of the population considered homosexuality to be ‘immoral’, compared to 14% in inner city Melbourne.5 As seen in P-14’s quote, trans people are often assumed to be part of the LGB community. Research shows that these homophobic perspectives were often due to decreased acceptance of non-traditional sexualities and a decrease in the LGB community presence2,25 but little research has been done into transgender experiences in rural communities.5
Peer-oriented networks and support groups can play an important role in decreasing feelings of loneliness and isolation, but they can be difficult to maintain. In 2019, the peer-trans support group based in western NSW stopped running26 due to a lack of external support. This may have contributed to increased feelings of isolation and loneliness among transgender individuals in rural communities. Although data is limited regarding trans individuals, other members of the LGBT+ community such as same sex attracted individuals, have found that one of the most important aspects to counter the experiences of stigma and marginalisation is social support.27,28 Without a social support network in western NSW the LGBT+ community would be left without an environment where they could interact socially without fear of stigma or discrimination, which is a vital aspect of maintaining mental health and wellbeing.2,29
In Australia, the unemployment rate in trans people is 19%3 while the current Australia wide unemployment rate is 4.5%.30 Furthermore, 33% of the trans population have reported discrimination due to being out as transgender in the workplace and in interviews.3 A third of the participants in our study were unemployed, confirming this research. Low rural rates of employment could also be attributed to decreased employment opportunities seen more generally throughout rural communities.21,23 There is a perpetuating cycle in society of discrimination and stigma surrounding being transgender, which is linked in with poor mental health and economic stability, and urgent attention must be paid to investing in community-led strategies to address this.7,31
This study had multiple strengths: extensive consultation with the trans community through the LGBTQI+ community organisation ACON meant that it was developed with community input and support, positioning it to address community-identified issues. However, there were some limitations to the study. All the participants were associated with western NSW SHCs. Based on participant accounts, these clinics have had a profound positive impact, which may skew our data towards a more positive outlook than if we were to study a region that is not serviced by these two clinics, or participants not linked to these clinics. Also, as mentioned in the reflexive statement the interviewer is not a member of the study population. Furthermore, this is not a generalisable sample and does not mimic the demographics present in rural areas regarding First Nations and migrant populations. A total of 16 out of 21 participants self-identified as non-Indigenous Australians; intersectional minority stress may have impacted those from more diverse backgrounds more significantly than Non-Indigenous Populations. A final limitation was that this study had more people in the 18–25 years age group compared to all other categories. A larger sample of older age groups of trans people in rural communities should be sought in future studies. In our study, most older participants reported having affirmed their gender for longer than younger participants, and these older participants often seemed more comfortable in themselves and more settled in the community.
From the results of this study, there are several implications with relevance to policy and practice change. Implementation of social support and community support groups in these communities would likely improve mental health and wellbeing and reduce the feelings of isolation and loneliness. Increasing LGBTQI+ community visibility and general community education would reduce stigma and discrimination at a societal level and lead to a more welcoming environment. There is also a need for increased education for employers regarding stigma and discrimination of trans employees. Continued support of the delivery of gender affirming health care in rural settings is needed into the foreseeable future to ensure this community continues to have access to the healthcare services they need and a environment they can feel safe and welcomed in. Furthermore, increased training of other healthcare services including the general practice workforce and mental health services could lead to more positive experiences in health care for trans individuals and increased access to appropriate care.
Conclusion
We found that many trans individuals reported stigma and discrimination within rural areas, with many younger participants (under 25 years old) feeling isolated and lonely and reporting difficulty gaining and retaining employment. However, rural communities with access to LGBTQ+ inclusive SHCs can positively benefit mental health and allow easier access to gender affirming therapy than travelling to metropolitan areas. We found that while health and wellbeing can mean different things to different people, it was commonly associated with feeling accepted by both society and self, whether that be socially, emotionally, or physically. Transgender and gender diverse peoples want to live freely and have access to health care and a community that supports them, regardless of where they live. Living rurally cannot be construed as either having a wholly positive or negative impact on the health and wellbeing of trans individuals, and the experiences of living in this environment are complex and diverse.
Data availability
Data from this study cannot be made available as it contains sensitive information that participants did not consent to sharing.
Conflicts of interest
Anna McNulty and Rosalind Foster are staff members of the Sydney Sexual Health Centre and provide medical care quarterly at the Western NSW Sexual Health Centres. Margaret Crowley and Donna Burns are the Nurse Unit Managers of the Dubbo and Orange Sexual Health Centres respectively. Anthony K J Smith (he/him) is an Associate Editor of Sexual Health but was blinded from the peer-review process for this paper. As a member of ACON’s ethics committee, he was not involved in the ethics approval of this research.
Acknowledgements
We thank the participants and key informants for taking the time to speak to us about their experiences and making this research possible; Teddy Cook for input, help and guidance throughout this project, from study design to implementation; Ruthy McIver who coordinated our ethics approval process and helped organise the transcription software needed; and Dr Chris Bourne for assisting in the interview training. We also thank the Dubbo Sexual Health Team for hosting our interviewer for 2 weeks while they conducted interviews and for their help and guidance regarding participant recruitment.
References
1 Bretherton I, Thrower E, Zwickl S, Wong A, Chetcuti D, Grossmann M, et al. The health and well-being of transgender Australians: a national community survey. LGBT Health 2021; 8(1): 42-9.
| Crossref | Google Scholar |
2 Newman CE, Smith AKJ, Duck-Chong E, Vivienne S, Davies C, Robinson KH, et al. Waiting to be seen: social perspectives on trans health. Health Sociol Rev 2021; 30(1): 1-8.
| Crossref | Google Scholar |
4 Dentato MP. The minority stress perspective. American Psychological Association. 2012. Available at https://www.apa.org/pi/aids/resources/exchange/2012/04/minority-stress
5 Morandini JS, Blaszczynski A, Dar-Nimrod I, Ross MW. Minority stress and community connectedness among gay, lesbian and bisexual Australians: a comparison of rural and metropolitan localities. Aust N Z J Public Health 2015; 39(3): 260-6.
| Crossref | Google Scholar |
6 Strauss P, Cook A, Winter S, Watson V, Wright Toussaint D, Lin A. Mental health issues and complex experiences of abuse among trans and gender diverse young people: findings from trans pathways. LGBT Health 2020; 7(3): 128-36.
| Crossref | Google Scholar |
7 Winter S, Diamond M, Green J, Karasic D, Reed T, Whittle S, et al. Transgender people: health at the margins of society. Lancet 2016; 388(10042): 390-400.
| Crossref | Google Scholar |
10 White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med 2015; 147: 222-31.
| Crossref | Google Scholar |
11 Bowman S, Nic Giolla Easpaig B, Fox R. Virtually caring: a qualitative study of internet-based mental health services for LGBT young adults in rural Australia. Rural Remote Health 2020; 20(1): 5448.
| Crossref | Google Scholar |
12 Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet 2015; 385(9968): 640-8.
| Crossref | Google Scholar |
13 Tan KKH, Treharne GJ, Ellis SJ, Schmidt JM, Veale JF. Gender minority stress: a critical review. J Homosex 2020; 67(10): 1471-89.
| Crossref | Google Scholar |
14 McCormack H, Nathan S, Varma R, Haire B. Dissonances in communication with sexual health consumers in an inner-Sydney sexual health clinic in relation to health literacy: a mixed-methods study. Health Promot J Austr 2021; 32(S1): 133-42.
| Crossref | Google Scholar |
16 Braun V, Clarke V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qual Res Sport Exerc Health 2021; 13(2): 201-16.
| Crossref | Google Scholar |
18 Su D, Irwin JA, Fisher C, Ramos A, Kelley M, Mendoza DAR, et al. Mental health disparities within the LGBT population: a comparison between transgender and nontransgender individuals. Transgend Health 2016; 1(1): 12-20.
| Crossref | Google Scholar |
19 Sevelius JM, Patouhas E, Keatley JG, Johnson MO. Barriers and facilitators to engagement and retention in care among transgender women living with human immunodeficiency virus. Ann Behav Med 2014; 47(1): 5-16.
| Crossref | Google Scholar |
20 Glynn TR, Gamarel KE, Kahler CW, Iwamoto M, Operario D, Nemoto T. The role of gender affirmation in psychological well-being among transgender women. Psychol Sex Orientat Gend Divers 2016; 3(3): 336-44.
| Crossref | Google Scholar |
25 Swank E, Frost DM, Fahs B. Rural location and exposure to minority stress among sexual minorities in the United States. Psychol Sex 2012; 3(3): 226-43.
| Crossref | Google Scholar |
27 Edwards J. Invisibility, safety and psycho-social distress among same-sex attracted women in rural South Australia. Rural Remote Health 2005; 5(1): 343.
| Crossref | Google Scholar |
28 Gottschalk L. Coping with stigma: coming out andliving as lesbians and gay men in regional and rural areas in the context of problems of rural confidentiality and social exclusion. Rural Soc Work Community Pract 2007; 12(2): 31-46.
| Google Scholar |
29 Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003; 129(5): 674-97.
| Crossref | Google Scholar |
30 Australian Bureau of Statistics. Labour force, Australia. Canberra: Australian Government; 2021. Available at https://www.abs.gov.au/statistics/labour/employment-and-unemployment/labour-force-australia/latest-release