Women’s perspectives of direct pharmacy access to oral contraception
Tara Dev A * , Pip Buckingham
A * , Pip Buckingham  A B and Danielle Mazza A *
A B and Danielle Mazza A *
A Department of General Practice, Monash University, Melbourne, Vic., Australia.
B Australian Research Centre in Sex, Health and Society, La Trobe University, Bundoora, Vic. 3083, Australia.
Australian Journal of Primary Health - https://doi.org/10.1071/PY22212
Submitted: 7 October 2022 Accepted: 6 June 2023 Published online: 3 July 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing on behalf of La Trobe University. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: Most oral contraception options require a doctor’s prescription in Australia; however, there are many models of direct pharmacy access that have been successfully implemented internationally. Despite these advancements, the most preferable OTC model for consumers is yet to be explored in the international literature, and no prior studies have determined the potential benefits of implementation in Australia. The aim of this study was to explore women’s perspectives and preferences for models of direct pharmacy access to oral contraceptive pills (OCPs).
Methods: Women participants (n = 20) aged 18–44 residing in Australia were recruited via posts on a community Facebook page and participated in semi-structured telephone interviews. Interview questions were guided by Andersen’s Behavioural Model of Health Service Use. Data were coded and thematically analysed in NVivo 12, using an inductive process to develop themes.
Results: Participants’ perspectives and preferences in relation to direct pharmacy OCP access were characterised by: (1) the importance of autonomy, accessibility and decreasing stigma; (2) confidence and trust in pharmacists; (3) health and safety concerns regarding OTC access; and (4) the need for varying OTC models to cater for both experienced and first-time users.
Conclusion: Women’s perspectives and preferences regarding direct pharmacy OCP access can be used to inform potential pharmacy practice advancements in Australia. While direct pharmacy OCP access is at the nexus of heated political debate in Australia, the potential benefits of being able to access OCPs directly from a pharmacist are evidently salient to women. Australian women’s preferred OTC availability models were identified.
Keywords: family planning services, healthcare disparities, mental health, minority health, patient-centred care, preventive health services, primary health care, quality of health care, women’s health services.
Introduction
Aside from the emergency contraceptive pill (ECP), contraceptive methods in Australia are currently prescription medicines (Australian Government, Therapeutic Goods Administration 2016). International literature suggests consumers experience barriers associated with contraceptive prescription requirements, including medical appointment costs, and temporal and geographical challenges (Landau et al. 2006; Dennis and Grossman 2012; Manski and Kottke 2015), and that eliminating the need to visit a clinician for contraceptive prescriptions would simplify and increase access (Dennis and Grossman 2012). As such, community pharmacists in over 100 countries now dispense many contraceptive methods without a medical prescription (Grossman 2015). Consistent with international evidence (Lindh et al. 2017; Teal and Edelman 2021), enhancing access to oral contraceptive pills (OCPs) is crucial as these are the most commonly used contraceptive methods in Australia (Richters et al. 2016).
There are several pharmacy-oriented models of care that could be implemented in Australia ranging from direct off-the-shelf access (as is prevalent in countries where OCPs are unregulated products) to pharmacist-prescribed OCPs (in which pharmacists perform consultations and dispensing with GP collaboration for a prescription retrospectively) (Grindlay et al. 2013). Most trialled care models involve mandatory pharmacist consultations, with some involving a screening questionnaire prior to a consultation with the pharmacist. This approach has been demonstrated as a safe and acceptable way to screen for contraindications to the OCP (Shotorbani et al. 2006; Xu et al. 2014). Prior research further indicates the vast majority of consumers are satisfied with direct pharmacy access due to increased convenience and decreased costs (Gardner et al. 2008; Parsons et al. 2013).
While international studies have suggested consumers are in favour of OTC access (Dennis and Grossman 2012; Grossman et al. 2013; Corscadden et al. 2017), there is limited research on consumer preferences in Australia. Moreover, it is important to explore women’s views on different models of OTC access (e.g. with pharmacist consultation ± self-screening or off-the-shelf) to provide information on how to best shape future models of care. While deregulation to a direct off-the-shelf model is unlikely to occur any time soon (given the Therapeutic Goods Administration declined an application to downregulate OCPs to pharmacist-only medicines in 2021) (Therapeutic Goods Administration 2021), we wanted to explore women’s thinking irrespective of the current restrictions to determine what features of direct pharmacy provision women value in potential models of care. This study aimed to investigate Australian women’s perspectives on direct pharmacy access to OCPs, their perceptions of various OTC access models, and their preferred model.
Methods
A qualitative study design using in-depth interviews was chosen to gain a detailed understanding of consumers’ perspectives on which aspects of pharmacy access were important to women and why (Kim et al. 2017). Women living in Australia, aged 18–44 years, were recruited via a post to a Facebook group due to social media’s proven effectiveness in recruiting women of reproductive age and from a younger adult demographic (Harris et al. 2015; Whitaker et al. 2017). The community group ‘Girls trade’ was selected as it aims to connect women from across Australia and trade information and items, and has a following of 66 000 members. The advertisement included a brief description of the project and link to an online eligibility survey in Qualtrics (Qualtrics, Provo, UT). To be eligible, potential participants had to have a current want/need to use oral contraception for the purpose of pregnancy prevention, i.e. they needed to have been or anticipate being sexually active with a cis man in the last 6 months or next 6 months, respectively; not currently be pregnant or trying to get pregnant; not have given birth in the last 2 months; not have undergone a hysterectomy/tubal ligation or their partner a vasectomy; and not be currently using long-acting reversible contraception (e.g. intrauterine device/implant).
After confirming their eligibility, interested potential participants provided demographic details (age, postcode, and level of education) and details of current contraceptive use using the same Qualtrics survey.
Postcodes determined the Index of Relative Socio-economic Advantage and Disadvantage (IRSAD) Census data, ranking each postcode from one through 10 (Australian Bureau of Statistics 2016). Participants were purposively sampled using IRSAD, aiming to interview at least one participant from each decile, to allow sample stratification based on age and IRSAD. While the sample size was too small for generalisation, stratification facilitated capturing major variations and comparisons, discussing differences in consumers from different socio-economic backgrounds (Patton 2015). Participants provided informed consent through an online Qualtrics form and received a A$50 gift voucher as compensation.
Rather than our recruitment methods being guided by the concept of data saturation we decided to cease recruitment after 20 interviews, having gained adequate amount and depth of data to explicate shared meanings across participants’ quotes, as aligned with reflexive thematic analysis methods (Braun and Clarke 2021).
Data collection
A semi-structured interview guide was developed (see Appendix 1) using Andersen’s Behavioural Model of Health Service Use framework (Andersen 1995). This theoretical framework explores individual health service usage considering predisposing characteristics, personal and community resources, and environment, population characteristics, health behaviour, and outcomes (Andersen 1995). Broad topic areas were established around these domains, and open-ended questions used during telephone interviews conducted by TD, a female medical student. Participants were asked about their experiences accessing contraception and their perspectives on OTC OCP access. The three OTC models trialled internationally (pharmacist consultation, self-screening questionnaires, and off-the-shelf model) were described to each participant. They were then asked to discuss the benefits and concerns associated with each model. Three pilot interviews were conducted to refine the interview guide, and field notes were taken after each interview to enhance interview effectiveness. These field notes were also used during the reflexive thematic analysis process to consider personal biases and interpretations to develop a meaningful coding framework.
Data analysis
Interviews (ranging from 25 to 45 min in length) were digitally recorded and transcribed verbatim by TD. Transcripts were imported into NVivo 12 qualitative data management software for coding and thematic analysis.
Inductive thematic analysis was used to identify themes within the qualitative data (Given 2010). The reflexive thematic analysis approach by Braun and Clarke (2019) was used, acknowledging researchers’ experiences and knowledge and how they influence one’s interpretation. TD (a medical student) and PB (a PhD student) independently coded 5 transcripts, discussing codes and identifying themes after coding the first, third and fifth interview. TD completed the remainder of the coding, regularly meeting with the other authors to discuss the coding framework and for guidance while developing themes. Our researchers (all with backgrounds in women’s health, sexual and reproductive health (SRH), pharmacy practice research, or medicine within Australia) provided their unique knowledge to interpret the meanings across participants’ responses. Themes were developed and revised iteratively, and eventually agreed upon as part of the reflexive thematic analysis, over the course of a few months (Tong et al. 2007; Allen 2017).
Results
Three-hundred and fifty-two women completed the recruitment screening survey, of which 186 met the inclusion criteria. The 20 women purposively sampled and interviewed had a median age of 22 years old (Table 1).
| Characteristic | No. of participants N | |
|---|---|---|
| Age | 18–20 | 6 |
| 21–23 | 8 | |
| 24–26 | 4 | |
| 27–29 | 2 | |
| IRSAD of postcodeA (1 = most disadvantaged, 10 = most advantaged) | 1 | 2 |
| 2 | 1 | |
| 3 | 1 | |
| 4 | 1 | |
| 5 | 2 | |
| 6 | 1 | |
| 7 | 3 | |
| 8 | 3 | |
| 9 | 2 | |
| 10 | 3 | |
| Current contraceptive | Oral contraceptive pill | 15 |
| Condoms | 3 | |
| No method | 2 | |
| Level of education | Post-graduate degree | 0 |
| Graduate diploma or graduate certificate | 0 | |
| Bachelor degree | 8 | |
| Advance diploma or diploma | 2 | |
| Year 12 or Certificate III/IV | 10 | |
| Year 11 or below | 0 | |
| Regular GP | Yes | 13 |
| No | 7 | |
| Previous unintended pregnancy | Yes | 3 |
| No | 17 | |
| Regular pharmacy | Yes | 10 |
| No | 10 | |
Four themes were identified, as described below.
The importance of autonomy, greater access and decreased stigma
Most (19/20) participants favoured OTC OCP access, citing improved accessibility and convenience as main advantages. Thirteen believed the current way of accessing OCPs (requiring a prescription from a GP) was more difficult than it needed to be.
It’s sort of like you have to jump through so many hoops to get it, you’ve got to book a doctor’s appointment, you’ve got to go to the doctor, get your script, go to the chemist, get your [pill] from the chemist. (Participant 1)
Perceived benefits of OTC OCPs included avoiding doctor’s appointment costs, convenience, confidentiality, and less travel/time required. Most participants believed OTC access would lead to increased OCPs usage, especially amongst those currently using less effective contraception methods (e.g. condoms). Two participants who had previously used OCPs (and who were not currently using any contraception), mentioned that they would likely resume OCP use if it were available OTC, citing the inconvenience of obtaining prescriptions as their reason for discontinuation.
Many participants expressed that they should have the right to access contraception simply and conveniently to take control of their own SRH. Furthermore, they believed convenient access would increase autonomy in accessing contraception of their choice.
Participants stated that direct pharmacy access would make obtaining contraception less intimidating, particularly for teenagers. They felt pregnancy prevention in young girls would be enhanced by enabling contraception to be accessed in safe and comfortable environments that are potentially less intimidating.
I think [the pharmacy] would be a lot less daunting than actually having to go to the doctor. I know that can be a little bit scary for young people and so being able to make it less daunting and say ‘oh just go to the pharmacy’. (Participant 14)
Six women (reflecting on their own teenage experiences) believed OTC OCP provision would lessen the stigma and fear of judgement associated with teenagers facing a GP seeking contraception.
I remember when I was younger, it was kind of scary to go by myself and to discuss [contraception]. I was scared they’d be like ‘oh you’re only 16, why are you sexually active?’… some teens are just quite afraid. (Participant 16)
Conversely, the main concern highlighted by most women regarding OTC access was a lack of privacy if they were to speak to the pharmacist on the pharmacy floor.
Speaking about confidential things like the pill, it’s in a public setting and everyone can hear it especially if it’s busy so it can be a bit awkward. (Participant 18)
However, women would feel comfortable if there was a private room available at the pharmacy where contraceptive counselling could occur.
I could see how some people wouldn’t like speaking just in the pharmacy… I maybe think they could have a separate small consultation room, that would be good. (Participant 16)
Confidence and trust in pharmacists
Participants reported prior positive experiences with pharmacists, holding them in high esteem, trusting them, and having confidence in advice provided. Several participants noted perceived high levels of Australian pharmacist training and accreditation.
I trust them, especially in Australia, you know they’ve got a good qualification and so I know they’re not doctors, but they still know a lot about medicine. (Participant 13)
Participants preferred speaking to a female pharmacist about their SRH. Additionally, they wanted pharmacists who could appropriately assess patients’ medical histories to identify any contraindications to OCPs.
If pharmacists could provide contraceptive counselling, the majority of women desired knowledgeable pharmacists, well trained in SRH. While eighteen participants felt pharmacists already possessed adequate knowledge, all participants believed pharmacists would benefit from extra SRH training.
I feel like if they were to have pills available over-the-counter, I would prefer them to have some training. It doesn’t have to be a long course, just kind of like the basics. (Participant 8)
Health and safety concerns
Decreased safety was a commonly cited concern regarding an OTC process. Primarily, participants were concerned that women with contraindications could access OCPs without screening. A specific concern was that pharmacists may not have access to consumers’ medical histories, compromising their capacity to make safe recommendations.
When you go to the GP, they know all your health conditions and your medical history. But if you go to the pharmacist they don’t have a close relationship with you and they can’t access your medical history. (Participant 16)
Some women from different educational backgrounds expressed concerns that OTC access to contraceptives could result in missed opportunities for important GP appointments, including discussions on preventive screening. However, when asked, all participants agreed that they would still prioritise attending separate GP appointments for preventive screening, even while accessing OCPs directly from pharmacists. This also applied to participants who were not currently using OCPs.
Following explanations on implementing self-screening questionnaires, most women liked this model and described attributes they thought were advantageous including increased privacy and comfort when discussing SRH, adequate questions to properly screen for contraindications, and providing the questionnaire in multiple languages. However, they also stated that questionnaires should be used in conjunction with broader pharmacist contraceptive counselling.
Some women had concerns regarding this method. Their main concern was that women may find it easier to be untruthful.
I hate a form cause it’s so easy to lie …. Without a conversation you don’t have the guilt, well I don’t. (Participant 5)
Few participants independently suggested an initial GP consultation for suitability assessment before accessing OCPs off the shelf. This approach would address concerns about contraindications and ensure proper health education while allowing ongoing access without further GP appointments or awkward conversations with pharmacists.
When discussing an off-the-shelf model (without pharmacist consultation), participants were concerned that consumers would not receive adequate counselling from a doctor or pharmacist regarding correct OCP use, potential OCP side-effects, and other contraceptive alternatives.
Every time I talk to someone that’s on the pill that has gotten pregnant it’s because they haven’t used it properly... like realistically, 17-year-old girls don’t sit there and read the instructions. (Participant 7)
Different over-the-counter models for different users
Women expressed that pharmacist consultations including contraindication screening, education on side effects and effective OCP use, and ongoing regular contact with pharmacists would address concerns about OTC OCP access. This model was seen as ideal for first-time OCP users, ensuring safety through screening and contraceptive counselling.
I think starting out or if you wanted to change pills or something it would be a lot more beneficial to speak to a doctor or a pharmacist just because there’s so many options and there’s different ones with different side effects. (Participant 15)
Some women wanted off-the-shelf access for repeat OCP users due to increased convenience, but emphasised the need for pharmacist availability. They cited concerns around decreased safety and a lack of education for women about correct OCP usage. Many women further stated that any model without contraindication screening or correct usage explanation was inappropriate for first-time OCP users. They suggested a model where experienced users have off-the-shelf access, while first-time users could consult a health-professional (pharmacist or GP) or complete self-screening questionnaires.
My ideal system would be for someone who had been on it for 2 years, 8 years, 10 years to be able to access it no questions asked. And for someone who was getting on it for the first time to have some sort of consultation or conversation or questionnaire to fill out before they were given it. (Participant 20)
In summary, opinions were mixed on an off-the-shelf model, with associated benefits seen as valuable to experienced OCP users tempered with concerns of inappropriateness for first-time users. Ultimately, participants concern around safety and misuse (especially in first-time users) overrode the benefit of convenience.
Discussion
Overall, we found the need to visit a GP for OCPs is perceived as not only an inconvenience, but in some cases a considerable barrier to access. Many participants would prefer to be able to access their OCP directly from a pharmacist. However, they emphasised the importance of pharmacists being appropriately trained to safely deliver contraceptive care, ensuring women are able to receive contraceptive advice in private dedicated counselling rooms.
While US studies suggest women may feel uncomfortable seeking contraception information from pharmacists due to inadequate training (Meredith et al. 2020a, 2020b), and women in Australia have previously reported reluctance to discuss their sexual health with a pharmacist (Hobbs et al. 2011), we found that women were confident in a pharmacist’s ability to provide OCPs and advice that is relevant to their contraceptive needs. Despite not all participants having a regular pharmacist, the majority still felt comfortable receiving consultations from pharmacists. This discordance between prior research and our findings may be due to participants’ perception of Australian pharmacists having undergone appropriate training necessary for consultations and prescriptionless dispensing.
Pharmacy undergraduate training in Australia includes contraception and blood pressure assessments, and pharmacists have also demonstrated their ability to safely dispense ECPs (Hobbs et al. 2011). However, Australian community pharmacists still face challenges in providing comprehensive contraceptive information and creating safe environments to have these discussions (Buckingham et al. 2023). There is evidently a need for relevant professional development or an accreditation component of potential community pharmacy OCP dispensing. Professional guidelines are also required to ensure standardised practices across the profession (Buckingham et al. 2023). For example, 11 states in the US have granted pharmacy provision of OCPs and have all mandated additional contraception-focused education for dispensing pharmacists. In Australia, a 12-month pilot program is being funded to expand pharmacist scope of practice including extending existing OCP prescriptions, after interested pharmacists undergo additional training (New South Wales Health 2022).
As the likelihood of women accessing OCPs directly from community pharmacists is strongly contingent on women’s comfort and confidence in pharmacists (Meredith et al. 2020a), any OTC model implemented must ensure women are aware that pharmacists are trained to provide these services (including counselling about pregnancy prevention). This echoes similar views of most participants in a large US qualitative study (Baum et al. 2016). Training in safe dispensing and effective communication would be necessary to overcome accessibility challenges and foster consumer confidence in pharmacists.
Some participants expressed concerns about pharmacists’ inability to access medical histories, which could limit effective screening for contraindications. To ameliorate this issue, patient-completed screening forms have been suggested as a strategy, as they have been shown to be safe and effective in community pharmacy settings (Shotorbani et al. 2006; Xu et al. 2014). The appropriateness of such screening was confirmed by our participants. Authors have also called for the better integration of community pharmacy within the primary care system, to promote interdisciplinary collaboration across physician and pharmacist professions. (Piquer-Martinez et al. 2022). This could open new possibilities for contraceptive care in Australia
Prior research consistently shows that appropriately trained pharmacists are capable of safely dispensing OCPs without direct physician involvement. The frequency of prescribing error by pharmacists in separate studies has been found to be very similar to that of physicians (between 5% and 8%) (Grossman et al. 2011; Anderson et al. 2019). In the UK, a successful initiative involved pharmacists consulting with women and determining their eligibility for OCPs based on predefined criteria (National Institute for Health and Care Excellence 2013). Out of 741 consultations, 693 people were correctly provided the OCP, and the remaining 48 individuals were referred to a primary care provider to discuss long active reversible contraception or general concerns (Parsons et al. 2013).
In our study, women recognised the need for different OTC models based on a person’s level of prior experience with OCPs (e.g., participating in a consultation with the pharmacist for inexperienced users versus off-the-shelf availability for experienced users), but emphasised the importance of maintaining preventative screening. In an international study, concerns were expressed by some GPs regarding the potential to reduce preventative screening rates (Rafie et al. 2016). This issue was also a focus of the Pharmaceutical Benefits Advisory Committee in their decision to reject the 2021 proposal to downschedule OCPs (Therapeutic Goods Administration 2021). However, all participants in our study acknowledged the importance of regular preventive screening and stated they would continue to visit their GP for these purposes even if OTC contraception were available. This is consistent with international data where a large US study found 84.8% of women stated identical intentions (Grindlay and Grossman 2018).
Strengths, limitations and future research
The study recruited participants from a single Facebook group, primarily comprising a younger adult demographic in Victoria. This may have resulted in potential socio-demographic bias. However, this may have been minimised by using stratified purposeful sampling to include women from diverse ages and IRSAD ranking. Although this study aimed to recruit women aged 18–44, our women ranged from 18 to 29 years old. Minors were not included in the study, so their opinions and experiences were not reflected. Since the study explored hypothetical models of OTC OCP access, participants’ perspectives on each model may have differed if they had experienced pharmacist contraceptive-prescribing in a real-world setting.
Reflexive thematic analysis was appropriately used to convey a story and establish patterns amongst our participants’ narratives. It was beneficial to our work as it helped facilitate discussions amongst our team, acknowledging researcher subjectivity whilst exploring themes. This was evident in the final theme of different OTC models for different users as we explored how consumer circumstance would affect their method of accessing services.
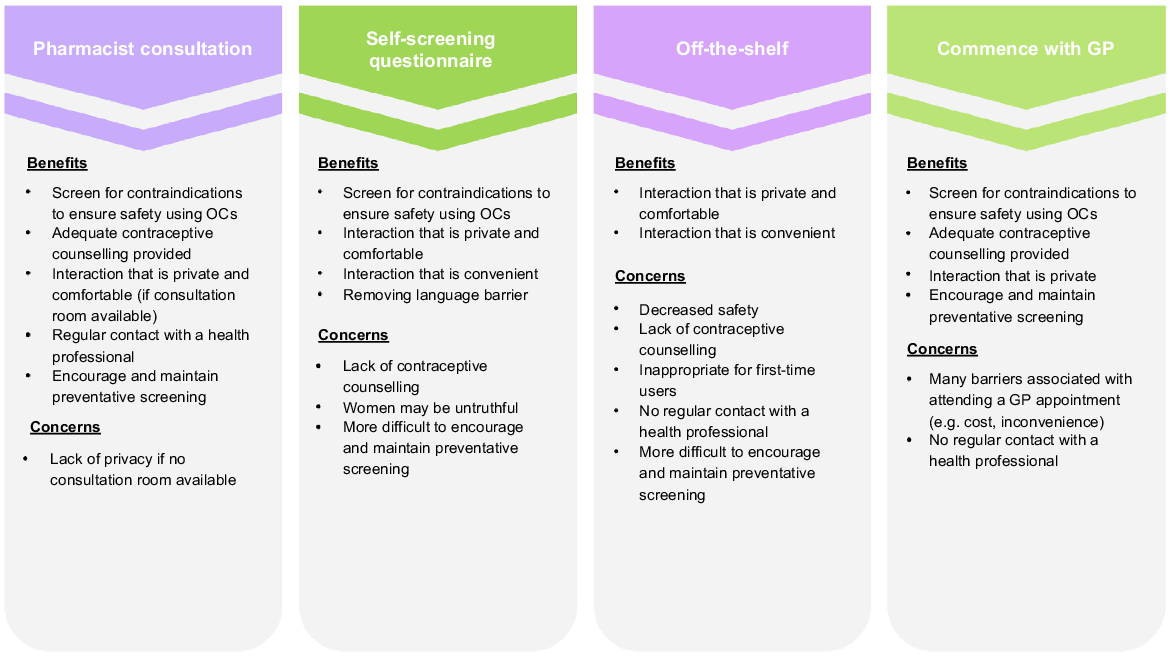
The findings of this study will be particularly useful for researchers and policy-makers when determining the core components of OTC access models (as is described in Fig. 1). This study indicates the preferred attributes identified include one-on-one consultations with pharmacists, contraindication screening, contraceptive counselling, information about preventative screening, and in-pharmacy privacy considerations Study findings also suggest women would benefit from self-screening questionnaires in combination with pharmacist consultations to enhance privacy and comfort.
Models of OTC access to OCPs and women’s perceived benefits and concerns associated with each model. Pharmacist consultation, self-screening questionnaire, and off-the-shelf were explained to the participants while commencement with a GP was independently suggested by some participants.
Further research is necessary to explore the perspectives of Australian GPs and pharmacists on OTC OCP access and its viability. Quantitative studies are needed to assess the safety and feasibility of pharmacy provision of OCPs with the desired attributes identified by consumers. Simulated pharmacist contraception-consultation encounters followed by qualitative interviews with women can provide insights into the effectiveness of this model.
Conclusion
Our study findings indicate that women generally favour OTC OCP access, aligning with global evidence highlighting women’s interest in such services provided by pharmacists. These findings have implications for future research on the feasibility of direct pharmacy provision of OCPs, which could enhance access to contraception, enhance women’s contraceptive autonomy, and reduce unintended pregnancies. Furthermore, findings on women’s concerns with OTC OCP access (and how to address them) can shape any future OTC OCP trials in Australia, and will be particularly useful when determining attributes to include in evaluations of various access models.
References
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36, 1-10.
| Crossref | Google Scholar |
Anderson L, Hartung DM, Middleton L, Rodriguez MI (2019) Pharmacist provision of hormonal contraception in the oregon medicaid population. Obstetrics & Gynecology 133, 1231-1237.
| Crossref | Google Scholar |
Baum S, Burns B, Davis L, Yeung M, Scott C, Grindlay K, Grossman D (2016) Perspectives among a diverse sample of women on the possibility of obtaining oral contraceptives over the counter: a qualitative study. Women’s Health Issues 26, 147-152.
| Crossref | Google Scholar |
Braun V, Clarke V (2019) Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health 11, 589-597.
| Crossref | Google Scholar |
Braun V, Clarke V (2021) To saturate or not to saturate? questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qualitative Research in Sport, Exercise and Health 13, 201-216.
| Crossref | Google Scholar |
Buckingham PLM, Hussainy S, Soon J, et al. (2023) Improving access to quality contraceptive counselling in community pharmacy: examining the knowledge, attitudes and practices of community pharmacists in Australia. BMJ Sexual & Reproductive Health 49, 87-96.
| Crossref | Google Scholar |
Corscadden L, Levesque J-F, Lewis V, Breton M, Sutherland K, Weenink J-W, Haggerty J, Russell G (2017) Barriers to accessing primary health care: comparing Australian experiences internationally. Australian Journal of Primary Health 23, 223-228.
| Crossref | Google Scholar |
Dennis A, Grossman D (2012) Barriers to contraception and interest in over-the-counter access among low-income women: a qualitative study. Perspectives on Sexual and Reproductive Health 44, 84-91.
| Crossref | Google Scholar |
Gardner JS, Downing DF, Blough D, Miller L, Le S, Shotorbani S (2008) Pharmacist prescribing of hormonal contraceptives: results of the direct access study. Journal of the American Pharmacists Association 48, 212-226.
| Crossref | Google Scholar |
Grindlay K, Grossman D (2018) Interest in over-the-counter access to a progestin-only pill among women in the United States. Women’s Health Issues 28, 144-151.
| Crossref | Google Scholar |
Grindlay K, Burns B, Grossman D (2013) Prescription requirements and over-the-counter access to oral contraceptives: a global review. Contraception 88(1), 91-96.
| Crossref | Google Scholar |
Grossman D (2015) Over-the-counter access to oral contraceptives. Obstetrics and Gynecology Clinics of North America 42, 619-629.
| Crossref | Google Scholar |
Grossman D, White K, Hopkins K, Amastae J, Shedlin M, Potter JE (2011) Contraindications to combined oral contraceptives among over-the-counter compared with prescription users. Obstetrics & Gynecology 117, 558-565.
| Crossref | Google Scholar |
Grossman D, Grindlay K, Li R, Potter JE, Trussell J, Blanchard K (2013) Interest in over-the-counter access to oral contraceptives among women in the United States. Contraception 88, 544-552.
| Crossref | Google Scholar |
Harris ML, Loxton D, Wigginton B, Lucke JC (2015) Recruiting online: lessons from a longitudinal survey of contraception and pregnancy intentions of young Australian women. American Journal of Epidemiology 181, 737-746.
| Crossref | Google Scholar |
Hobbs MK, Taft AJ, Amir LH, et al. (2011) Pharmacy access to the emergency contraceptive pill: a national survey of a random sample of Australian women. Contraception 83, 151-158.
| Crossref | Google Scholar |
Kim H, Sefcik JS, Bradway C (2017) Characteristics of qualitative descriptive studies: a systematic review. Research in Nursing & Health 40, 23-42.
| Crossref | Google Scholar |
Landau SC, Tapias MP, Mcghee BT (2006) Birth control within reach: a national survey on women’s attitudes toward and interest in pharmacy access to hormonal contraception. Contraception 74, 463-470.
| Crossref | Google Scholar |
Lindh I, Skjeldestad FE, Gemzell-Danielsson K, et al. (2017) Contraceptive use in the Nordic countries. Acta Obstetricia et Gynecologica Scandinavica 96, 19-28.
| Crossref | Google Scholar |
Manski R, Kottke M (2015) A survey of teenagers’ attitudes toward moving oral contraceptives over the counter. Perspectives on Sexual and Reproductive Health 47, 123-129.
| Crossref | Google Scholar |
Meredith AH, Olenik NL, Farris KB, Hudmon KS (2020a) Women’s perceptions of pharmacist-prescribed hormonal contraception. Journal of the American College of Clinical Pharmacy 3, 425-432.
| Crossref | Google Scholar |
Meredith AH, Vahary EB, Wilkinson TA, Meagher CG, Vielott T, Ott MA (2020b) Adolescents’ perceptions of contraception access through pharmacies. Pharmacy 8, 53.
| Crossref | Google Scholar |
Parsons J, Adams C, Aziz N, Holmes J, Jawad R, Whittlesea C (2013) Evaluation of a community pharmacy delivered oral contraception service. Journal of Family Planning and Reproductive Health Care 39, 97-101.
| Crossref | Google Scholar |
Piquer-Martinez C, Urionagüena A, Benrimoj SI, et al. (2022) Integration of community pharmacy in primary health care: the challenge. Research in Social and Administrative Pharmacy 18, 3444-3447.
| Crossref | Google Scholar |
Rafie S, Kelly S, Gray EK, Wong M, Gibbs S, Harper CC (2016) Provider opinions regarding expanding access to hormonal contraception in pharmacies. Women’s Health Issues 26, 153-160.
| Crossref | Google Scholar |
Richters J, Fitzadam S, Yeung A, et al. (2016) Contraceptive practices among women: the second Australian study of health and relationships. Contraception 94(5), 548-555.
| Crossref | Google Scholar |
Shotorbani S, Miller L, Blough DK, Gardner J (2006) Agreement between women’s and providers’ assessment of hormonal contraceptive risk factors. Contraception 73, 501-506.
| Crossref | Google Scholar |
Teal S, Edelman A (2021) Contraception selection, effectiveness, and adverse effects: a review. JAMA 326, 2507-2518.
| Crossref | Google Scholar |
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care 19, 349-357.
| Crossref | Google Scholar |
Whitaker C, Stevelink S, Fear N (2017) The use of facebook in recruiting participants for health research purposes: a systematic review. Journal of Medical Internet Research 19, e290.
| Crossref | Google Scholar |
Xu H, Eisenberg DL, Madden T, Secura GM, Peipert JF (2014) Medical contraindications in women seeking combined hormonal contraception. American Journal of Obstetrics and Gynecology 210, 210.e1-210.e5.
| Crossref | Google Scholar |
Appendix 1. Interview guide
Basic demographic information collected
Semi-structured interview guide with probing questions underneath
Demographics
Can you tell me a little bit about your experience accessing your current form of contraception?
What contraception are you currently using?
How do you obtain your current contraception? Prompt: GP then pharmacist? How many repeats?
How do you manage prescriptions? Prompt: Do you keep them at home or leave them at the pharmacy?
Have you ever encountered difficulties accessing contraception?
What do you think are some barriers to accessing contraception?
Can you tell me a little bit about your experience with accessing any medication from a pharmacy?
There has been talk about making the pill available over-the-counter. This would mean that you wouldn’t need to see a doctor for a prescription in order to obtain the pill and could buy it directly off the shelf in a pharmacy. Another option would be to make it only available in pharmacies where you wouldn’t need a prescription but you would need to speak to the pharmacist first to see if the pill is suitable for you. What are your thoughts on this?
What do you think are some advantages to having the pill be over-the-counter?
What do you think are some disadvantages to having the pill over-the-counter?
Do you think that it is safe enough to purchase the pill over-the-counter? Why or why not?
What are the benefits and drawbacks of making the pill available over-the-counter for the general population?
Can you tell me whether you would be interested in using oral contraceptives (e.g. the pill) if they were available over the counter and explain why or why not?
Under what circumstances would you access the pill over-the-counter? Prompt: Would it be something that you would use regularly or if your supply runs out?
If you are not interested in personally using the pill over-the-counter, would it be something you are in favour of for other women?
If you were able to access the pill over-the-counter, would you still attend a general practitioner for routine health screening e.g. CST, STI screen?
Two ways to access the pill over-the-counter would be directly off the shelf or following a consultation with a pharmacist. Would you prefer one of these methods over the other?
Would pharmacy access only (where a pharmacist would need to be consulted with before obtaining the pill) be something to help lessen your concerns about the pill being available over-the-counter?
How do you feel about pharmacists’ level of knowledge about things like a consumer’s medical history and knowledge about the pill to appropriately counsel and supply contraception?
How do you feel about having a consultation with a pharmacist at the pharmacy before accessing oral contraception?
Another method of accessing the pill over-the-counter in pharmacies would be to use a questionnaire where women would fill out a form where they are asked questions about their medical history to assess safe use of the pill. What do you think about this?
Is there anything else you would like to add?
*Questions in bold will be asked to all participants. Other questions will be used to prompt participants if appropriate.


