Young Australians’ receptiveness to discussing sexual health with a general practitioner
Helen Bittleston A * , Jane S. Hocking
A * , Jane S. Hocking  A , Jacqueline Coombe
A , Jacqueline Coombe  A , Meredith Temple-Smith
A , Meredith Temple-Smith  B and Jane L. Goller
B and Jane L. Goller  A
A
A Melbourne School of Population and Global Health, The University of Melbourne, Carlton, Vic. 3010, Australia.
B Department of General Practice, The University of Melbourne, Carlton, Vic. 3010, Australia.
Australian Journal of Primary Health - https://doi.org/10.1071/PY23083
Submitted: 1 May 2023 Accepted: 24 July 2023 Published online: 24 August 2023
© 2023 The Author(s) (or their employer(s)). Published by CSIRO Publishing on behalf of La Trobe University. This is an open access article distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND)
Abstract
Background: Most sexual health care in Australia is provided through general practice. However, many young Australians experience barriers to accessing sexual health care. This research examines young Australians’ receptiveness to discussing sexual health with a general practitioner (GP).
Methods: We conducted an anonymous online sexual health survey (open 2 May to 21 June 2022). Anyone living in Australia aged 16–29 years was eligible to participate. Participants were recruited via social media and asked whether they agreed with five statements exploring their receptivity to discussing sexual health with GPs. We explored characteristics associated with responses using multivariable logistic regression.
Results: Among 1915 participants, 69.3% were cisgender women, with a median age of 20 years; 48.5% were heterosexual. Approximately one-fifth agreed they might not tell a GP the whole truth about their sexual history, would be worried about confidentiality when discussing their sexual history and would be too embarrassed to see their usual GP if they thought they had a sexually transmitted infection. Over half (55.8%) agreed they would be comfortable with a GP bringing up sexual health in an unrelated consultation, but 39.6% would be nervous to bring up sexual health in case they needed an intimate examination. Multivariate regression identified several characteristics associated with responses. Notably, having a school-based sex education and a usual GP were factors associated with increased receptivity to discussing sexual health.
Conclusions: Young Australians were generally open to discussing sexual health with a GP. School-based sex education and GP–patient relationships are key to promoting sexual health among young people.
Keywords: access to health care, general practice, online survey, primary health care, quantitative research, sexual health, sexually transmissible infections, young people.
Background
The prevention, detection and comprehensive management of sexually transmissible infections (STIs) is a key component of sexual health care for young people. STI notifications are highest among young people, and (prior to the COVID-19 pandemic) were increasing throughout high-income countries, including Australia (King et al. 2022). In particular, chlamydia (the most frequently notified bacterial STI in Australia) impacts young people, with 70% of the 86 916 cases in 2021 diagnosed among 15–29-year-olds (King et al. 2022). Left untreated, chlamydia and gonorrhoea can lead to pelvic inflammatory disease in people with female reproductive organs, which in turn can cause infertility, ectopic pregnancy and chronic pelvic pain (Bateson and Edmiston 2016). The recent resurgence of syphilis that has been observed globally is also of considerable concern in Australia (King et al. 2022). Syphilis can cause irreversible, severe complications, and is particularly dangerous for pregnant people and their infants (Genc 2000; Hook 2017). Opportunistic STI testing for young people (aged 15–29 years) is recommended by the Australian STI management guidelines, with a standard asymptomatic check-up including testing for chlamydia, gonorrhoea and syphilis, as well as HIV and hepatitis B (Australasian Sexual Health Alliance 2022; Ong et al. 2022). Timely access to STI testing is key to reducing STI rates and improving health outcomes (e.g. reducing the risk of complications) through effective and comprehensive management of infections (Fairley et al. 2022).
Sexual health is a broad term that encompasses many aspects of young people’s health, including fertility regulation, sexual violence prevention and sexual functioning (WHO 2006; Mitchell et al. 2021). In addition to STI testing and management, young people require access to care for other aspects of their sexual health and wellbeing. For example, many young women opt to use short-acting hormonal contraceptives (Harris et al. 2020), available through primary care (although, despite high adoption of contraceptive methods among young women, high rates of unplanned pregnancy continue throughout Australia; Rowe et al. 2016). Furthermore, although there is little Australian research that considers young people’s sexual functioning and unmet need for care for sexual difficulties and dysfunction, some recent evidence suggests that sexual difficulties are common among young men (Schlichthorst et al. 2016), and research conducted overseas suggests that sexual dysfunction may be more common among young women (Moreau et al. 2016).
For young people in Australia, general practice is a key setting for sexual health care. Most Australians visit a general practitioner (GP) each year (AIHW 2022), providing opportunities to promote and deliver sexual health care to patients. Other sexual health services (for example, sexual health clinics and family planning centres) provide comprehensive sexual health care to many young people in Australia. However, availability of services varies by location, and many are overburdened. Australian sexual health providers have recently stressed the importance of increasing sexual health services within general practice, leaving specialist services with the capacity to focus on priority populations (Kularadhan et al. 2022).
We know that many young people in Australia and internationally do not access timely sexual health care for a range of reasons, including embarrassment or concerns about being judged by health care providers (Pavlin et al. 2008; Baker et al. 2013; Hoopes et al. 2017), difficulty accessing appropriate and/or affordable services (Adam et al. 2019; AIHW 2022), and concerns about confidentiality (Baker et al. 2013; Kang et al. 2014; Hoopes et al. 2017). Some GPs also struggle to find the space to initiate sexual health conversations with patients. For example, a recent study involving interviews with Victorian GPs found that raising sexual health in unrelated consultations with young male patients was not necessarily routine or straightforward for all GPs (Collyer et al. 2018). Other research conducted overseas has also identified that addressing sexual health proactively in primary care is challenging for many providers, due to issues, such as time constraints, complexity and sensitivity of issues, and a lack of training (Gott et al. 2004; Zannoni et al. 2021). Despite these challenges, primary care remains a crucial setting for the provision of sexual health care to young people, and sexual and reproductive health care is a key component of general practice.
In this paper, we sought to understand young Australian’s receptiveness to discussing sexual health with GPs. We explored how open young people are to having sexual health raised opportunistically in unrelated consultations, and barriers to initiating and having open and honest discussions about sexual health with GPs.
Methods
We conducted an online survey to explore various aspects of young people’s sexual and reproductive health. The survey was open for 7 weeks in 2022 (2 May to 21 June), and anyone aged between 16 and 29 years, being a high-risk age group for STIs, who was living in Australia was eligible to participate. All survey questions were reviewed by colleagues (including graduate students aged <30 years) for clarity and appropriateness. The survey was administered via Qualtrics survey software, and distributed via paid social media (Facebook and Instagram) advertisements. Advertisements were further circulated among the researchers’ networks (for example, via student and staff university noticeboards). To encourage survey participation and completion, we offered a prize draw incentive, whereby respondents who reached the end of the survey could provide their email address to win one of five A$100 vouchers.
Participants were presented with information about the study and had to confirm their consent before progressing to questions. Any questions could be left unanswered, with the exception of eligibility and consent questions.
Basic demographic information was collected at the beginning of the survey, including age, gender identity and postcode of residence. A matrix style question asked participants whether they agreed or disagreed with five statements related to discussing sexual health with a GP. These statements were developed to determine whether some previously identified barriers to accessing sexual health care (including embarrassment, confidentiality and fear of intimate examinations) continue to be important to young people. Participants could also select ‘neutral or unsure’. The five statements read as follows within the survey:
I would be too embarrassed to see my usual GP if I thought I had an STI
If a GP asked about my sexual history, I might not tell them the whole truth
I would be worried about confidentially when discussing my sexual history with a GP
I would be OK with a GP asking me about my sexual health if I was seeing them for an unrelated reason
I would be nervous about bringing up sexual health with a GP in case I needed to have an intimate examination or test (e.g. examination of genitals)
We calculated the proportion of respondents who agreed with each statement, along with 95% confidence intervals. We also explored characteristics associated with agreement with each statement using univariable and multivariable logistic regression models. Characteristics associated with each statement in the univariable models were retained in multivariable models, although a priori we included sexuality, age and gender in multivariable models due to their importance to the outcomes, as these factors have been previously found to be associated with patterns and experiences of accessing of primary care services (Alencar Albuquerque et al. 2016; AIHW 2022).
Independent variables included in the models were age group (categorised as: 16–17, 18–20, 21–24, and 25–29 years), sex/gender (female/woman, male/man, gender diverse), sexuality (heterosexual, gay/lesbian, bisexual/pansexual, something else) and country of birth (Australia, overseas and ≤5 years in Australia, overseas and >5 years in Australia). Binary variables were derived from data for Aboriginal or Torres Strait Islander status, metropolitan location, any history of partnered sexual activity, school-based sex education and has a usual GP.
All analyses were performed in Stata 16.0.
Ethics approval
Ethics approval was provided by the University of Melbourne Ethics Committee (ID: 22475). This research was undertaken with the informed consent of all participants.
Results
Respondent characteristics
Among 1915 participants, 69.3% were cisgender women, with a median age of 20 years (interquartile range 17–24 years), approximately half were heterosexual (48.5%), 86.4% reported receiving sex education at school and 66.9% had a usual GP (Table 1).
| Characteristic | n | % | |
|---|---|---|---|
| GenderA | Cisgender women | 1323/1910 | 69.3 |
| Cisgender men | 413/1910 | 21.6 | |
| Trans and gender diverse | 174/1910 | 9.1 | |
| Age group (years) | 16–17 | 577/1836 | 31.4 |
| 18–20 | 406/1836 | 22.1 | |
| 21–24 | 438/1836 | 23.9 | |
| 25–29 | 415/1836 | 22.6 | |
| SexualityB | Heterosexual | 923/1902 | 48.5 |
| Gay/lesbian/queer | 298/1902 | 15.7 | |
| Bisexual/pansexual | 591/1902 | 31.1 | |
| Something else | 90/1902 | 4.7 | |
| Sex educationC | Yes | 1655/1915 | 86.4 |
| Usual GP | Yes | 1279/1913 | 66.9 |
| Sexually activeD | Yes | 1502/1912 | 78.6 |
| Aboriginal and/or Torres Strait Islander | Yes | 53/1902 | 2.8 |
| Lives in major city | Yes | 1587/1887 | 84.1 |
| Country of birth | Australia | 1549/1891 | 81.9 |
| Overseas, >5 years in Australia | 226/1891 | 12.0 | |
| Overseas, ≤5 years in Australia | 116/1891 | 6.1 |
AParticipants could select multiple gender identities. ‘Trans and gender diverse’ people includes respondents who said they were transgender and/or selected agender, non-binary, genderfluid/genderqueer or self-described their gender and did not also select ‘man’ or ‘woman’.
BParticipants could select multiple sexuality options. Those who selected ‘queer’ only were included with gay/lesbian respondents unless they also selected bisexual or pansexual. ‘Something else’ includes asexual and questioning or unsure men and women who did not select another sexuality.
CSchool-based sex education, those who could not remember were included with ‘no’.
DReported any partnered sexual activity (including vaginal, anal and oral sex, as well as any other sexual contact with another person).
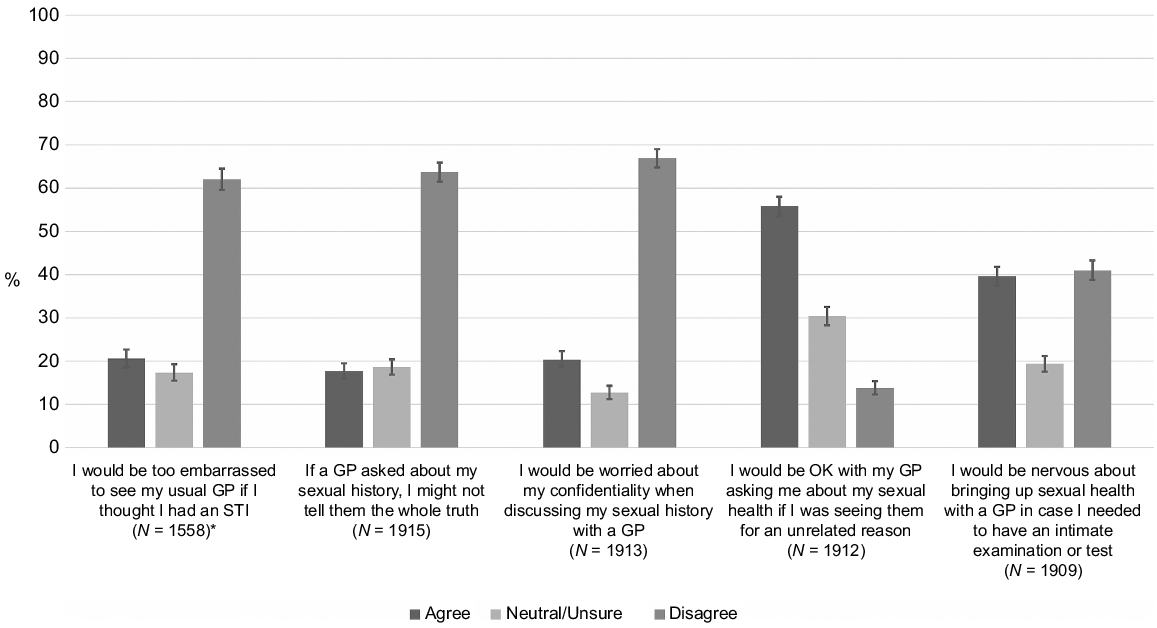
Proportions of responses to each statement are shown in Fig. 1. All multivariable analysis findings are shown in Table 2, and univariable data are available in the supplementary material.
Participant responses to statements about discussing sexual health with general practitioners. *Only including participants who said they have a usual GP.
| Statement 1: I would be too embarrassed to see my usual GP if I thought I had an STIA (N = 1558) | Statement 2: If a GP asked about my sexual history, I might not tell them the whole truth (N = 1915) | Statement 3: I would be worried about confidentiality when discussing my sexual history with a GP (N = 1913) | Statement 4: I would be OK with a GP asking me about my sexual health if I was seeing them for an unrelated reason (N = 1912) | Statement 5: I would be nervous about bringing up sexual health with a GP in case I needed to have an intimate examination or test (N = 1909) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | aOR (95%CI) | n (%) | aOR (95%CI) | n (%) | aOR (95%CI) | n (%) | aOR (95%CI) | n (%) | aOR (95%CI) | |
| Overall | 321 (20.6) | – | 339 (17.7) | – | 391 (20.4) | – | 1066 (55.8) | – | 756 (39.6) | – |
| GenderB | ||||||||||
| Woman | 228 (20.8) | REF | 241 (18.2) | REF | 270 (20.4) | REF | 719 (54.4) | REF | 523 (39.7) | REF |
| Man | 62 (19.9) | 1.0 (0.7–1.4) | 69 (16.7) | 0.9 (0.7–1.3) | 88 (21.4) | 1.1 (0.8–1.4) | 262 (63.6) | 1.5 (1.2–1.9)** | 145 (35.3) | 0.8 (0.6–1.0) |
| Trans and gender diverse | 31 (20.8) | 0.7 (0.5–1.2) | 27 (15.5) | 0.8 (0.5–1.3) | 30 (17.2) | 0.7 (0.4–1.1) | 83 (47.7) | 0.9 (0.6–1.2) | 85 (48.9) | 1.1 (0.8–1.6) |
| Age group (years) | ||||||||||
| 16–17 | 153 (33.3) | 7.1 (4.3–11.8)*** | 143 (24.8) | 2.6 (1.8–3.8)*** | 203 (35.3) | 7.4 (4.8–11.2)*** | 270 (47.0) | 0.4 (0.3–0.6)*** | 328 (57.1) | 4.5 (3.3–6.1)*** |
| 18–20 | 68 (20.8) | 4.1 (2.4–7.0)*** | 67 (16.5) | 1.6 (1.0–2.3)* | 83 (20.4) | 3.4 (2.2–5.4)*** | 215 (53.0) | 0.5 (0.4–0.7)*** | 182 (44.8) | 2.8 (2.1–3.9)*** |
| 21–24 | 59 (16.0) | 3.0 (1.8–5.1)*** | 51 (11.6) | 0.9 (0.6–1.4) | 48 (11.0) | 1.5 (0.9–2.4) | 253 (57.8) | 0.7 (0.5–0.9)** | 122 (28.0) | 1.4 (1.0–2.0)* |
| 25–29 | 21 (6.1) | REF | 54 (13.0) | REF | 33 (8.0) | REF | 285 (68.7) | REF | 86 (20.8) | REF |
| SexualityC | ||||||||||
| Heterosexual | 147 (20.0) | REF | 171 (18.5) | REF | 187 (20.3) | REF | 532 (57.8) | REF | 346 (37.7) | REF |
| Gay/lesbian | 54 (21.8) | 1.3 (0.9–1.9) | 54 (18.1) | 1.1 (0.8–1.7) | 64 (21.5) | 1.3 (0.9–1.9) | 167 (56.0) | 0.9 (0.6–1.2) | 121 (40.7) | 1.2 (0.9–1.6) |
| Bi/pansexual | 106 (21.5) | 1.1 (0.8–1.5) | 101 (17.1) | 0.9 (0.7–1.2) | 122 (20.7) | 1.0 (0.8–1.3) | 319 (54.1) | 0.9 (0.8–1.2) | 246 (41.7) | 1.1 (0.9–1.4) |
| Something else | 12 (17.1) | 0.7 (0.4–1.5) | 12 (13.3) | 0.8 (0.6–1.4) | 16 (17.8) | 0.9 (0.5–1.6) | 40 (44.4) | 0.7 (0.4–1.1) | 39 (43.3) | 1.0 (0.6–1.6) |
| Aboriginal and/or Torres Strait Islander | ||||||||||
| No | 302 (20.1) | – | 323 (17.5) | – | 372 (20.1) | – | 1036 (56.1) | – | 723 (39.2) | – |
| Yes | 14 (30.4) | – | 11 (20.8) | – | 15 (28.3) | – | 25 (47.2) | – | 25 (47.2) | – |
| Country of birth | ||||||||||
| Australia | 264 (20.6) | – | 269 (17.4) | REF | 311 (20.1) | – | 866 (55.9) | – | 614 (39.7) | – |
| Overseas, >5 years in Australia | 37 (20.6) | – | 52 (23.0) | 1.4 (1.0–1.9) | 51 (22.7) | – | 126 (56.0) | – | 86 (38.2) | – |
| Overseas, ≤5 years in Australia | 14 (18.0) | – | 15 (12.9) | 0.8 (0.4–1.5) | 24 (20.7) | – | 61 (52.6) | – | 44 (37.9) | – |
| Lives in major city | ||||||||||
| Yes | 264 (20.3) | – | 285 (18.0) | – | 316 (19.9) | – | 879 (55.5) | – | 617 (39.0) | – |
| No | 51 (21.6) | – | 49 (16.3) | – | 68 (22.7) | – | 172 (57.3) | – | 130 (43.3) | – |
| Sexually activeD | ||||||||||
| No | 98 (32.1) | REF | 70 (17.1) | REF | 103 (25.2) | REF | 191 (46.7) | REF | 225 (55.2) | REF |
| Yes | 221 (17.7) | 0.7 (0.5–0.9)* | 268 (17.8) | 1.4 (1.0–2.0)* | 286 (19.1) | 1.1 (0.8–1.5) | 874 (58.3) | 1.2 (1.0–1.6) | 529 (35.3) | 0.7 (0.5–0.9)** |
| Sex educationE | ||||||||||
| No/unsure | 53 (26.7) | REF | 64 (24.6) | REF | 74 (28.6) | REF | 123 (47.5) | REF | 119 (46.0) | REF |
| Yes | 268 (19.7) | 0.6 (0.4–0.9)* | 275 (16.6) | 0.6 (0.4–0.9)** | 317 (19.2) | 0.5 (0.4–0.7)*** | 943 (57.1) | 1.5 (1.1–2.0)** | 637 (38.6) | 0.7 (0.5–0.9)** |
| Usual GP | ||||||||||
| No | N/A | N/A | 109 (17.2) | – | 157 (24.8) | REF | 299 (47.3) | REF | 271 (43.0) | REF |
| Yes | N/A | N/A | 229 (17.9) | – | 234 (18.3) | 0.7 (0.5–0.9)** | 767 (60.0) | 1.8 (1.4–2.2)*** | 485 (38.0) | 0.8 (0.6–1.0)* |
REF, reference category.
*** <0.001, ** <0.01, * <0.05.
AOnly includes participants who said they have a usual GP.
BParticipants could select multiple gender identities. ‘Trans and gender diverse’ people includes respondents who said they were transgender and/or selected agender, non-binary, genderfluid/genderqueer or self-described their gender and did not also select ‘man’ or ‘woman’.
CParticipants could select multiple sexuality options. Those who selected ‘queer’ only were included with gay/lesbian respondents unless they also selected bisexual or pansexual. ‘Something else’ includes asexual and questioning or unsure men and women who did not select another sexuality
DReported any partnered sexual activity (including vaginal, anal and oral sex, as well as any other sexual contact with another person).
ESchool-based sex education, those who could not remember were included with ‘no’.
Statement 1: I would be too embarrassed to see my usual GP if I thought I had an STI
Of the 1558 participants who reported having a usual GP, 321 (20.6%, 95% CI 18.6–22.7%) agreed that they would be too embarrassed to see them if they thought they had an STI. From multivariate analysis, we found that younger age groups were more likely to agree with this statement when compared with the oldest age group (16–17 years aOR 7.1, 95% CI 4.3–11.8; 18–20 years aOR 4.1, 95% CI 2.4–7.0; 21–24 years aOR 3.0, 95% CI 1.8–5.1). Respondents who had received a school-based sex education and who had any history of partnered sexual activity were less likely to agree with Statement 1 (aOR 0.6, 95% CI 0.4–0.9 and aOR 0.7, 95% CI 0.5–0.9, respectively).
Statement 2: If a GP asked about my sexual history, I might not tell them the whole truth
A total of 339 of 1915 (17.7%, 95% CI 16.0–19.5%) respondents said they might not disclose the whole of their sexual history to a GP. Those in the two youngest age groups were more likely to agree with Statement 2 when compared with the oldest age group (16–17 years aOR 2.6, 95% CI 1.8–3.8; 18–20 years aOR 1.6, 95% CI 1.0–2.3). Sexually active respondents also were more likely to agree with this statement (aOR 1.4, 95% CI 1.0–2.0), and those who had received a school-based sex education were less likely to agree with Statement 2 (aOR 0.6, 95% CI 0.4–0.9).
Statement 3: I would be worried about confidentially when discussing my sexual history with a GP.
A total of 391 of 1913 (20.4%, 95% CI 18.7–22.3%) respondents agreed that they would be concerned about confidentiality when discussing their sexual history with a GP. Those in the two youngest age groups were more likely to agree with this statement, when compared with the oldest age group (16–17 years aOR 7.4, 95% CI 4.8–11.2; 18–20 years aOR 3.4, 95% CI 2.2–5.4). Those who had received a school-based sex education and those with a usual GP were less likely to agree with this statement (aOR 0.5, 95% CI 0.4–0.7 and aOR 0.7, 95% CI 0.5–0.9, respectively).
Statement 4: I would be OK with a GP asking me about my sexual health if I was seeing them for an unrelated reason.
Over half (1066/1912; 55.8%, 95% CI 53.5–58.0%) of respondents agreed that they would be OK with a GP bringing up their sexual health in an unrelated consultation, and just under one-third (30.4%, 95% CI 28.3–32.5%) were neutral or unsure about their agreement with this statement. Younger age groups were less likely to agree with this statement than the oldest age group (16–17 years aOR 0.4, 95% CI 0.3–0.6; 18–20 years aOR 0.5, 95% CI 0.4–0.7; 21–24 years aOR 0.7, 95% CI 0.5–0.9). Male respondents were more likely to agree with Statement 4, compared with female respondents (aOR 1.5, 95% CI 1.2–1.9). Those who had received a school-based sex education and those with a usual GP were more likely to agree with this statement (aOR 1.5, 95% CI 1.1–2.0 and aOR 1.8, 95% CI 1.4–2.2, respectively).
Statement 5: I would be nervous about bringing up sexual health with a GP in case I needed to have an intimate examination or test.
A total of 756 of 1909 (39.6%, 95% CI 37.4–41.8%) respondents agreed that they would be nervous about bringing up their sexual health with a GP in case they needed an intimate examination. All younger age groups were more likely to agree with this statement when compared with the oldest age group (16–17 years aOR 4.5, 95% CI 3.3–6.1; 18–20 years aOR 2.8, 95% CI 2.1–3.9; 21–24 years aOR 1.4, 95% CI 1.0–2.0). Those who were sexually active, those with a school-based sex education and those with a usual GP all were less likely to agree with Statement 5 (aOR 0.7, 95% CI 0.5–0.9, aOR 0.7, 95% CI 0.5–0.9 and aOR 0.8, 95% CI 0.6–0.1, respectively).
Discussion
In this survey of young Australians, we found that young people generally appeared to be receptive to discussing their sexual health with a GP. Most indicated they would be comfortable for a GP to initiate discussions about sexual health, to see their usual GP if they thought they had an STI and that they trusted their GP in respect to confidentiality in discussing sexual health matters. However, the prospect of sensitive examinations was a barrier to raising sexual health concerns, with a significant amount of respondents agreeing they would be nervous to initiate discussions about sexual health in case they needed to have an intimate examination or test. Respondents with a usual GP or who had received school sex education were more likely to be more receptive to discussing sexual health with a GP.
Our analysis identified that receptiveness to discussing sexual health with a GP was strongly associated with age. We found a clear trend, whereby the younger the survey participants were, the more likely they were to have reservations about discussing their sexual health, whether it was raised by themselves or their GP. For example, whereas only 8% of 25–29-year-olds indicated they were concerned about confidentiality when discussing sexual health with a GP, 35% of 16–17-year-olds said they were concerned about this. In addition, a higher proportion of the youngest respondents than the oldest respondent (57% vs 21%) indicated they would be nervous to bring up sexual health in case they needed an intimate examination. In Australia, people from the age of 15 years can access their own Medicare card, and under 18s are able to consent for medical treatment in some circumstances, provided the medical practitioner is satisfied that they are a ‘mature minor’ and have capacity to do so (Bird 2011). We found that those with a usual GP and those who had received a school-based sex education were less likely to be apprehensive about intimate examinations or concerned about their confidentiality, which may indicate that health promotion through school programs and individual health care providers can provide young people with reassurance about their rights when accessing care for sensitive issues.
Interestingly, we found few differences between responses from young men and women. The main exception was that male respondents were more likely than female respondents to say they would be OK with a GP bringing up their sexual health in an unrelated consultation. Health care access differs by gender. In Australia, men of all ages are reported to visit a GP less frequently than women (AIHW 2022), and a recent review of men’s help-seeking behaviours and engagement with general practice highlighted that men – particularly younger men – tend to visit a GP when they have an acute issue, rather than viewing general practice as a source of preventative health care (Mursa et al. 2022). Meanwhile, reproductive responsibilities continue to lie primarily with women (Caddy et al. 2023), many of whom will visit a GP for advice on contraception (providing opportunities for GPs to discuss other sexual health issues). As such, it is possible that our female participants consider these sexual health-related consultations as a more appropriate time to discuss sexual health, whereas men – who do not tend to have such opportunities – are more open to their sexual health being raised in unrelated consultations. Nevertheless, most female respondents still considered it acceptable for a GP to raise their sexual health in an unrelated consultation, and GPs may be reassured that most young people are open to these discussions. To support GPs to raise and discuss sexual health with young patients, there is a range of professional development material available throughout Australia (NWMPHN, n.d.; RACGP 2022).
Importantly, our findings highlight the positive impact that a school-based sex education can have on young people’s sexual health. We found this to be associated with a higher level of receptiveness to discussing sexual health with a GP. There is evidence that school-based sex education programs improve health outcomes and attitudes towards sexual and reproductive health, and increase knowledge (UNESCO 2016). In Australia, relationships and sexuality education is covered in the Health and Physical Education learning area of the national curriculum (ACARA, n.d.). However, some areas for improvement have been identified in Australian school-based sex education programs. In a recent survey, Australian secondary school students generally disclosed negative experiences of school sex education programs, citing (among other things) poor content, delivery and timing of education programs (Waling et al. 2020). Many students highlighted that they would like school sex education programs to contain more information about a number of factors, including safer sex practices, and specifically information about the transmission of and risk of STIs and HIV (Waling et al. 2021). Furthermore, recommendations from a survey of Australian teachers of sexuality education include a need for further training for teachers that focuses on the current curriculum, as well as gender, sexual diversity and sexual behaviours (areas that teachers are less comfortable teaching; Ezer et al. 2020). Our findings emphasise the importance of providing young people with a school-based sex education, and support recommendations to optimise program delivery when necessary.
Furthermore, our findings reveal that having an established clinical relationship with a GP can positively impact young people’s sexual health, with those reporting a usual GP having a higher receptivity to discussing sexual health. Our findings support the existing literature that has demonstrated the benefits that an ongoing patient–doctor relationship and continuity of care can have on patient experience and outcomes (Jackson and Ball 2018). However, we also acknowledge that regarding sexual health, patient preferences may vary. For example, existing research has identified that although many young Australians would like STI testing to be conducted by their usual GP, others have expressed a preference to access testing through a different GP or specialist sexual health service (Kang et al. 2014). Therefore, although our findings highlight the important role that an ongoing relationship with a GP can play for young people, we note that it is important for young people to have the option to access sexual health care via a new or unknown provider, if preferred.
Finally, we found that neither sexuality nor diverse gender identity were associated with receptiveness to discussing sexual health with GPs. Given the large body of evidence that has found LGBTQI+ people experience discrimination and stigma when discussing sexual health with GPs (Alencar Albuquerque et al. 2016; Brooks et al. 2018; Ayhan et al. 2020), this was an unexpected finding. We had anticipated that we may find young LGBTQI+ participants to be less receptive to discussing their sexual health with a GP and more likely to have concerns about their confidentiality or about revealing their sexual history to GPs. We are unsure why we did not find an association, although we note that there were few transgender and gender diverse respondents, limiting the power to detect a statistically significant association for this group. Although our findings may suggest that there has been some progression towards reducing stigma and discrimination towards young LGBTQI+ people in primary health care, we interpret this with caution, taking into consideration that young people who respond to an online sexual health survey may be more open to discussing their sexual health.
Our study utilised a convenience sample, which enabled quick and cost-effective recruitment, and resulted in a large sample size. However, the generalisability of our findings to the general population is limited by utilising this study design. In particular, there was an overrepresentation of female respondents, people residing in major cities and LGBTQI+ young people. By recruiting via social media, and developing the survey in English only, we also acknowledge that some population groups with lower levels of English literacy or access to the internet and/or social media will not be well-represented in this survey. This is an important exclusion to note, as these groups experience barriers to accessing health care, and may have different perspectives on discussing sexual health in general practice.
A further limitation of this study relates to survey respondents’ interpretations of ‘sexual health’, as we did not define this within the survey tool. Although questions about many aspects of young people’s sexual and reproductive health were included within the survey, this question followed a question relating to which services respondents might access for STI testing. It is therefore not possible to determine how respondents interpreted ‘sexual health’ here, and whether they viewed this as relating to STI testing only, or whether they considered this term more broadly.
Conclusions
Reassuringly, young people appeared to be largely receptive to having open and honest discussions about their sexual health with a GP, and most would be accepting of a GP raising their sexual health in an unrelated consultation. However, a substantial number of young people were apprehensive about physical examinations, and this may be a barrier to young people raising their sexual health with GPs independently. Notably, we identified two important factors that were supportive of sexual health discussions with GPs: an ongoing GP–patient relationship (i.e. ‘usual GP’) and having received a school-based sex education. Our findings, therefore, highlight the importance of routine primary care for young people, and support the existing literature that demonstrates the usefulness and importance of a school-based sex education in regard to young people’s sexual health.
Data availability
The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research, supporting data is not available.
References
Alencar Albuquerque G, de Lima Garcia C, da Silva Quirino G, Alves MJH, Belém JM, dos Santos Figueiredo FW, da Silva Paiva L, do Nascimento VB, da Silva Maciel É, Valenti VE, de Abreu LC, Adami F (2016) Access to health services by lesbian, gay, bisexual, and transgender persons: systematic literature review. BMC International Health and Human Rights 16, 2.
| Crossref | Google Scholar |
Australian Curriculum Assessment and Reporting Authority (ACARA) (n.d.) Health and physical education. Sydney, Australia. Available at https://www.australiancurriculum.edu.au/f-10-curriculum/health-and-physical-education/ [Accessed 16 March 2023]
Australian Institute of Health and Welfare (AIHW) (2022) General practice, allied health, and other primary care services. Available at https://www.aihw.gov.au/reports/health-care-quality-performance/general-practice-allied-health-and-other-primary-c [Accessed 30 January 2023]
Australasian Sexual Health Alliance (2022) Australian STI management guidelines for use in primary care. ASHM. Available at https://sti.guidelines.org.au/standard-asymptomatic-checkup/ [Accessed 18 May 2023]
Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S (2020) A Systematic review of the discrimination against sexual and gender minority in health care settings. International Journal of Health Services 50, 44-61.
| Crossref | Google Scholar |
Baker JR, Arnold-Reed DE, Brett T, Hince DA, O’Ferrall I, Bulsara MK (2013) Perceptions of barriers to discussing and testing for sexually transmitted infections in a convenience sample of general practice patients. Australian Journal of Primary Health 19, 98-101.
| Crossref | Google Scholar |
Bateson D, Edmiston N (2016) Pelvic inflammatory disease: management of new-onset low abdominal pain in young women. Medicine Today 17, 14-22.
| Google Scholar |
Bird S (2011) Consent to medical treatment: the mature minor. Australian Family Physician 40, 159-160.
| Google Scholar |
Brooks H, Llewellyn CD, Nadarzynski T, Pelloso FC, De Souza Guilherme F, Pollard A, Jones CJ (2018) Sexual orientation disclosure in health care: a systematic review. British Journal of General Practice 68, e187-e196.
| Crossref | Google Scholar |
Caddy C, Temple-Smith M, Coombe J (2023) Who does what? Reproductive responsibilities between heterosexual partners. Culture, Health & Sexuality
| Crossref | Google Scholar |
Collyer A, Bourke S, Temple-Smith M (2018) General practitioners’ perspectives on promoting sexual health to young men. Australian Journal for General Practitioners 47, 376-381.
| Crossref | Google Scholar |
Fairley CK, Chow EPF, Simms I, Hocking JS, Ong JJ (2022) Accessible health care is critical to the effective control of sexually transmitted infections. Sexual Health 19, 255-264.
| Crossref | Google Scholar |
Genc M (2000) Syphilis in pregnancy. Sexually Transmitted Infections 76, 73-79.
| Crossref | Google Scholar |
Gott M, Galena E, Hinchcliff S, Elford H (2004) “Opening a can of worms”: GP and practice nurse barriers to talking about sexual health in primary care. Family Practice 21, 528-536.
| Crossref | Google Scholar |
Harris ML, Coombe J, Forder PM, Lucke JC, Bateson D, Loxton D (2020) Young women’s complex patterns of contraceptive use: findings from an Australian Cohort Study. Perspectives on Sexual and Reproductive Health 52, 181-190.
| Crossref | Google Scholar |
Hook EW, 3rd (2017) Syphilis. The Lancet 389, 1550-1557.
| Crossref | Google Scholar |
Hoopes AJ, Benson SK, Howard HB, Morrison DM, Ko LK, Shafii T (2017) Adolescent perspectives on patient-provider sexual health communication: a qualitative study. Journal of Primary Care & Community Health 8, 332-337.
| Crossref | Google Scholar |
Jackson C, Ball L (2018) Continuity of care: vital, but how do we measure and promote it? Australian Journal for General Practitioners 47, 662-664.
| Crossref | Google Scholar |
Kang M, Rochford A, Skinner SR, Mindel A, Webb M, Peat J, Usherwood T (2014) Sexual behaviour, sexually transmitted infections and attitudes to chlamydia testing among a unique national sample of young Australians: baseline data from a randomised controlled trial. BMC Public Health 14, 12.
| Crossref | Google Scholar |
Kularadhan V, Fairley CK, Chen M, Bilardi J, Fortune R, Chow EPF, Philips T, Ong JJ (2022) Optimising the delivery of sexual health services in Australia: a qualitative study. Sexual Health 19, 376-385.
| Crossref | Google Scholar |
Mitchell KR, Lewis R, O’Sullivan LF, Fortenberry JD (2021) What is sexual wellbeing and why does it matter for public health? The Lancet Public Health 6, e608-e613.
| Crossref | Google Scholar |
Moreau C, Kågesten AE, Blum RW (2016) Sexual dysfunction among youth: an overlooked sexual health concern. BMC Public Health 16, 1170.
| Crossref | Google Scholar |
Mursa R, Patterson C, Halcomb E (2022) Men’s help-seeking and engagement with general practice: An integrative review. Journal of Advanced Nursing 78, 1938-1953.
| Crossref | Google Scholar |
North Western Melbourne Primary Health Network (NWMPHN) (n.d.) VHHITAL. Available at https://nwmphn.org.au/about/partnerships-collaborations/vhhital/ [Accessed 23 June 2023]
Ong JJ, Fairley CK, Fortune R, Bissessor M, Maloney C, Williams H, Castro A, Castro L, Wu J, Lee PS, Chow EPF, Chen MY (2022) Improving access to sexual health services in general practice using a hub-and-spoke model: a mixed-methods evaluation. International Journal of Environmental Research and Public Health 19, 3935.
| Crossref | Google Scholar |
Pavlin NL, Parker R, Fairley CK, Gunn JM, Hocking J (2008) Take the sex out of STI screening! Views of young women on implementing chlamydia screening in general practice. BMC Infectious Diseases 8, 62.
| Crossref | Google Scholar |
RACGP (2022) 2022 RACGP curriculum and syllabus for Australian general practice: sexual health and gender diversity. Royal Australian College of General Practitioners. Available at https://www.racgp.org.au/education/education-providers/curriculum/curriculum-and-syllabus/units/sexual-health-and-gender-diversity [Accessed 23 June 2023]
Rowe H, Holton S, Kirkman M, Bayly C, Jordan L, McNamee K, Mcbain J, Sinnott V, Fisher J (2016) Prevalence and distribution of unintended pregnancy: the Understanding Fertility Management in Australia National Survey. Australian and New Zealand Journal of Public Health 40, 104-109.
| Crossref | Google Scholar |
Schlichthorst M, Sanci LA, Hocking JS (2016) Health and lifestyle factors associated with sexual difficulties in men – results from a study of Australian men aged 18 to 55 years. BMC Public Health 16, 1043.
| Crossref | Google Scholar |
Waling A, Bellamy R, Ezer P, Kerr L, Lucke J, Fisher C (2020) ‘It’s kinda bad, honestly’: Australian students’ experiences of relationships and sexuality education. Health Education Research 35, 538-552.
| Crossref | Google Scholar |
Waling A, Fisher C, Ezer P, Kerr L, Bellamy R, Lucke J (2021) “Please teach students that sex is a healthy part of growing up”: Australian students’ desires for relationships and sexuality education. Sexuality Research and Social Policy 18, 1113-1128.
| Crossref | Google Scholar |
WHO (2006) Sexual and reproductive health and research. World Health Organisation. Available at https://www.who.int/teams/sexual-and-reproductive-health-and-research/key-areas-of-work/sexual-health/defining-sexual-health [Accessed 18 May 2023]
Zannoni R, Dobberkau E, Kaduszkiewicz H, Stirn AV (2021) Addressing sexual problems in German primary care: a qualitative study. Journal of Primary Care & Community Health 12, 215013272110464.
| Crossref | Google Scholar |


