Co-designing a Health Journey Mapping resource for culturally safe health care with and for First Nations people
Alyssa Cormick A * , Amy Graham A , Tahlee Stevenson A , Kelli Owen A , Kim O’Donnell A B and Janet Kelly AA
B
Abstract
Many healthcare professionals and services strive to improve cultural safety of care for Australia’s First Nations people. However, they work within established systems and structures that do not reliably meet diverse health care needs nor reflect culturally safe paradigms. Journey mapping approaches can improve understanding of patient/client healthcare priorities and care delivery challenges from healthcare professionals’ perspectives leading to improved responses that address discriminatory practices and institutional racism. This project aimed to review accessibility and usability of the existing Managing Two Worlds Together (MTWT) patient journey mapping tools and resources, and develop new Health Journey Mapping (HJM) tools and resources.
Four repeated cycles of collaborative participatory action research were undertaken using repeated cycles of look and listen, think and discuss, take action together. A literature search and survey were conducted to review accessibility and usability of MTWT tools and resources. First Nations patients and families, and First Nations and non-First Nations researchers, hospital and university educators and healthcare professionals (end users), reviewed and tested HJM prototypes, shaping design, format and focus.
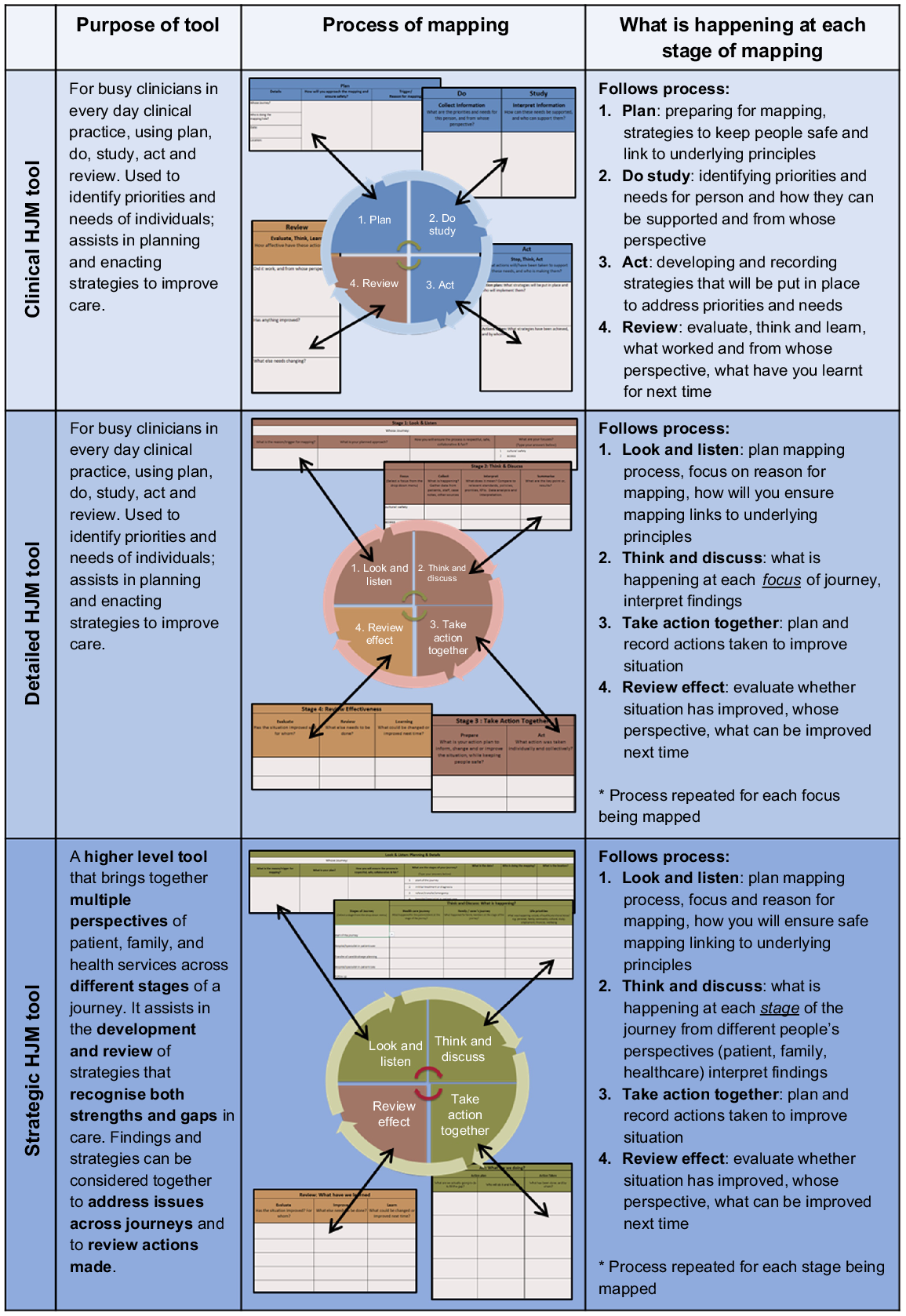
The MTWT tool and resources have been used across multiple health care, research and education settings. However, many users experienced initial difficulty engaging with the tool and offered suggested improvements in design and usability. End user feedback on HJM prototypes identified the need for three distinct mapping tools for three different purposes: clinical care, detailed care planning and strategic mapping, to be accompanied by comprehensive resource materials, instructional guides, videos and case study examples. These were linked to continuous quality improvement and accreditation standards to enhance uptake in healthcare settings.
The new HJM tools and resources effectively map diverse journeys and assist recognition and application of strengths-based, holistic and culturally safe approaches to health care.
Keywords: Aboriginal and/or Torres Strait Islander health care, co-design in participatory action research, continuous quality and improvement, cultural safety, decolonising First Nations health care, Health Journey Mapping, patient centred care, Patient Journey Mapping.
Introduction
Changes in the way health care is provided for and with First Nations peoples
Increasingly, healthcare services, professionals and accreditation processes are recognising that Australia’s biomedically focused healthcare system does not adequately consider, nor meet the health and wellbeing needs of, First Nations people (Aboriginal and/or Torres Strait Islander peoples) (Yashadhana et al. 2021). Historically, Australian health services and structures have been built upon the priorities and worldviews of the ‘Eurocentric majority’, excluding specific health and wellbeing needs of First Nations people (Gatwiri et al. 2021). Targeted work is therefore needed to address the deeply entrenched discrimination and racism within our healthcare systems (Nolan-Isles et al. 2021).
There is increasing recognition that the provision of culturally safe and responsive care requires systems level changes, as well as professional and interpersonal level changes, informed by First Nations people (Wilson et al. 2020). Healthcare services and workers uphold standards to protect the public from harm and improve quality of care. In Australia, these include specific national standards relating to culturally safe care for First Nations people, as defined by health systems (ACSQHC 2017) and healthcare disciplines (AHPRA 2020).
Culturally safe care requires shared respect and knowledge, deep listening, removal of barriers, acknowledgement of cultural differences, reflecting on one’s own assumptions and prejudices and appreciation that the same care is not always appropriate for, or responsive to, the needs of different individuals (Mackean et al. 2020). A therapeutic culturally safe relationship identifies and responds to the individual healthcare needs of each patient or client, resulting in co-designed care that is perceived as safe by the recipient of care (Gollan and Stacey 2021).
Healthcare professionals and health services can respond to ongoing gaps and needs in everyday practice by engaging in two-way communication, building and maintaining respectful relationships, critically reflecting on their practice and unconscious biases, acknowledging the impact of history and colonisation and supporting First Nations healthcare professionals (Mackean et al. 2020; Fisher et al. 2021). Creating culturally safe environments and practicing in a culturally safe manner is an ongoing learning and reflective process as individuals strengthen their knowledge and understanding by listening to recipients of care and reflecting on their own practice (ACSQHC 2017; Gollan and Stacey 2021). While this is often difficult to achieve in busy clinical settings, journey mapping can assist in providing structural frameworks for enacting, embedding and evaluating cultural safety.
Journey mapping
Journey mapping is a method of describing and recording different stages of patients/clients’ healthcare interactions, enabling assessment of strengths and gaps in care (Fraser et al. 2021). Mapping illustrates patient experiences and allows gaps to be identified from the perspectives of patients, families and healthcare providers (Joseph et al. 2020). The resulting information or ‘journey maps’ may be compared with, and evaluated against, existing guidelines, standards and models of care for continuous quality improvement (Fraser et al. 2021). The development and use of journey mapping in health care has increased over the past decade (Davies et al. 2022). However, as this is an emerging field of practice, there is currently no consistency in methodology or reporting on use and effectiveness of journey mapping, highlighting the need for clearer methodologies and reporting guidelines (Joseph et al. 2020; Davies et al. 2022).
Co-designing mapping tools
Between 2008 and 2015, the Managing Two Worlds Together (MTWT) research project was undertaken to identify and address the challenges that many Aboriginal people living in rural and remote areas of South Australia and Northern Territory face throughout their health care journeys to and from Adelaide city hospitals (The Lowitja Institute 2015; Kelly et al. 2017). The research team interviewed First Nations patients and family members undergoing health journeys, and the healthcare professionals in rural, remote and metropolitan health services. At the time the team identified there were no existing tools to identify different dimensions of health that included factors impacting access and quality of care, and multiple perspectives from patients, families and health professionals. The team therefore co-designed patient journey mapping tools with First Nations patients, families and health professionals, and non-First Nations health professionals who were research participants, resulting in the development of the MTWT mapping tool, a workbook and series of case study reports published by the Lowitja Institute (The Lowitja Institute 2015; Kelly et al. 2017). These resources identified ways of mapping barriers and enablers of care and developing responsive strategies.
In 2020 members of the MTWT research team sought to evaluate the effectiveness of the MTWT patient journey mapping tools in practice, and determine if there was a need to update or co-design new tools. They approached the Lowitja Institute who funded a review of citations and evaluation of effectiveness by people who had used the tools, and then a project to co-design and pilot a new set of Health Journey Mapping (HJM) tools. This research project was conducted in collaboration with members of the Aboriginal Kidney Care Improving Outcomes Now (AKction) Research project, a First Nations led project at the University of Adelaide, Adelaide Nursing School. This paper reports on the citation review, evaluation and co-design of three new HJM tools and education resources. The overall aim of this project was to review accessibility and usability of the MTWT patient journey mapping tool and resources, and develop new HJM tools and resources.
Method
A cyclical participatory action research (PAR) and co-design approach was used by the research team with First Nations patients and families, and First Nations and non-First Nations researchers, hospital and university educators and healthcare professionals (end users). Together they reviewed the effectiveness of the original MTWT tool and developed new tools and resources that responded to their individual and collective priorities and needs. Research was conducted with health professionals and health service educators in mainstream health services and Aboriginal Community Controlled Health services in metropolitan, rural and remote areas, with university educators in university settings and with First Nations community members in university and community settings.
PAR provides a reflective and action focused approach, enabling development of effective solutions by situating participants as experts to identify and address the problems they face (Stringer and Aragon 2021). End users were invited to collaborate in the cyclical decolonising PAR processes of look and listen, think and discuss, take action and review effectiveness (Kelly 2008). This process enabled end users to continuously inform development and evaluation, ensure First Nations definitions of health and wellbeing were continually reinforced and ensure that each iteration of the tools and resources responded to diverse end users’ unique needs. Co-design approaches are used to identify and resolve issues through collaboration with end users (Butler et al. 2022). This project applied an iterative decolonising co-design approach, where end users’ expertise identified the need and informed development of new mapping tools and resources. This co-design approach was underpinned by concepts of cultural safety, reciprocity, compassion, collaboration, empowerment and trust (Chamberlain et al. 2019).
As shown in Fig. 1, the project involved four PAR cycles: (phases 1a and 1b) reviewing the use of the original MTWT mapping tool and resources; (phase 2) co-designing the new HJM tools, education material and worked examples; and (phase 3) testing and piloting the final HJM resource with end users.
Overview of the HJM project, explaining co-design processes, PAR activities and results of each research phase. HJM, Health Journey Mapping; PAR, participatory action research; MTWT, Managing Two Worlds Together; PPTs, PowerPoints.
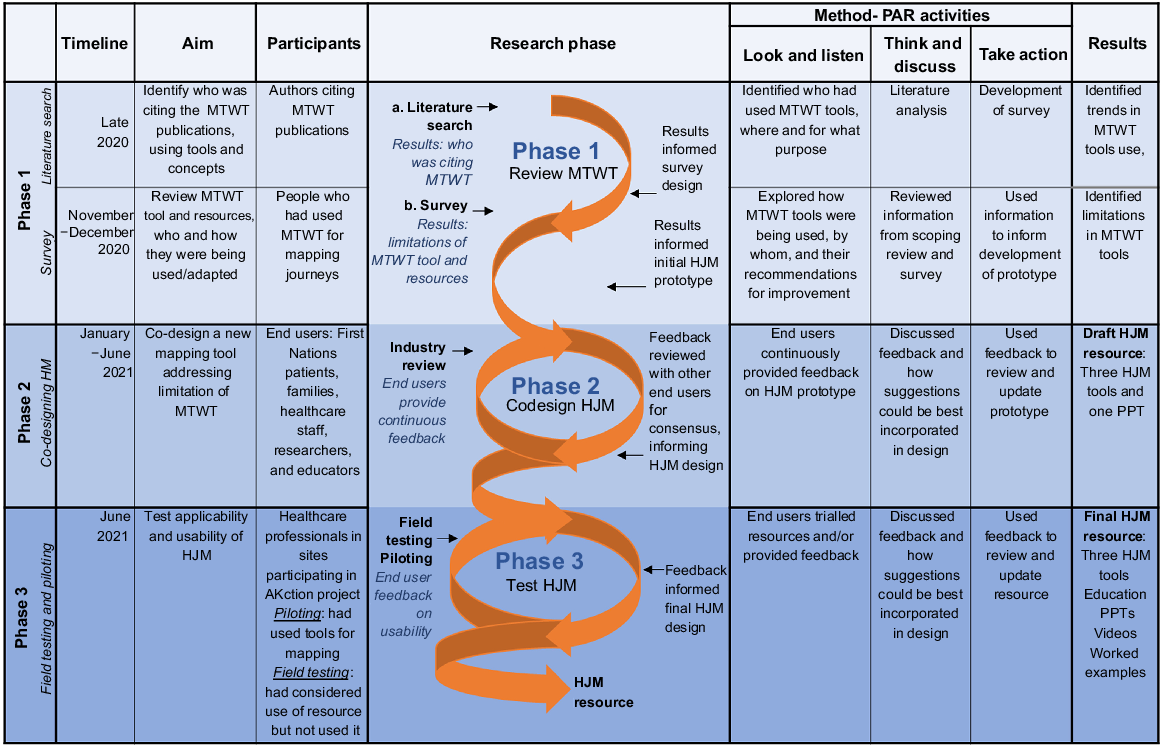
Phase 1a. Literature search
Phase 1a aimed to review citations of the MTWT patient journey mapping tool, identifying who had used the tool and concepts, for what purpose and to what extent.
An online literature and document search for citations of MTWT publications was conducted in late 2020 using Google Scholar. Google Scholar was chosen to capture a wider range of sources including grey literature. Citations were collated, deductively analysed and presented in tables to identify the type and location of publication, the purpose and extent of mapping.
Phase 1b. Survey
Phase 1b aimed to review how the MTWT tool had been used since inception and determine how the tools had been accessed, used, adapted and/or updated, and garner suggestions for improvement.
Potential participants were identified through the literature search and MTWT team members relational and collegial networks. This included people who had contacted the MTWT team about using the tool but had not yet completed or published their research. Inclusion criteria for involvement was that participants had used or adapted the MTWT tool to map a journey. Potential participants were from six main groups: health professionals from urban rural and remote locations; Canadian researchers who had begun using the tool; individual researchers and research projects including non-government organisations and Aboriginal Community Controlled Health organisations; university academics; higher degree students; and members of the original MTWT research team. Seventy seven individuals were emailed and invited to complete the survey. Nineteen people completed the survey, four of whom identified as First Nations. Ten potential participants responded that they were unable or ineligible to complete the survey because they had significantly increased workload due to the COVID-19 pandemic or had not yet used the MTWT tool.
An online Survey Monkey questionnaire was sent to 77 potential participants, comprising 35 questions covering ten areas: demographics; discovery of and decision to use the tools; application and use of the tools; ease and adaptability; linking to standards; methodological approaches; what journey mapping enabled users to achieve; evaluation of the tools; use in education; and suggestions moving forward. Potential study participants were contacted via email, informed of the project and invited to participate in the online survey. If interested, a participant information form and a link to the online survey was provided via email. Survey responses were collated; qualitative data were analysed using simple descriptive analysis, and quantitative data were presented in tables and graphs within Survey Monkey and analysed by identifying trends in usage.
Phase 2. End user industry review and co-design
Phase 2 aimed to co-design new journey mapping tools and education materials that addressed limitations of the original MTWT tool and resources.
Participants or end users were First Nations patients and family members, and First Nations and non-First Nations healthcare professionals, researchers and educators. Potential participants were identified through existing healthcare, research, and education networks of the AKction research project and invited to be involved in the project. Of those invited, 30 participants participated in the industry review and co-design phase. Seven of the participants identified as First Nations.
An initial prototype was developed using findings and recommendations from the literature search and survey results. The prototype consisted of one mapping tool and an educational Power Point focusing on topics of importance identified by end users. These included the underlying principles of cultural safety, equity, partnership and continuous quality improvement, with instructions on how to use the tools. This prototype was shared and discussed with end users.
A First Nations informed, collaborative decision-making and PAR process was then applied, enabling iterations of the resource to be continuously reviewed and updated in response to ongoing discussion and feedback loops from end users. Look and listen: potential participants were contacted by the research team and invited to be involved in the research project. The prototype was shared with interested participants, who then individually provided feedback to the research team in person, via videoconferencing, phone or email. Think and discuss: feedback from participants was reviewed weekly in collaborative meetings by involving both First Nations and non-First Nations research team members. Emerging ideas and suggestions were inductively analysed thematically in Word documents, then discussed in the next round with end users to gain consensus. Take action: the prototype and accompanying resources were continually adapted by end user recommendations. Review effectiveness: the final prototypes were shared with end users for review (Kelly 2008). This process was repeated for several months, as different participants engaged with the project and provided their feedback on different iterations of the prototype and resources. The Lowitja Institute was also involved in these conversations, identifying focus and goals for the project from a First Nations research institute perspective.
Phase 3. Field testing and piloting to review resource
Phase 3 aimed to test the applicability and useability of the new HJM resources (tools, education materials and worked examples).
Participants were First Nations and non-First Nations healthcare professionals and managers within healthcare sites already participating in the AKction project, where patient journey mapping activities were being established and covered by existing ethics approvals. Potential participants were identified through their involvement in the AKction project. Piloting participants were required to actively use the HJM tools for mapping, while field testing participants were required to have considered using the resource for mapping. Five participants field tested, and five participants piloted the tools. Two of the participants who piloted the tools identified as First Nations.
Due to the short timeframe of this project and increased demands from the COVID-19 pandemic impacting healthcare professionals’ capacity, field testing and piloting occurred concurrently. This enabled participants who were unable to actively use the tools to also provide feedback on near final versions based on what would work best in their worksite. Interested participants were sent a prototype of the tools via email and provided feedback in person, via videoconferencing, phone or email. Piloting occurred in AKction research sites with healthcare professionals actively using the tools for mapping journeys of First Nations kidney patients. These participants provided feedback in person, via videoconferencing, phone or email which was then collated and inductively thematically analysed in Word documents. Input from field testing and piloting informed changes to the final resource.
Ethics approval
Ethics approval for the Health Journey Mapping project was provided by the Aboriginal Health Council of South Australia, AHREC Protocol #04-20-896. This project was conducted in collaboration with the AKction project that received ethical approval from the Aboriginal Health Council of South Australia, AHREC Protocol # 04-22-944, the Central Adelaide Local Health Network Human Research Ethics Committee (HREC reference number: HREC/19/CAHLN/45, CAHLN reference number: R20190124) and the University of Adelaide Research Ethics Committee (UoA ID 33394). This project was conducted according to the NHMRC National Statement on Ethical Conduct in Human Research.
Results
Phase 1a. Literature search
There were 20 pieces of work published by the MTWT project; including six peer reviewed journal articles, two project reports, two workbooks and 10 case study reports. Of these, 14 were cited in 73 published works. These publications included 58 peer reviewed articles, nine PhD theses, two reports, two conference papers and two textbook chapters. Sixty-two of these publications were from Australia, three from Canada, two from the United States of America and one each from the United Kingdom, the Netherlands, Germany, Pakistan, the Maldives and Italy (see Supplementary data).
Six sources reported actual use of the MTWT tool to map patient journeys in other studies (Table 1). These were predominantly in Australia, with growing use of the concepts and implementation apparent in Canada. The tools were used to map diverse patient journeys for a range of purposes including: assisting direction and provision of services for Aboriginal patients experiencing chronic health conditions (Armstrong et al. 2021); understanding gaps in health care for rheumatic heart disease in pregnancy for Aboriginal women (Belton et al. 2018); understanding patients perspectives of barriers and enablers for burns care in Aboriginal children (Fraser 2019); patient experiences of pregnancy loss (Freeman 2020); cultural safety in Aboriginal patient journeys (Kelly 2017); and understanding access to care in hospitals following burn injuries for Aboriginal children (Ivers et al. 2015). Findings from this literature search informed design and content of the MTWT survey and identified potential survey participants.
| Authors | Publication title | Country of publication | Use of MTWT mapping tool | |
|---|---|---|---|---|
| Armstrong et al. (2021) | ‘You felt like a prisoner in your own self, trapped’: the experiences of Aboriginal people with acquired communication disorders. | Australia | MTWT mapping tools used to assist in the direction and provision of services for patients experiencing other chronic health conditions. Mapping was used by healthcare professionals to assist in navigating complex journeys. | |
| Belton et al. (2018) | Rheumatic heart disease in pregnancy: how can health services adapt to the needs of Indigenous women? A qualitative study. | Australia | MTWT concepts and to some extent tools were used to interview participants by journey modelling. This enabled understanding of the current gaps in care and identify improvements. | |
| Fraser (2019) | A disjuncture of world views: manifestation in burns care for Aboriginal and Torres Strait Islander children in Australia. | Australia | Mapping activities were conducted based on the MTWT tool. Mapping was used to understand the barriers/enablers of care from the patient’s perspective. | |
| Freeman (2020) | Navigating early pregnancy loss within Ontario’s healthcare system: a qualitative exploratory study of the experiences of midwifery clients and midwives. | Canada | Mapping activities based on MTWT tool. Mapping was used to visualise and understand patient experiences and response to issues. | |
| Kelly (2017) | Using mapping tools to improve Aboriginal patient journeys. | Australia | MTWT tool was used in teaching workshops and for assessing cultural safety. | |
| Ivers et al. (2015) | Understanding burn injuries in Aboriginal and Torres Strait Islander children: protocol for a prospective cohort study. | Australia | MTWT tool was used as a case study methodology to follow the journey of three Aboriginal children accessing care in hospitals following burn injuries. |
Phase 1b. MTWT survey
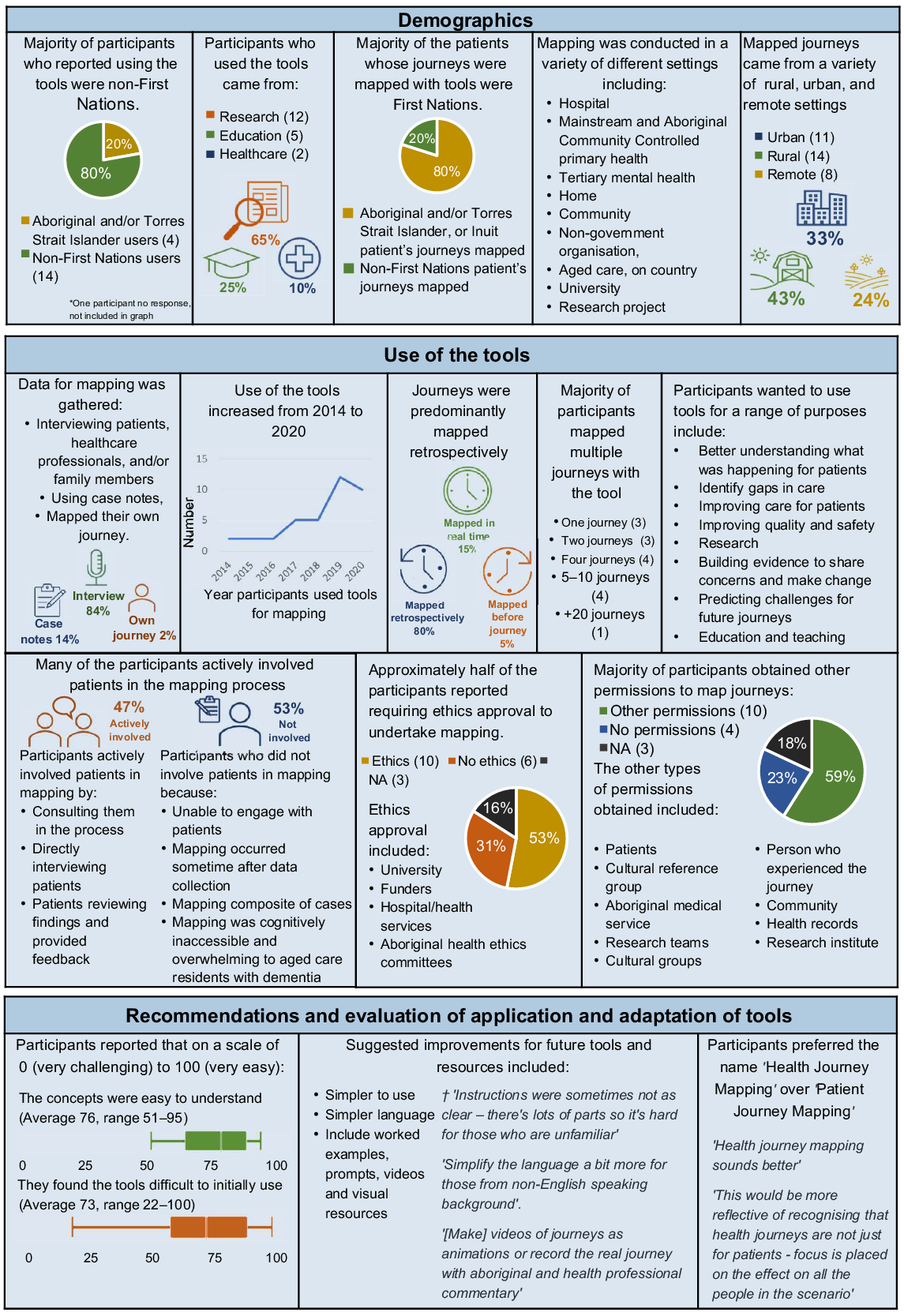
Findings from the survey identified that the MTWT tool was used by a range of people and purposes in diverse settings. The majority of participants who reported using the tool were non-First Nations (14 non-First Nations, 4 Aboriginal and/or Torres Strait Islander, 1 no response). They had backgrounds in research (12), education (5) and health care (2). The majority of patients whose journeys were mapped were First Nations (Aboriginal and/or Torres Strait Islander: 11, Inuit: 1, non-First Nations: 3).
The MTWT tool enabled users to support patients’ journeys in multiple ways including identification of gaps in their journeys, providing evidence for care, looking at multiple perspectives, being person centred and making sense of complex barriers to help seeking. The majority of participants mapped multiple patient journeys with the MTWT tool. Data for mapping was predominantly gathered via interviewing patients, healthcare professionals and/or family members (30), followed by using case notes (5) and one participant who mapped their own journey (1). The majority of mapping was conducted retrospectively (retrospective mapping, real time mapping, mapping before a journey). Many participants were actively involved patients in the mapping processes (actively involved patients: 8, did not actively involve patients: 9).
Many participants reported difficulty initially engaging with the tool and made suggestions to improve existing limitations. Participants particularly found the tool initially difficult to ‘pick up and use’, reporting that it took them time to understand how to use the tool and engage in mapping activities. Participants suggested making the tools simpler to use, including simpler language and worked examples, prompts and visual resources. Participants also preferred the name ‘Health Journey Mapping’ compared to ‘Patient Journey Mapping’ as it ‘would be more reflective of recognising that health journeys are not just for patients’ but also for families, community and healthcare professionals. Removal of the term ‘patient’ additionally identifies that individuals whose journeys are mapped have lives and responsibilities beyond their role as a patient (Fig. 2).
Phase 2. End user industry review and co-design
Input from end users informed the development of the new HJM resources by highlighting areas to focus on, format suggestions and recommended supplementary resources. End users specifically identified: the need to have three tools with different purposes: a clinical tool for busy clinicians to quickly pick up and use, a detailed care planning tool and a strategic tool to bring together multiple perspectives; for mapping to follow a four step process including a review stage; to link the tools and educational material to continuous quality and improvement, cultural safety, comprehensive care and the National Safety and Quality Health Service (NSQHS) standards (ACSQHC 2022); and for the mapping tools to be accessible in both Word and Excel versions (Table 2).
| Input from end usersA | How it informed development | |
|---|---|---|---|
Focus | Should have a focus on cultural safety. Partnership, safety and equity are used throughout the mapping process. | Resources linked to cultural safety and CQI. Resources include underlying principles of Safety, Equity and Partnership. | |
Link to standards of care. | Resource links directly to three NSQHS Standards (ACSQHC 2022), to support implementation in healthcare services: | ||
Mapping needs to focus on patients and their families. | Person centred approach. | ||
Usage | Our preference is that these tools will be for use across a range of healthcare settings.B | Tools designed to be used in all healthcare settings, for a variety of end users. | |
Uses familiar language for nurses. | Clinical HJM tool follows process plan to study act (to be familiar for clinical staff), while detailed and strategic HJM tools follow PAR process look and listen, think and discuss, take action together. | ||
For evaluation and reflection. | All tools include a review stage in mapping, to link to CQI. | ||
Clinicians/end users [will] read the principles first and this along with the tools would [better] ensure its safe use. | Underlying principles safety, equity and partnership to be overt throughout tools and education resources. | ||
Format | Separating into three different tools would be really good and so much easier to use and engage with. | Three distinct tools with unique purposes. | |
A tool needs to be created for busy clinicians. | A quick and easy Clinical HJM tool to be used in busy clinical settings. | ||
Detailed … tool could help us work out how to redesign our health service networks. | A detailed HJM tool for care planning. | ||
[Strategic] tool useful for high level state wide strategic planning. | A strategic HJM tool for reviewing models of care and strategic and collaborative planning. | ||
Consider how the tools can be used in multiple settings by multiple users. Can it be stand-alone without explaining it. | Tools available in different formats, with instructions and prompt questions embedded in tools. | ||
Keep review section a different colour. | Tools all have a review stage for CQI, that is specifically a different colour prompting users to complete. | ||
Supplementary resources | Include a recorded presentation/video in the package. | Includes an educational Power Point with voiceover and videos. | |
I actually think this tool works for both metropolitan and rural patients it would be good to see an example of both. | Case studies/worked examples created to reflect diverse patient journeys and support use. |
Phase 3. Field testing and piloting to inform final version
Findings from phases 1 and 2 resulted in the development of three distinct HJM tools (clinical, detailed and strategic) and educational materials (videos, worked examples, case studies and PowerPoints with voiceovers) (Fig. 3, Table 3). The clinical HJM tool was designed for busy healthcare clinicians to use in everyday practice. The detailed HJM tool enabled comprehensive care planning and evaluation. The strategic HJM tool brought together multiple perspectives of patients, family and health services across different stages of a journey. These tools were made available in interactive Excel, PDF and Word formats, following a four-step reflective mapping process (plan, do study, act and review for the clinical HJM tool; look and listen, think and discuss, take action together and review effectiveness for the detailed and strategic HJM tools). The research team facilitated multiple workshops with end users to identify how the resource could be best utilised in healthcare sites and adaptations needed to meet their specific requirements.
Summary of the three HJM mapping tools, their purposes and processes for mapping journeys (Phase 3 results). HJM, Health Journey Mapping.
| Educational material | Summary | ||
|---|---|---|---|
| Educational PowerPoints/Videos with voiceover | Why the HJM tools were developed. | PPT. Background information, holistic definitions of health, removing hierarchies, underlying principles safety equity partnership, NSQHS, cultural safety, explanation of journey mapping. | |
| Which HJM tool to use. | PPT. Explanation of clinical, detailed and strategic tools, comparison of tools, how to use tools, planning. | ||
| Resources to support your HJM experience. | PPT. Links to useful resources. | ||
| How to use the clinical HJM Tool. | PPT and Video. Background information, instructions to map with clinical HJM tool. | ||
| How to use the detailed HJM tool. | PPT and Video. Background information, instructions to map with detailed HJM tool. | ||
| How to use the strategic HJM tool. | PPT and Video. Background information, instructions to map with strategic HJM tool. | ||
| Case studies/Worked examples | Mrs Brown scenario. | Case studies (not actual patient journeys but representative journeys written by collating multiple actual stories and experiences) and worked examples in clinical, detailed and strategic HJM tools. | |
| Mary scenario. | |||
| Tim scenario. | |||
| Videos | About the HJM toolkit. | Introductory video explaining HJM resource and underlying principles. | |
| Health Journey Mapping workshop recording. | Two-part video recording of online workshop held by Janet Kelly, Amy Graham, and Alyssa Cormick with the Lowitja Institute, discussing use of the HJM tools. | ||
| Other | Health Journey. Mapping user guide. | Introduces Health Journey Mapping, comprehensive overview of the HJM resources and how to apply the tools in practice. |
PPT, PowerPoint; HJM, Health Journey Mapping; NSQHS, National Safety and Quality Health Standards.
These HJM tools and resources are increasingly being used by a range of healthcare workers and researchers across South Australia for First Nations and other recipients of care, this increase in use occurring both during and following the field testing and piloting phase. Uses include to map adolescent clinic transitions from the Women and Children’s Hospital to the Royal Adelaide Hospital, to identify gaps in care for near miss and poor outcomes for Aboriginal patients at the Royal Adelaide Wellbeing Hub, to map cardiac and eye care journeys at Flinders Medical Centre, to map health care experiences of women with disabilities who have experienced violence, to evaluate the role and effectiveness of kidney health peer navigators, to map the oral health journeys of people with chronic kidney disease and to voice renal health care recommendations by mapping the journey of an Aboriginal woman with chronic kidney disease (Cormick et al. 2022). Internationally the resources are being used by clinicians and researchers working with First Nations peoples in Canada.
Many end users identified that using the HJM mapping tools has helped them identify and legitimise the time required to build rapport and communicate more effectively with patients, even in a busy clinical settings. Those end users who had not applied the mapping tools instead utilised the concepts embedded within mapping tools and applied them to existing resources and clinical practices.
Discussion
The benefits of journey mapping are increasingly being recognised within Australia and internationally (Davies et al. 2022). Similar benefits were identified by users of the MTWT tool (Fig. 2) and early adopters of the HJM tools. The HJM tools and resources have been co-designed with multiple end users to identify and address diverse health care priorities and needs of First Nations people. They build upon the strengths of the earlier MTWT package, and address identified accessibility and usability limitations.
The resulting HJM tools and resources have stronger potential to identify and improve care for patients across different settings, embedding culturally safe and responsive care into primary, secondary and tertiary levels and providing evidence of this for accreditation.
The inclusion of the cyclical PAR approach (look and listen, think and discuss, take action together and review) (Kelly 2008) enables First Nations and non-First Nations end users to more effectively communicate and co-design care, while incorporating important elements of cultural safety, quality improvement and evaluation. Drawing on the diverse skills, expertise, perspectives and worldviews of end users, the resulting HJM tools and resources are relevant, flexible and applicable for different health journey experiences across a range of healthcare services and settings. These tools specifically focus on enabling First Nations people’s life and care experiences and priorities to be acknowledged and for patients to be actively involved in planning and evaluating their own care.
Educators involved in the tools’ development have introduced concepts of scaffolding and resource design that helps to clearly explain core concepts for new users. The design and structure of the tools were further strengthened by being piloted by people already familiar with mapping processes and those engaging with it for the first time. The PAR approach and co-design methodology (Stringer and Aragon 2021; Butler et al. 2022) used within this project can inform future research and development of culturally responsive health care and education models, demonstrating the value of collaborating with care consumers and healthcare, education and research end users.
One of the strengths of the new HJM tools and resources is that they provide a framework that enables healthcare professionals and services to identify, enact and record cultural safety and embed it into practice and models of care. Purposefully linking the National Safety and Quality Health Service (NSQHS) standards, in particular Standard 2: Partnering with consumers, Standard 5: Comprehensive care and Standard 6: Communicating for safety quality and safety (ACSQHC 2022), provides healthcare professionals and services with a mechanism to systematically evaluate and improve care, as well as co-design more responsive models of care, and provide evidence of this for accreditation. The HJM resources also promote the six specific actions the NSQHS developed for working with First Nations peoples (ACSQHC 2017).
Limitations
The tight timeline for completion linked to funding requirements was a limiting factor for this project. In addition, workforce demands associated with the COVID-19 pandemic reduced participation from those in healthcare settings. These demands limited end users ability to apply the tools in clinical settings, and moved many research activities from in-person to virtual formats. While this enabled flexibility for busy end users, it reduced opportunities for in-person collaboration. HJM implementation strategies are continuing beyond the project timelines, as discussed at the end of the Results section. There were more non-First Nations than First Nations participants, but three First Nations people were directly involved in the design and direction of the tools as part of the research team, and the HJM project worked in collaboration with the AKction project which is First Nations led and has a strong and diverse First Nations Reference Group. Members of this group also commented on and reviewed the HJM tools.
Future directions
Since completion of the project the tools have been implemented in various healthcare services and settings. Further research is evaluating the implementation, effectiveness and impact of the tools in improving access, experiences and outcomes of journeys. There is an emerging interest in how First Nations community members could use the tools themselves, combining cultural story-telling, art and journey mapping principles. For example, Peer Navigators in Port Augusta Kidney Care have used sand trays to map and share kidney dialysis and transplantation patient’s journeys, and the National Indigenous Kidney Transplantation Taskforce (NIKTT) are adapting the tools for community peer navigation use. The research team also plans to further engage with the university sector to design an education package specific for undergraduate and postgraduate education and research students. There is also growing interest in how the tools can be adapted and used more widely for other patient and client groups.
Conclusion
The HJM tools and resources have been co-designed with and for First Nations patients and families, and First Nations and non-First Nations healthcare professionals, educators and researcher end users to ensure they are applicable, adaptable, effective and culturally safe. These new tools enable diverse end users to better identify strengths and gaps in individual healthcare journeys, evaluate journeys against guidelines and standards, provide evidence for continuous quality improvement processes and identify solutions and respond to healthcare needs and priorities of First Nations patients and families, as well as other recipients of health care.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary materials.
Acknowledgements
We would like to acknowledge that this research project was conducted on the unceded lands of the Kaurna People on the Tartanyangga (Adelaide Plans, South Australia) and was informed by First Nations people from both Australia and Canada. We acknowledge all First Nations people involved in this project and pay our deepest respect to you and your families. We also acknowledge the Aboriginal Kidney Care Together – Improving Outcomes Now (AKction) research project and the First Nations community members and First Nations and non-First Nations healthcare professionals, researchers and educators who collaborated on this project. We thank the Lowitja Institute who funded this project, and worked collaboratively to co-design tools, resources and evaluation frameworks, and who now provide public access to the tools and resources on their website the Lowitja Learning Hub. We would also like to acknowledge Eileen Willis, Elizabeth Rix, Ellen Davies and Judith Dwyer who provided collegial peer review on this manuscript.
References
Armstrong E, Coffin J, Hersh D, Katzenellenbogen JM, Thompson SC, Ciccone N, Flicker L, Woods D, Hayward C, Dowell C, McAllister M (2021) “You felt like a prisoner in your own self, trapped”: the experiences of Aboriginal people with acquired communication disorders. Disability and Rehabilitation 43(13), 1903-1916.
| Crossref | Google Scholar | PubMed |
Australian Commission on Safety and Quality in Health Care (ACSQHC) (2017) Action 1.21: improving cultural competency. Available at https://www.safetyandquality.gov.au/standards/national-safety-and-quality-health-service-nsqhs-standards/resources-nsqhs-standards/user-guide-aboriginal-and-torres-strait-islander-health/action-121-improving-cultural-competency
Australian Commission on Safety and Quality Health Care (ACSQHC) (2022) The NSQHS standards. Available at https://www.safetyandquality.gov.au/standards/nsqhs-standards
Australian Health Practitioner Regulation Agency (AHPRA) (2020) National scheme’s Aboriginal and Torres Strait Islander health and cultural safety strategy. Available at https://www.ahpra.gov.au/About-Ahpra/Aboriginal-and-Torres-Strait-Islander-Health-Strategy/health-and-cultural-safety-strategy.aspx
Belton S, Kruske S, Jackson Pulver L, Sherwood J, Tune K, Carapetis J, Vaughan G, Peek M, McLintock C, Sullivan E (2018) Rheumatic heart disease in pregnancy: how can health services adapt to the needs of Indigenous women? A qualitative study. Australian and New Zealand Journal of Obstetrics and Gynaecology 58(4), 425-431.
| Crossref | Google Scholar | PubMed |
Butler T, Gall A, Garvey G, Ngampromwongse K, Hector D, Turnbull S, Lucas K, Nehill C, Boltong A, Keefe D, Anderson K (2022) A comprehensive review of optimal approaches to co-design in health with First Nations Australians. International Journal of Environmental Research and Public Health 19(23), 16166.
| Crossref | Google Scholar | PubMed |
Chamberlain C, Gee G, Brown SJ, Atkinson J, Herrman H, Gartland D, Glover K, Clark Y, Campbell S, Mensah FK, Atkinson C, Brennan SE, McLachlan H, Hirvonen T, Dyall D, Ralph N, Hokke S, Nicholson J (2019) Healing the past by nurturing the future – co-designing perinatal strategies for Aboriginal and Torres Strait Islander parents experiencing complex trauma: framework and protocol for a community-based participatory action research study. BMJ Open 9(6), e028397.
| Crossref | Google Scholar | PubMed |
Cormick A, Owen K, Turnbull D, Kelly J, O’Donnell K (2022) Renal healthcare: voicing recommendations from the journey of an Aboriginal woman with chronic kidney disease. Renal Society of Australasia Journal 18(3), 88-100.
| Crossref | Google Scholar |
Davies EL, Pollock D, Graham A, Laing RE, Langton V, Bulto L, Kelly J (2022) Reporting of patient journey mapping in current literature: a scoping review protocol. JBI Evidence Synthesis 20(5), 1361-1368.
| Crossref | Google Scholar | PubMed |
Fisher M, Mackean T, George E, Friel S, Baum F (2021) Stakeholder perceptions of policy implementation for Indigenous health and cultural safety: a study of Australia’s ‘Closing the Gap’ policies. Australian Journal of Public Administration 80(2), 239-260.
| Crossref | Google Scholar |
Fraser S (2019) A disjuncture of World views: manifestation in burns care for Aboriginal and Torres Strait Islander children in Australia. PhD Thesis, Flinders University, Adelaide, SA, Australia. Available at https://flex.flinders.edu.au/file/594bbe6b-d5c2-4581-9118-72352a933314/1/ThesisFraser2019OA.pdf
Fraser S, Mackean T, Grant J, Hunter K, Ryder C, Kelly J, Holland A, Griffin B, Clapham K, Teague WJ, Darton A, Ivers RQ (2021) Patient journey mapping to investigate quality and cultural safety in burn care for Aboriginal and Torres Strait Islander children and families – development, application and implications. BMC Health Services Research 22(1), 1428.
| Crossref | Google Scholar |
Freeman A (2020) Navigating early pregnancy loss within Ontario’s healthcare system: a qualitative exploratory study of the experiences of midwifery clients and midwives. Master’s Thesis, University of Waterloo, Ontario, Canada. Available at http://hdl.handle.net/10012/16288
Gatwiri K, Rotumah D, Rix E (2021) BlackLivesMatter in healthcare: racism and implications for health inequity among Aboriginal and Torres Strait Islander peoples in Australia. International Journal of Environmental Research and Public Health 18(9), 4399.
| Crossref | Google Scholar | PubMed |
Gollan S, Stacey K (2021) First Nations cultural safety framework. Australian Evaluation Society, Melbourne. Available at https://www.aes.asn.au/images/AES_FirstNations_Cultural_Framework_finalWEB_final.pdf
Ivers RQ, Hunter K, Clapham K, Coombes J, Fraser S, Lo S, Gabbe B, Hendrie D, Read D, Kimble R, Sparnon A, Stockton K, Simpson R, Quinn L, Towers K, Potokar T, Mackean T, Grant J, Lyons RA, Jones L, Eades S, Daniels J, Holland AJA (2015) Understanding burn injuries in Aboriginal and Torres Strait Islander children: protocol for a prospective cohort study. BMJ Open 5(10), e009826.
| Crossref | Google Scholar | PubMed |
Joseph AL, Kushniruk AW, Borycki EM (2020) Patient journey mapping: current practices, challenges and future opportunities in healthcare. Knowledge Management & E-Learning: An International Journal 12(4), 387-404.
| Crossref | Google Scholar |
Kelly J (2008) Moving forward together in Aboriginal women’s health: a participatory action research exploring knowledge sharing, working together and addressing issues collaboratively in urban primary health care settings. Doctoral Dissertation, Flinders University, Adelaide, SA, Australia. Available at https://flex.flinders.edu.au/file/00b93d55-fa65-4e01-af67-11aad0479eab/1/Thesis-Kelly-2009.pdf
Kelly J (2017) Using mapping tools to improve Aboriginal patient journeys. Australian Nursing & Midwifery Journal 24(9), 43.
| Google Scholar | PubMed |
Kelly J, Dwyer J, Mackean T, O Donnell K, Willis E (2017) Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care. Australian Journal of Primary Health 23(6), 536-542.
| Crossref | Google Scholar | PubMed |
Mackean T, Fisher M, Friel S, Baum F (2020) A framework to assess cultural safety in Australian public policy. Health Promotion International 35(2), 340-351.
| Crossref | Google Scholar | PubMed |
Nolan-Isles D, Macniven R, Hunter K, Gwynn J, Lincoln M, Moir R, Dimitropoulos Y, Taylor D, Agius T, Finlayson H, Martin R, Ward K, Tobin S, Gwynne K (2021) Enablers and barriers to accessing healthcare services for Aboriginal people in New South Wales, Australia. International Journal of Environmental Research and Public Health 18(6), 3014.
| Crossref | Google Scholar | PubMed |
The Lowitja Institute (2015) Managing two worlds together: improving the Aboriginal patient journey. Available at https://www.lowitja.org.au/page/research/research-categories/health-services-and-workforce/cultural-safety/completed-projects/managing-two-worlds-together-state-3-aboriginal-patient-journey-mapping-tools-project
Wilson A, Wilson R, Delbridge R, Tonkin E, Palermo C, Coveney J, Hayes C, Mackean T (2020) Resetting the narrative in Australian Aboriginal and Torres Strait Islander nutrition research. Current Developments in Nutrition 4(5), NZAA080.
| Crossref | Google Scholar |
Yashadhana A, Fields T, Burnett A, Zwi AB (2021) Re-examining the gap: a critical realist analysis of eye health inequity among Aboriginal and Torres Strait Islander Australians. Social Science & Medicine 284, 114230.
| Crossref | Google Scholar | PubMed |