Exploring the feasibility of a gambling harm screening model in general practice and community service settings in Fairfield: a pilot study
Andrew Reid A B C D * , Nick McGhie
A B C D * , Nick McGhie  E , Thi Huyen Linh Nguyen
E , Thi Huyen Linh Nguyen  E , Uday Yadav
E , Uday Yadav  F , Patricia Cullen
F , Patricia Cullen  G , Leon Booth
G , Leon Booth  H and Amy Bestman
H and Amy Bestman  G I
G I
A
B
C
D
E
F
G
H
I
Abstract
Gambling is a growing public health issue in Australia. However, limited research has examined the role of primary health care and social services in routine screening for gambling harm in Australia. This research aimed to explore the enablers and barriers to implementing a co-designed gambling screening model in Fairfield, New South Wales – an area with high gambling expenditure.
A co-designed gambling screening and referral model for GP and community-based organisations was implemented in Fairfield in 2020. Follow-up interviews were conducted with nine health care professionals who implemented the screening in 130 patients. Thematic analysis generated key barriers and enablers for implementation of this model.
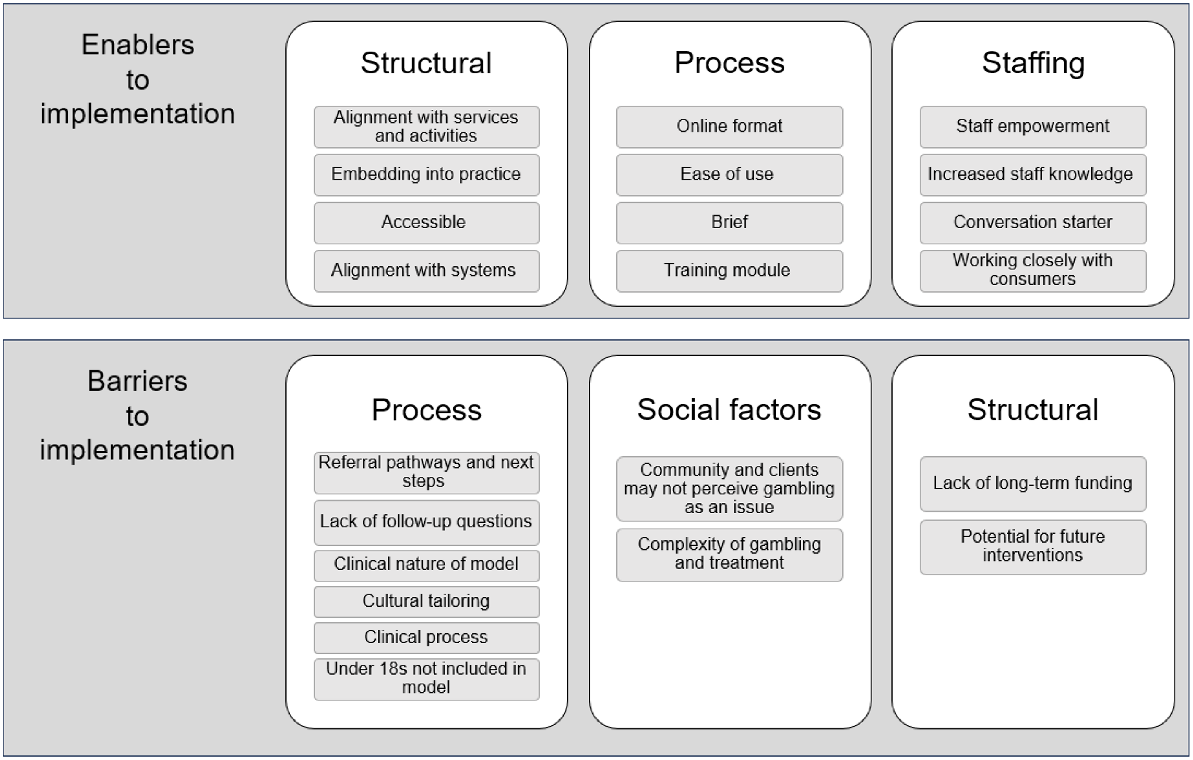
Key enablers for the screening model implementation included structural factors (alignment of the screening model with current work), process factors and staffing factors (staff empowerment). However, we also noted process factors as a barrier to implementation, particularly the referral pathway following screening. Other barriers included social and structural factors, such as the complexity of gambling harm and project funding.
Embedding routine screening in primary and community care settings can play a role in treating, reducing and preventing gambling-related harm, and reducing stigma in Fairfield and beyond. Additionally, screening models such as this provide health systems with clear evidence on the level of gambling harm in their community (particularly important in culturally and linguistically diverse communities who are underrepresented in research). This evidence is important for addressing system-level drivers of harm and advocating for political reform to reduce the impact of gambling on communities.
Keywords: culturally diverse communities, gambling harm, health services, implementation research, public health, qualitative methods, screening.
Introduction
Gambling causes significant health and social harm in Australia and internationally (Hilbrecht et al. 2020; Wardle et al. 2021; Hing et al. 2022). Recognising the broader impacts of gambling on individuals, families and communities (Browne et al. 2017; Price et al. 2021), there has been a shift towards a public health approach to address gambling harm (Wardle et al. 2019; Hing et al. 2022). A considerable proportion of gambling-related harm now comes from low- or moderate-risk gamblers, in addition to ‘problem gamblers’, which is a term frequently used to describe people who experience significant gambling harm (Dowling et al. 2015; Miller 2017; Riley et al. 2018).
Assessing gambling harm
Current models assessing gambling harm in Australia may be inadequate due to the reliance on self-disclosure to health care providers (Browne et al. 2016), with only a small proportion of patients (1%) seeking help for gambling-related harm (Australian Institute of Health and Welfare 2023). This is a challenge for culturally and linguistically diverse (CALD) community members who may refrain from discussing gambling harm with health care providers due to the associated stigma (Dickins and Thomas 2016). Gambling screening in primary care settings can provide opportunities to discuss gambling, identify at-risk individuals and improve treatment outcomes (Browne et al. 2017, 2023; Roberts et al. 2019). However, limited research to date has explored the use of screening in Australian CALD communities (Dickins and Thomas 2016; Rowlatt et al. 2023). Implementing gambling screening in general practice (GP) settings could help to overcome gambling stigma and support CALD communities. Although there is some guidance for general practitioners (GPs) on initiating conversations about gambling, there is a need to assess the acceptability of this approach in CALD communities (Oei et al. 2019).
Screening measures for gambling harm may also be suitable for non-health community services in disadvantaged and CALD communities. There is an established link between gambling harm and harmful alcohol consumption (Currie et al. 2013), family violence (Abbott et al. 2014; Dowling et al. 2014, 2016), and financial harm (Marko et al. 2023). In Australia, due to the high comorbidity between gambling harm and related issues addressed in primary care and community services, implementing gambling screening measures in these contexts is likely to be beneficial.
Co-designing a screening model for gambling harm
This research was based in the Fairfield local government area (termed Fairfield from this point forward), in urban NSW. Fairfield is known for its high level of disadvantage, ranking in the lowest decile for socioeconomic status in Australia, and considered the most disadvantaged area in the Greater Sydney area (Australian Bureau of Statistics 2016). The area is highly culturally diverse, with nearly 60% of residents born overseas and 76% speaking a language other than English at home (Australian Bureau of Statistics 2016). Gambling is a significant issue in this area, with the 3841 electronic gambling machines (as of 2022) resulting in a daily loss of AU$1.7 million (Rachwani 2023).
In 2017, the Fairfield City Health Alliance established the Gambling Working Group, consisting of key stakeholders from local government, South Western Sydney Local Health District, South West Sydney Primary Health Network, multicultural gambling service, social service providers and academics, to address gambling harm in Fairfield, NSW. Through community consultation, a knowledge gap among service providers regarding gambling harm and a lack of empowerment to address harms were identified. The current research was part of a larger study that utilised a co-design approach and a literature review to address these gaps, and create a gambling screening and referral model for GP and community-based services in Fairfield, NSW (Nguyen and McGhie 2020). The co-designed screening model, implemented by GPs and community workers for 13 weeks in 2020, was developed for CALD communities, and materials were translated into three languages (Arabic, Assyrian and Vietnamese). Additionally, a training and resource kit was developed for professionals delivering the model (Nguyen and McGhie 2020).
The screening model asked individuals to complete the three-item Problem Gambling Severity Index short form assessment (Volberg and Williams 2012) and the Concerned Others Gambling Screen to identify individual harm caused by someone else’s gambling (Sullivan et al. 2007). If the screening indicated harm, the provider initiated a conversation and provided a list of gambling help services for them to contact. As the pilot focused on local cultural groups, referrals were often made to the NSW multicultural problem gambling service (Nguyen and McGhie 2020).
During implementation of the screening model, 130 patients completed the online screening, with follow-up actions (such as referral to help services) administered by providers. Quantitative analysis of the screening data revealed that 40% had no risk of gambling harm, 17% were considered at-risk due to their gambling behaviour and 20% due to someone else’s gambling behaviour (Nguyen and McGhie 2020). Just under one-quarter of patients (23%) were identified as being at risk of gambling harm from both personal and someone else. These rates of gambling harm are substantially higher than the 2019 NSW state prevalence survey, which reported 1% of the NSW population as problem gamblers and 9.4% of participants classified as being either low- (6.6%) or moderate- (2.8%) risk gamblers (Browne et al. 2019). One-third of patients (37%) were provided with information about support services, and 10% were referred to help services (Nguyen and McGhie 2020).
Following the implementation of the model, a qualitative evaluation was conducted with providers to examine the enablers and barriers to the model’s implementation, given the high rates of gambling harm identified. This paper reports on these findings.
Methods
Design and setting
As described above, the present study is part of a larger project that aimed to co-design, implement and evaluate a gambling screening model using mixed methods. Here, we report the findings of qualitative interviews with providers to understand their perspectives on the feasibility, acceptability, barriers and enablers of the gambling screening model implementation in routine practice.
Recruitment and data collection
The sample for this study were the GPs and community workers who administered the screening model (n = 12). Following the implementation of the model, two participants dropped out due to lack of capacity to implement the screening, and another withdrew for personal reasons. These results report on the perspectives of the remaining participants who implemented the model. To showcase some of the various stakeholders and perspectives, we have assigned each a participant number in the results.
All participants received a Participant Information Sheet and Consent Form. In July 2020, the project team conducted eight interviews with nine participants, including two GPs and seven community workers from five local organisations. Open-ended questions explored implementation experiences, including barriers faced, observed effects and perceived usefulness of the model. The 1-hour interviews were conducted remotely via phone or video conferencing software. Participant data were de-identified before analysis, and the findings were reported in a manner that protects individual participant anonymity.
Data analysis
Data were analysed using a thematic approach (Braun and Clarke 2021), focusing on acceptability, feasibility, factors that facilitated or hindered intervention implementation and drawing lessons for public health. This study was conducted in 2020 during the COVID-19 pandemic. Consequently, project implementation was adjusted to meet participant needs, such as using telehealth appointments. We have examined and reported these impacts in our current paper.
Results
Fig. 1 is a summary of the key themes identified from participant responses. More prominent themes are presented first in each list. Below are further descriptions of these themes.
Enablers to implementation
Structural factors facilitated the screening model implementation. Participants noted screening for gambling harm was congruent with the subject matter of the services, such as drug and alcohol services or domestic violence services, and the specific activities of the service, such as enquiries about living situation, employment, health and health behaviours. This commentary highlighted the positive addition of screening to holistic patient care. For example, one GP identified that questions about gambling harm could be integrated into their practice as part of their overall comprehensive approach, similar to asking about smoking or alcohol consumption. While a participant from a community-based organisation stated:
Because it’s just another thing that you can add in. Because if we’re going to check up on people’s different areas of their life that they may be struggling in or if they’ve come in for a ‘no interest loan scheme’, and something shows up in their income statement where there’s large bulks of money going in and out, then there’s a way that you can actually talk to them about it. To go look, this is what I’ve identified. There seems to be a pattern of behaviour happening. Can we explore this a bit more? That way you can end up using the tool [model] that way. To say, ‘Look, we’re here not to judge you. We’re here to support you’. (Participant #1 – Community Worker)
The alignment of the model with the provided services facilitated staff’s ability to embed the screening into standard protocols to better engage with clients and provide support in a range of aspects of their life:
[For example] link with services and say, ‘Just be careful, this might become a problem. You might start substituting your drinking or your drugs for gambling, and if you’re getting a couple of wins, they’re going to entice you then to spend more’. So, it’s just put in that way, to be more aware of things that are affecting young people and how easy it could be to swap one [harmful behaviour] for the other. (Participant #2 – Community Worker)
During COVID-19, paper-based screening questions were adapted for telehealth services into an online format. Participants perceived this increased accessibility of the screening model for patients. Additionally, administering the survey online aligned with existing processes and workload. Integrating screening into the intake or standard consultation procedures for GPs and community workers made it easier to access and utilise. GPs supported embedding screening into computer systems, making it convenient to remember to ask gambling questions consistently.
Participants also noted entering screening results into an online survey was convenient. However, community workers expressed challenges conducting the screening over the phone during telehealth appointments (during COVID-19), as they believed face-to-face interactions allowed for a more supportive environment to ask sensitive questions and interpret nonverbal cues. They anticipated that data collection would be more suitable once in-person appointments resumed. Participants appreciated the ability to receive feedback through the online platform, such as email updates on the number of clients screened, which served as motivation to continue the intervention.
Moreover, participants highlighted the model’s ease of use, particularly noting the brevity of the three-item screening questionnaire and use of validated instruments for identifying gambling harm, simplifying the implementation process. None of the participants found the process challenging. The training module and resource kit provided at the beginning of the pilot project served as crucial process-related enablers. Participants reported their involvement in the pilot, particularly the training, improved their understanding of gambling issues and increased their comfort in initiating conversations about gambling with clients. The webinar and access to recorded content received positive feedback, and participants found additional training resources, such as follow-up emails, valuable. The resource kit, available in English, Arabic, Assyrian and Vietnamese, was user-friendly and provided a model for effective communication with clients. Some participants highlighted the resource kit’s ability to initiate discussions about gambling in a non-stigmatising manner.
The third enabling theme was the staffing factors related to implementing the screening model. All nine participants expressed positive responses to their involvement in the pilot project. A key theme that emerged was screening served as a supportive entry point for discussing gambling with clients (or patients). Although some participants emphasised the project’s impact on their confidence in addressing gambling harm, one GP stressed the importance of building patients’ comfort during discussions on gambling harm, while a community worker stated, ‘I feel like I can help – I feel confident in conducting assessments and providing referrals and information.’ Another community worker mentioned participating in the pilot project enabled them to gain experience in broaching the topic of gambling with clients, and increased their confidence to continue these discussions beyond the project. One GP commented:
To be honest it probably wasn’t something that I addressed or raised or dealt with often enough beforehand, and probably was something … wouldn’t have always initiated on my own unless it was brought up to me … In that sense [being involved in the pilot], it’s probably something I’m a little bit more comfortable bringing up, and just mentioning it and doing that sort of very even basic discussion … So yeah, a little bit more – a bit more on my radar now. I’m doing it a bit more. (Participant #4 – GP)
Barriers to implementation
The first barrier pertained to the referral processes of the screening model, including the unclear process for service providers to support patients through referrals in this model. A community service participant preferred to offer clients the option of making a joint call to services for information before making a referral. Another community worker suggested a clear online referral system instead of a list of contacts. Additionally, a service provider noted that although the materials and cultural groups chosen for the study were appropriate, they limited engagement with other populations. They recommended ongoing consideration of target audiences and continuous material updates, as needed.
The second barrier was the brevity of the screening model. Although the model’s brevity was generally seen as useful, some practitioners found the short and formal interaction made it difficult to engage in meaningful discussions with clients. In response, some participants opted to take a more conversational approach to the questionnaire rather than adhering to the strict question-and-answer format. One participant recommended providing additional support and more detailed follow-up questions to community workers.
Another barrier related to the need for workers to remember to administer screening to all patients. One GP shared specific challenges related to their current practice systems, highlighting the necessity for reminders to complete the screening model. They proposed integrating the model into medical software to surmount these barriers and seamlessly incorporate the model into routine clinical practice for continuous screening. One suggestion was to have an iPad in the waiting room for patients to self-administer questionnaires that automatically link into practice medical records.
The screening model used in the current model was designed for adults aged >18 years. Some community workers raised concerns about this limitation, as they often work with children affected by others’ gambling or who engage in gambling themselves. However, it is worth mentioning that some participants in the pilot felt empowered to utilise their training to initiate conversations about gambling with youth. As one worker stated:
So just opening up that, so I found that that was a really good way to just start building on that relationship regarding gambling. (Participant #2, Community Worker)
Another barrier was related to social factors impacting the implementation of the screening model. Two key themes emerged. First, some clients did not recognise their gambling behaviour as harmful, and some were unaware that their actions constituted gambling. This initially hindered support, especially for those seeking help from alcohol and other drug services. Second, gambling harm and treatments were complex. Community workers emphasised the need to prioritise other pressing issues, such as financial harm, domestic violence and homelessness, particularly for individuals affected by others’ gambling. One worker ensured clients received emotional and mental health support while providing information about gambling help services. Therefore, addressing gambling-related concerns was often not the top priority, rather a secondary issue.
The final barrier relates to the structural factors that hindered the model implementation. Participants noted that the absence of dedicated long-term funding for gambling screening creates uncertainty about the continuation of screening resources, and developing procedures for screening in GP and community service settings. This was perceived as impacting the continuation and scaling up of the intervention, and also on intake procedures for gambling screening harm within both GP and community service settings. More funding needed to address these concerns was noted.
Discussion
Gambling harm is a significant public health concern (Wardle et al. 2019, 2021; Hilbrecht et al. 2020), profoundly impacting specific populations, including those within the Fairfield community (Nguyen and McGhie 2020). Given gambling harm is caused by the complex interplay of individual, social, environmental and commercial dimensions (Browne et al. 2017; Hing et al. 2022), population-based screening tools (such as part of routine primary care) provide an important opportunity to capture data on gambling harm (Blythe and van Schalkwyk 2021). The current research supports the role of primary health care screening as an entry point to: (1) identify the level of gambling harm within community settings, (2) support active referral of those experiencing gambling harm to support services, (3) support a holistic approach to patient care by addressing gambling as part of comorbidities, and (4) de-stigmatise gambling harm.
However, it should be noted that screening alone is not sufficient to reduce harm caused by gambling. Highlighting the prevalence of harm at the local level, particularly in culturally diverse areas, can signal the need for action on gambling harm. This should be underpinned by a comprehensive public health framework to prevent gambling harm (Thomas et al. 2023). The feasibility of a local, primary care-delivered screening model for gambling harm presents key opportunities. This research raises the following areas for discussion.
First, through discussions with primary health care workers and those working in social services in this pilot study, it was clear that staff were unprepared and lacked confidence in discussing gambling harm, despite these issues being prevalent among their clients. This is particularly critical given the high levels of gambling harm observed in this study. Therefore, all staff in this region must be adequately trained to engage in conversations around gambling harm, recognise indicators of gambling harm, and provide the appropriate referral and help-seeking pathways. Incorporating gambling screening models into standard practice can empower health care professionals to engage in this harm mitigation strategy. However, adequate and long-term funding of the screening model (including training, implementation and monitoring, and evaluation) should be supported. One proposal to further enable uptake of the model was to embed screening tools into practice management software systems. Future research should examine the feasibility of this, including the availability of long-term funding to ensure sustainability.
Second, primary health care professionals engaging in conversations about gambling harm can play an important role in de-stigmatising gambling issues, and reducing individual and community stigma associated with help-seeking (Dickins and Thomas 2016). In line with Australian research (Dickins and Thomas 2016; Brown and Russell 2020), the present findings suggest stigma poses a significant barrier to gambling treatment in CALD settings. However, the examined model assisted health and community workers to have open and non-stigmatising discussions around gambling harms, which appeared to increase community members’ openness to engage in these conversations. Integrating the screening model into standard practice is likely to facilitate productive conversations about gambling, and holds promise for potentially mitigating gambling-related shame within CALD communities, such as Fairfield. Based on the findings of this research, we propose this approach as being appropriate to culturally diverse community needs. Furthermore, we recommend that discussions should adopt a public health perspective to gambling harm and avoid placing blame on the individual, but instead highlight the role of the environment in gambling harm (Miller et al. 2018). Doing so could foster shifts in community attitudes to gambling harm that place more responsibility on industry rather than individuals.
Third, the project was focused on delivery of the screening model in GPs and social community services. However, a key component of this is ensuring patients who indicate gambling harm are appropriately supported and referred to gambling help services. Analysis of raw data revealed that 32% of patients exhibited indications of gambling harm (Nguyen and McGhie 2020), levels that are much higher than the NSW state average (Browne et al. 2019). These results may have occurred for several reasons. First, the population screened in this larger project were predominantly from CALD backgrounds, a population group often missing in gambling research studies. Second, the screening model also sought to identify patients who might be affected by another person’s gambling behaviour. Third, although the screening model was offered to all patients within a service, those who experience gambling harm might be more likely to choose to participate in the screening. Future research should seek to examine gambling harm prevalence in this area further. However, regardless of the reasons for these high positive screens, any future implementation of screening in general practice and community services must have appropriate referral pathways in place to support patients. This was an area of weakness in our study, with no specific defined referral pathway besides providing patients with materials for gambling support services. Future research should explore how referral mechanisms can be integrated into the model in a culturally appropriate way. As noted by some participants in this study, this includes whether it is feasible for health professionals to sit with patients while they connect to services (i.e. through calling gamblers help). Special attention should also be dedicated to offering adequate support for cases involving violence and financial hardships.
Finally, key limitations of this study should be noted. First, the pilot project evaluation sample was limited due to time constraints within clinical settings. Consequently, this sample only included nine participants. We also note a gap in the range of participants, and in future would like to seek the perspectives of practice nurses and practice owners involved in implementing the model. Second, because of the first wave of the COVID-19 lockdown in NSW, face-to-face engagement was severely restricted, adversely affecting project recruitment, uptake and overall implementation. Although there was online engagement in the delivery of the model, the absence of face-to-face interaction hindered our capacity to establish the necessary relationships with professionals to engage in the project. Future research should seek to further evaluate the screening model on a larger scale to examine the effectiveness of the model in supporting gambling harm reduction in CALD communities. Finally, future research should seek to examine the feasibility and acceptability of the screening model with consumers, particularly those from different cultural backgrounds. This is particularly important given the screening tools have not been validated specifically for the communities this project sought to work with (Arabic, Assyrian and Vietnamese).
Conclusions
Primary healthcare and community service settings can play a role in screening for and mitigating gambling harm within communities. From the perspective of health and community workers, this screening model has shown real promise for addressing gambling in health and community settings. Future work should focus on addressing the barriers identified to the model and evaluating the impacts of the model on community members, particularly those from different cultural backgrounds, to ensure that the model is culturally appropriate and effective. Finally, screening for gambling harm in local care settings can provide important data on the extent of gambling harm. This is an important tool to support harm reduction and regulatory change to reduce and prevent gambling harm.
Data availability
The data presented in this paper is confidential and will not be made publicly available.
Declaration of funding
The pilot study was funded by the New South Wales Government under the 2018 Responsible Gambling Grants Program.
Acknowledgements
We want to acknowledge the invaluable contribution to the project by the Fairfield City Health Alliance Gambling Working Group members and the participants involved in this research project.
References
Australian Bureau of Statistics (2016) Census QuickStats: fairfield (C). Australian Bureau of Statistics. Available at https://www.abs.gov.au/census/find-census-data/search-by-area [Retrieved 1 September 2023]
Australian Institute of Health and Welfare (2023) Gambling in Australia. AIHW, Australian Government. Available at https://www.aihw.gov.au/reports/australias-welfare/gambling [Retrieved 2 January 2024]
Blythe J, van Schalkwyk M (2021) Screening for gambling harms in primary care. The BMJ Opinion. Available at https://blogs.bmj.com/bmj/2021/06/18/screening-for-gambling-harms-in-primary-care/
Braun V, Clarke V (2021) Thematic analysis: practical guide [eBook version]. (SAGE Publications).
| Google Scholar |
Brown KL, Russell AMT (2020) What can be done to reduce the public stigma of gambling disorder? Lessons from other stigmatised conditions. Journal of Gambling Studies 36(1), 23-38.
| Crossref | Google Scholar |
Browne M, Langham E, Rawat V, Greer N, Li E, Rose J, Rockloff M, Donaldson P, Thorne H, Goodwin B, Bryden G, Best T (2016) Assessing gambling-related harm in Victoria: a public health perspective. V. R. G. Foundation. Available at https://responsiblegambling.vic.gov.au/documents/69/Research-report-assessing-gambling-related-harm-in-vic.pdf
Browne M, Rawat V, Greer N, Langham E, Rockloff M, Hanley C (2017) What is the harm? Applying a public health methodology to measure the impact of gambling problems and harm on quality of life. Journal of Gambling Issues 36, 28-50.
| Crossref | Google Scholar |
Currie SR, Hodgins DC, Casey DM (2013) Validity of the problem gambling severity index interpretive categories. Journal of Gambling Studies 29(2), 311-327.
| Crossref | Google Scholar |
Dowling NA, Jackson AC, Suomi A, Lavis T, Thomas SA, Patford J, Harvey P, Battersby M, Koziol-McLain J, Abbott M, Bellringer ME (2014) Problem gambling and family violence: Prevalence and patterns in treatment-seekers. Addictive Behaviors 39(12), 1713-1717.
| Crossref | Google Scholar |
Dowling NA, Cowlishaw S, Jackson AC, Merkouris SS, Francis KL, Christensen DR (2015) Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: a systematic review and meta-analysis. Australian & New Zealand Journal of Psychiatry 49(6), 519-539.
| Crossref | Google Scholar |
Dowling N, Suomi A, Jackson A, Lavis T, Patford J, Cockman S, Thomas S, Bellringer M, Koziol-Mclain J, Battersby M, Harvey P, Abbott M (2016) Problem gambling and intimate partner violence: a systematic review and meta-analysis. Trauma, Violence, & Abuse 17(1), 43-61.
| Crossref | Google Scholar |
Hilbrecht M, Baxter D, Abbott M, Binde P, Clark L, Hodgins DC, Manitowabi D, Quilty L, SpÅngberg J, Volberg R, Walker D, Williams RJ (2020) The conceptual framework of harmful gambling: a revised framework for understanding gambling harm. Journal of Behavioral Addictions 9(2), 190-205.
| Crossref | Google Scholar |
Hing N, Russell AMT, Browne M, Rockloff M, Tulloch C, Rawat V, Greer N, Dowling NA, Merkouris SS, King DL, Stevens M, Salonen AH, Breen H, Woo L (2022) Gambling-related harms to concerned significant others: a national Australian prevalence study. Journal of Behavioral Addictions 11(2), 361-372 Available at https://researchers.cdu.edu.au/en/publications/gambling-related-harms-to-concerned-significant-others-a-national.
| Google Scholar |
Marko S, Thomas SL, Pitt H, Daube M (2023) The lived experience of financial harm from gambling in Australia. Health Promotion International 38(3), daad062.
| Crossref | Google Scholar |
Miller HE, Thomas SL, Robinson P (2018) From problem people to addictive products: a qualitative study on rethinking gambling policy from the perspective of lived experience. Harm Reduction Journal 15(1), 16.
| Crossref | Google Scholar |
Price A, Hilbrecht M, Billi R (2021) Charting a path towards a public health approach for gambling harm prevention. Journal of Public Health 29(1), 37-53.
| Crossref | Google Scholar |
Rachwani M (2023) Silent epidemic’: almost two-thirds of Sydney’s gambling losses occur in city’s west. Available at https://www.theguardian.com/australia-news/2023/feb/12/silent-epidemic-almost-two-thirds-of-sydneys-gambling-losses-occur-in-citys-west [Retrieved 6 September 2023]
Riley BJ, Harvey P, Crisp BR, Battersby M, Lawn S (2018) Gambling-related harm as reported by concerned significant others: a systematic review and meta-synthesis of empirical studies. Journal of Family Studies 27(1), 112-130.
| Crossref | Google Scholar |
Roberts A, Bowden-Jones H, Roberts D, Sharman S (2019) Should GPs routinely screen for gambling disorders? British Journal of General Practice 69(682), 226-227.
| Crossref | Google Scholar |
Rowlatt V, Wraith D, Doan T-VM, Malatzky C (2023) Culturally and linguistically diverse gamblers of East Asian Descent in Australia: a comprehensive review of current evidence. Journal of Gambling Studies 39(2), 947-969.
| Crossref | Google Scholar |
Sullivan S, McCormick R, Lamont M, Penfold A (2007) Problem gambling: patients affected by their own or another’s gambling may approve of help from general practitioners. The New Zealand Medical Journal 120(1257), U2605.
| Google Scholar |
Thomas SL, Crawford G, Daube M, Pitt H, Hallett J, McCarthy S, Francis L, Edmunds M (2023) Time for policies on gambling to benefit health – not the gambling industry. Health Promotion Journal of Australia 34(2), 267-271.
| Crossref | Google Scholar |
Volberg RA, Williams RJ (2012) Developing a short form of the PGSI. Report to the Gambling. (G. Commission) Available at https://assets.ctfassets.net/j16ev64qyf6l/3B8AogTkdtA6LxTCs1knvK/0f6c6d5127f4037666242b345e4ca5de/Developing_a_Short_Form_of_the_PGSI.pdf
Wardle H, Reith G, Langham E, Rogers RD (2019) Gambling and public health: we need policy action to prevent harm. BMJ 365, l1807.
| Crossref | Google Scholar |
Wardle H, Degenhardt L, Ceschia A, Saxena S (2021) The Lancet Public Health Commission on gambling. The Lancet Public Health 6(1), e2-e3.
| Crossref | Google Scholar |