Perceptions of general practitioners towards managing dental presentations in Australia: a qualitative study
Ruby Biezen A , Angel Leong B and Leanne Teoh
A , Angel Leong B and Leanne Teoh  B *
B *
A
B
Abstract
Patients presenting with dental pain are common in general practice, despite dental infections being most appropriately managed with dental treatment to address the cause of the infection. Although antibiotics are not appropriate for the management of localised toothache without signs of systemic spread, general practitioners (GPs) often prescribe antibiotics and analgesics for the management of dental pain. The aim of this study was to explore GPs’ perceptions and management of dental presentations in Australia.
Twelve semi-structured interviews were conducted with GPs across Victoria, Australia, between October 2022 and January 2023. Data were thematically analysed.
The study found that dental pain was the most common presenting complaint for patients attending general practice with a dental problem. Five major themes were identified in this study: knowledge, beliefs about capabilities, emotion, environmental context and resources, and social influences/social professional role and identity. In terms of knowledge and capabilities, GPs would advise patients to seek dental care, as they are aware that antibiotics would not resolve the underlying issue. Challenges for GPs included limited training in oral and dental treatment, as well as emotions, such as patient anxiety and phobia resulting in patients seeking dental care through a GP rather than a dentist. Barriers due to the context, such as access to dental care, long waiting lists within the public dental system and cost, were some of the reasons patients present to general practice rather than a seeing a dentist. Furthermore, issues that influenced GPs’ antibiotic prescribing included patients’ expectations for antibiotics to treat their dental pain, as well as dentists advising their patients to attend their GP for antibiotics prior to dental treatment.
This study identified factors that influenced GPs’ management of patients with dental conditions. To address these issues, it is imperative to develop interventions addressing patients’ knowledge around oral health, as well as providing improved access to dental care for these patients.
Keywords: antibiotic, antibiotic prescribing, dental, dentist, general practitioner, patient healthcare, primary care, toothache.
Introduction
Oral diseases, such as tooth decay and gum disease, are the most common chronic conditions, affecting approximately 3.5 billion people worldwide (WHO 2022). In Australia, 10% of adults have severe tooth loss and 31% have untreated tooth decay (Australian Dental Association (ADA) 2020). Dental treatment, such as fillings, root canal treatments or extractions, are required for the source of the problem to be addressed. However, patients with dental conditions often visit general practice instead of a dentist. Approximately 750,000 visits to primary care general practitioners (GPs) were for dental conditions in Australia in 2011 (Sen Gupta and Stuart 2020).
Cost and access to timely dental care have been cited as barriers for patients to obtain treatment from a dentist. Affordability of dental care was the reason for 39% of people aged 15 years and older avoiding or delaying a dental visit, and 23% of patients who attended a dentist chose not to proceed with dental treatment in Australia due to cost (AIHW 2022). A study in Wales found that patients expressed concern around the ‘lack of transparency regarding costs associated with dental care’ (Cope et al. 2018). Access to dental care in Australia is mostly delivered through the private sector, with only approximately 11% of dentists working in public practice (Department of Health 2016). Therefore, the provision of public practice dentistry is disproportionate to the one-third of the Australian population who are eligible for treatment. As a result, long waiting lists are common, with some patients waiting up to 2 years to access routine dental care (AIHW 2018). Cope et al. (2018) also found difficulties in accessing dental services in Wales as one of the reasons that patients seek GPs for their dental treatment. Therefore, these barriers are contributing factors influencing patients to seek dental care in general practice instead of dentistry (Sen Gupta and Stuart 2020).
The vast majority of dental issues require treatment by dental procedures; antibiotics are often not required, as they are adjunctive to dental treatment. In general, they are only needed when a tooth infection shows signs of systemic spread (Therapeutic Guidelines 2019). However, multiple studies have shown that GPs tend to prescribe antibiotics as treatment for dental conditions (Anderson et al. 2000; Cope et al. 2015; Nguyen et al. 2023). An Australian case–vignette study of 30 GPs who worked in rural Queensland, Tasmania and South Australia between 2013 and 2014 showed that GPs tend to prescribe antibiotics and short-term pain relief for dental conditions, including toothaches, dental abscesses and acute orofacial pain (Park et al. 2022). Furthermore, they reported that costs of travelling to the dentist also discouraged patients from seeking dental care. A qualitative study of GPs in Wales also showed that the majority will prescribe antibiotics for a dental problem (Cope et al. 2015). Patients who have acute dental problems are more likely to be prescribed antibiotics by GPs compared with dentists, as shown in a comparative study of the management of dental conditions by GPs and dentists using standard consultation data (Anderson et al. 2000). Furthermore, a retrospective cohort study using a database of patient records in the UK showed that more than half the consultations by GPs for dental consultations resulted in antibiotic prescription (Cope et al. 2016a).
Factors, such as patient expectations and the perceived need for antibiotics by patients, are some of the reasons that influence GPs’ prescribing behaviour when using antibiotics for dental conditions (Cope et al. 2018). In addition, a patient study found that dissatisfaction with dental care, dental anxiety and self-diagnosis of dental infections were factors that have influenced antibiotic prescription by GPs (Cope et al. 2015).
Ultimately, inappropriate use of antibiotics contributes to the global public health problem of antimicrobial resistance, which accounts for 700,000 deaths worldwide annually (IACG 2019). Understanding behavioural reasons for antibiotic prescription can lead to the development of interventions to assist with appropriate prescribing. There is a lack of research exploring the reasons influencing antibiotic prescription by GPs for patients with dental conditions in Australia. Thus, our study aimed to explore the perceptions and factors of GPs towards managing dental presentations in Australia.
Methods
Theory
In this study, we applied the Theoretical Domains Framework (TDF; Michie et al. 2005) and the COM-B model to inform data analysis (Michie et al. 2011). This framework was chosen as a behavioural approach is needed to understand GPs’ perceptions when managing dental presentations. This can then inform researchers and guide future research to develop better interventions. The TDF consisted of 14 theoretical domains derived from 128 constructs. This framework has been used to design research studies, such as treatment pathways (Scott et al. 2013), improving uptake, and understanding behaviours around vaccinations (Painter et al. 2010; Biezen et al. 2018) and antimicrobial stewardship in general practice (Biezen et al. 2017). The COM-B model is centred around how the three essential conditions (Capability, Opportunity and Motivation) are needed to change behaviour (Michie et al. 2011).
Design
This was a cross-sectional qualitative study comprising semi-structured interviews with GPs in Victoria, Australia. Ethics approval was obtained by The University of Melbourne Human Ethics Sub-Committee (2022-25002-33041-3).
Participants and recruitment
GPs were recruited through advertisements using the Victorian primary care practice-based Research and Education Network (VicREN), and through the research team’s professional network and snowball sampling technique.
GPs were included if they currently worked in general practice in Victoria, and see patients presenting with a dental complaint at least once per month. A purposive sample of GPs was selected to ensure a range of demographics was included, including sex, range of years of clinical experience, varied socioeconomic index for areas (SEIFAs) and locality of urban or rural workplace locations.
Procedure
Interview questions were developed from literature reviews (Cope et al. 2015, 2018), as well as the clinical experience of the research team to identify key themes around antibiotic prescribing and GPs’ management of patients presenting with dental issues (interview guide in Supplementary Data 1). Interview questions were around the knowledge of management of dental conditions, education and training, thoughts on strategies to improve oral health, and their perceptions on why patients attend medical care for dental treatment. The interview questions were piloted with two GPs and refined based on their feedback. These pilot data were not included in the final analysis.
Interviews (ranged between 12 and 38 minutes) were conducted between October 2022 and January 2023, over the video conferencing platform, Zoom, by LT and AL. Written consent was obtained prior to the interview. GPs were reimbursed for their time with a gift voucher (valued at 100 AUD) upon the completion of the interview. Interviews were conducted until data saturation was achieved.
Analysis
Interviews were digitally recorded and transcribed verbatim by AL. Two researchers (RB and AL) read the first transcript independently, and generated initial codes and themes. The researchers then compared and refined the codes and themes until consensus was reached through discussion. A further two transcripts were coded, compared and refined. The process was repeated until all transcripts were analysed. The codes were matched to the domains within the TDF and mapped to the COM-B model where the themes were generated. Data were managed using NVivo (ver. 12, QSR International).
Results
Twelve GPs participated in the semi-structured interviews. Of those, 50% were men. Participants had an average of 13.3 years of clinical experience ranging between 2 and 37 years. Seven GPs worked in rural areas, and there was an even spread of SEIFA for workplace locations. Demographic details of the participating GPs are shown in Table 1.
| Participant ID | Sex | Years of experience | Postcode of workplace | Rural/urban | SEIFA decile (1–10) | |
|---|---|---|---|---|---|---|
| GP1 | Male | 7 | 3737 | Rural | 2 | |
| GP2 | Female | 22 | 3123 | Urban | 10 | |
| GP3 | Male | 6 | 3057 | Urban | 9 | |
| GP4 | Female | 2 | 3191 | Urban | 10 | |
| GP5 | Male | 3 | 3031 | Urban | 5 | |
| GP6 | Female | 6 | 3166 | Urban | 8 | |
| GP7 | Female | 2 | 3076 | Rural | 4 | |
| GP8 | Male | 8 | 3810 | Rural | 5 | |
| GP9 | Male | 37 | 3219 | Rural | 1 | |
| GP10 | Female | 13 | 3551 | Rural | 8 | |
| GP11 | Female | 30 | 3551 | Rural | 8 | |
| GP12 | Male | 23 | 3551 | Rural | 8 |
SEIFA, socioeconomic index for areas; (1–10), 1 = lowest SEIFA, 10 = highest SEIFA.
The most common dental presentation encountered by GPs was dental pain, but other presenting complaints, such as broken teeth, dry socket, dental caries, facial swelling and ulcers, were also reported.
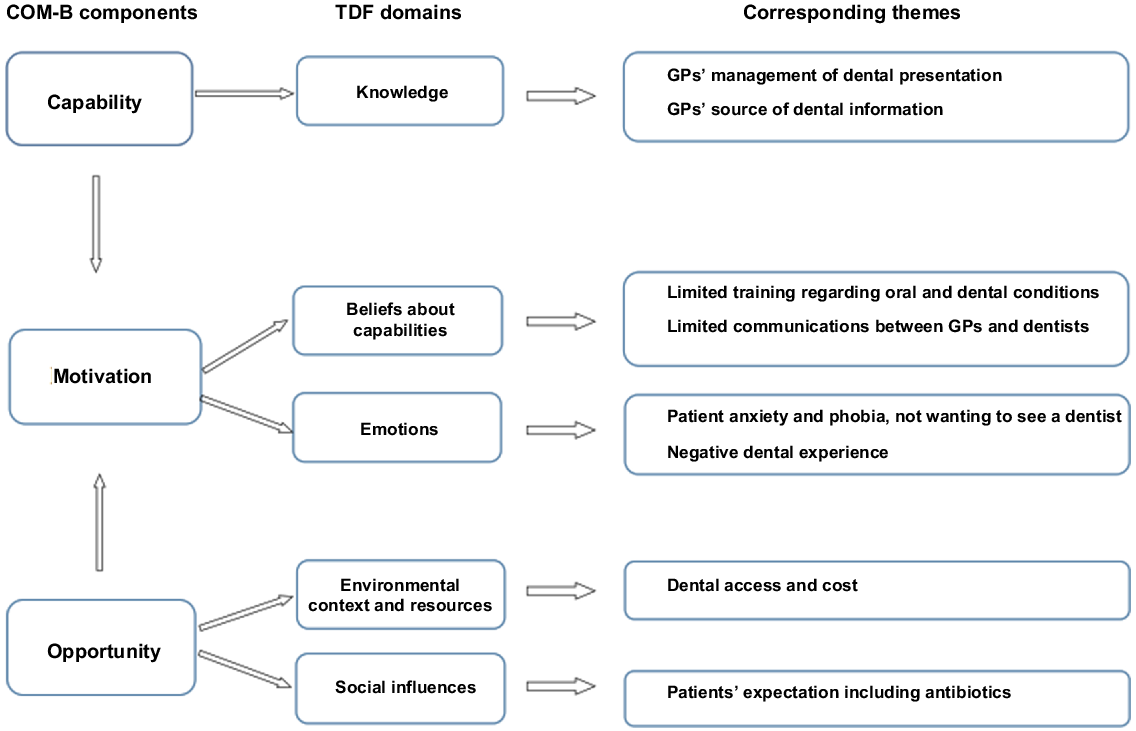
Six domains from the TDF across five themes were identified: knowledge, beliefs about capabilities, emotion, environmental context and resources, and social influences and social professional role and identity. Fig. 1 showed the relationship between the identified themes from the TDF mapped onto the COM-B model.
Theme 1: Capability – knowledge
All GPs acknowledged that dental treatment by a dental practitioner is needed to resolve most dental issues. Therefore, GPs would often provide temporary treatment to alleviate symptoms, but refer patients to seek dental care. Antibiotics were usually prescribed, in addition to the recommendation and referral to attend a dentist.
I would always emphasise that … even if the pain goes away with antibiotics, it is not necessarily the end of it. There may still be an underlying problem that needs sorting out through the dentist. (GP2)
I’ll usually prescribe them antibiotics and ask them to see a dentist after kind of they started the antibiotics to kind of sort out any kind of presumed dental infection(s). (GP3)
Amoxicillin was the most common antibiotic prescribed by GPs in this study, with pain relief also prescribed in some cases.
The national Australian dental guidelines, Therapeutic Guidelines and HealthPathways (a local Australian resource aimed for general practice; Therapeutic Guidelines 2019; HealthPathways 2023), were the most commonly cited resources that GPs use for guidance on managing dental conditions.
Theme 2: Motivation – beliefs about capabilities
Although guidelines were often used, and considered as important to manage dental conditions, GPs thought they only had basic knowledge of oral health, as they received limited training regarding oral and dental conditions.
There hasn’t been a lot of dentistry done, a little bit in my GP training … about the kind of acute presentations and emergencies things that we should know and do, but that I don’t feel like I have a great understanding of this part of the mouth … the teeth. (GP7)
GPs believed that dental treatment is usually required by a dentist, and acknowledged they had limited treatment options available to them, therefore reporting having reduced confidence in managing dental presentations.
GP is not able to manage anything else about it anyway and provide a script. (GP2)
And then … it’s the question about antibiotics or not, which I think a lot of GPs find a bit tricky. And … I don’t always feel 100% confident in making that judgement. (GP7)
Communication between GPs and dentists was limited, with some GPs stating that they would prefer to have better communication pathways with dentists to improve the management of their patients’ overall health conditions, similar to their interactions with other allied health professionals.
I suppose just have better communication with the dentist, perhaps have the sense of the dentist and us being part of the same care team for a patient … certainly we’d benefit from … there’d be a lot that I could learn from dentists … the dentist might benefit from some information from me about my patient’s health … I think it makes sense that we should be communicating and calling on each other for advice. (GP7)
Furthermore, some GPs reported that patients were advised by their dentist to obtain antibiotics from their GP first, prior to seeing the dentist. The initiation of antibiotics from the dentist was expressed by several participants in this study.
They say, I tried to get hold of them, and they say, come in to see the GP for some antibiotics first. (GP1)
So often a common story … and they been instructed [by the dentist] … I don’t know how true it is, but they say they were told to go and get some antibiotics, and then book into the dentist. (GP10)
Theme 3: Motivation – emotion
GPs expressed that dental anxiety and phobia were reasons behind patients’ delay and/or avoiding seeing a dentist. Due to this, GPs were unsure if patients would seek dental care, despite recommend patients to see a dentist after GPs’ treatment.
I have patients who have dental anxiety, and are afraid to go and see the dentist. (GP10)
Phobia is definitely, there are one or two patients that really don’t want to see the dentist, but they always say that they’ll book in to see the dentist, but I know that they won’t. (GP3)
Negative past experiences and poor oral health were reasons GPs suggested why some patients were unwilling to see a dentist. Some of these might have resulted in patients having preconceived assumptions as to the treatment that will be provided.
You know, I think for some people who … perhaps don’t have great oral health … they’ve potentially had experiences where they’ve been made to feel quite ashamed, or, you know have had quite difficult experiences with dentistry. So … I suspect that some patients are a little reluctant to go to the dentist, and perhaps coming to the GP … can feel a little bit safer. (GP7)
It’s the people that don’t have a regular dentist that may be afraid of the dentist or have preconceived ideas that ‘if I go to the dentist, they are going to pull my tooth out’. (GP2)
Theme 4: Opportunity – environmental context and resources
GPs reported dental care access is an issue for patients, particularly those working in locations with lower SEIFAs or requiring dental care from community public dental practices. Long patient waiting lists and the inaccessibility of timely dental care were common barriers.
I think that’s really pretty big for, for a lot of patients and the public dentistry is just so limited … the community dentistry … there are quite long wait times … the access could still be better, I think. (GP7)
Even access to community dentists … in any health services is very difficult as well … access to the dentistry I think is a significant issue in Australia and certainly in my experience as a GP. (GP9)
Cost was also a factor identified by several GPs that presented a barrier for patients seeking dental care.
… I really get the impression that a lot of it is around cost … people not seeing them … because it’s another thing that you have to pay … (GP6)
I’m dealing with a lot of … people who have a Health Care Card and pension card, living in public housing, can’t afford to see a dentist, don’t have money to have private insurance. (GP5)
GPs reported that the structure of dental care provision in comparison with primary medical care may also influence patients attending the GP instead of the dentist. This is due to the subsidisation of primary general medical care under the federal Medicare scheme, whereas most dentistry is provided by private dental clinics.
If it was under like a bulk billed Medicare, then I think a lot more people will be flocking to dentists. (GP6)
No Medicare rebate to see a dentist, so I think significant proportion of my patients with dental pain have been on Health Care Cards and haven’t got … sufficient funds to be able to pay for a private dentist, and so they will try and manage it themselves with seeing a GP… getting analgesics and antibiotics. (GP9)
However, for GPs who worked in more affluent locations, cost was not a major consideration that influenced dental management for patients.
Cost can be a barrier, I guess, for a few patients. Generally not too much. I’m lucky in that my clinic has a good socioeconomic kind of basis for its patients. (GP3)
Theme 5: Opportunity – social influences/social professional role and identity
Patients’ past experiences influenced their perception that antibiotics were necessary to cure their dental ailments. Some GPs reported that they encountered patients who believed antibiotics were an appropriate treatment for their dental infection.
They might test it out and see if antibiotic makes it better or not. Hopefully not, but if the pain gets better, they’d believe that antibiotics cure the infection. Therefore, when they have pain the next time, they will ask and come in again for antibiotics. So, it is like a reinforcement. (GP5)
I’ve actually had quite a few issues with patients in the past been quite insistent on wanting antibiotics. Because, you know, they’ve had this before … and was given antibiotics. Or I know I have an infection; I need some antibiotics. (GP6)
Patient expectations for antibiotics were also another factor leading to GPs feeling pressured to prescribe antibiotics. This misconception by patients regarding the use of antibiotics for other types of infections also applied to dentistry.
I think there is an expectation. But I think people often equate pain to infection, which is often the case in other parts of the body. If you have pain or swelling on the skin, it might be an infected boil or abscess that might need an antibiotic. So, they probably have that expectation when it comes to dental issues as well. (GP2)
Additionally, GPs reported that some patients would self-manage their dental infection and pain with antibiotics, similar to other medical conditions.
I suspect there would already be some self-treatment for dental pain that goes away or might have gone away without the antibiotic anyway … they definitely do that for other medical illnesses, so there’s no reason why they wouldn’t. (GP3)
GPs realised that patients would rather seek help through their GP, or even self manage their dental problems, than go to a dental practitioner to resolve their dental issues. They were therefore inclined to manage their patient care as much as possible.
Discussion
In this qualitative study exploring GPs’ management and antibiotic prescribing for dental conditions in Australia, we identified several factors that affected patients, clinicians, as well as system-related factors that influenced antibiotic prescribing for patients presenting with dental conditions. Factors, such as dental anxiety, past experiences with dental care and expectations for antibiotics by patients, influenced prescribing, whereas GPs reported factors, such as education and knowledge of management of dental conditions, influenced prescribing. Finally, difficulties in accessing and affordability of dental care in Australia underscored antibiotic prescribing for dental conditions, particularly for GPs who worked in areas with lower socioeconomic status. The findings of this study provide a basis for targeted interventions to improve the use of antibiotics for dental conditions in general practice, and highlights the importance of timely and affordable access to dental care.
GPs in this study reported limited training on the management of dental conditions. This is a concern, as GPs can be the first health professionals that patients see for oral and dental problems (Biniecki et al. 2018). Other studies have also found that GPs felt they received insufficient or no formal training regarding dental conditions, in both Australia as well as other countries (Trivedy et al. 2012; Nagarakanti et al. 2013; Cope et al. 2015; Biniecki et al. 2018; Yeng et al. 2020). Aside from their medical degree, GPs have indicated they gained education on dental problems by interaction with dental colleagues, private study and by their own personal dental experiences (Biniecki et al. 2018). It is therefore imperative that GPs are provided with the necessary resources required to manage patients with dental conditions.
Although it was shown that GPs do prescribe antibiotics for dental conditions, they also recognised that antibiotics are not a definitive treatment for these patients, and dental referral is needed (Biniecki et al. 2018). However, GPs from this study mentioned cost and access to dental care, especially those living in the lower socioeconomic areas, were some of the barriers for their patients. A comparative study in Western Australia showed that patients who lived in rural and remote areas were 14% and 27% less likely to see a dentist compared with urban patients, respectively, demonstrating that geographical location is a factor in the ability to access dental services (Adams et al. 2004). In addition to the long waiting lists of up to 2 years to access routine dental care, difficulties in navigating and accessing the public dental system, and understanding the availability of access for emergency dental care can be confusing (AIHW 2018; Stormon et al. 2021). The importance of access to oral health services is recognised in prevention of oral diseases and to reduce unnecessary antibiotic use for dental conditions (Thompson et al. 2020). In addition, affordability of dental treatment is reported to be a barrier for patients by our GPs in this study, especially those from lower SEIFA locations. Certainly, a population-based study spanning a decade of Western Australian children and adolescents showed that 43,937 children were hospitalised due to oral conditions, with much higher percentages of children who lived in disadvantaged locations (Alsharif et al. 2015).
Self-management of dental pain with antibiotics and analgesics by some patients has been documented in the literature, and was also reported by GPs in the present study. In Sharjah, United Arab Emirates, a cross-sectional study showed that 70.7% of 566 patients who attended the University Dental Hospital practice self-medicated for oral health problems (AlQahtani et al. 2019). Similarly, another cross sectional, hospital-based study of patients in Nepal showed that almost 63% of 265 patients reported self-managing toothaches, mostly with analgesics and antibiotics (Bhattarai et al. 2020). In addition, a cross-sectional study of dental patients in Malaysia showed that patients who practice self-medication had firmer views about the benefits of medications and were less likely to perceive medicines as harmful (Mittal et al. 2018). These findings collectively underscore the benefit of public education in appropriate medication use for dental problems.
Initiation of antibiotic prescriptions for patients by their GP, but on recommendation by the dentist, prior to attending their dental appointment, was a novel finding in this study that has not been previously documented in the literature. A cross-sectional study exploring the appropriateness of dental antibiotic prescribing choices by GPs in Victoria, Australia, showed only approximately 27% were in accordance with guidance (Teoh et al. 2023). This is similar to inappropriate dental antibiotic prescribing, with up to 80% of dental antibiotics being overprescribed for both therapeutic and prophylactic reasons (Cope et al. 2016b; Suda et al. 2019; Teoh et al. 2019). Inappropriate use of antibiotics by prescribers is important in the context of antibiotic resistance, and the findings of this study reinforce that dentists are also important targets for antibiotic stewardship interventions.
The diversity of the demographics of the participating GPs was a strength of this study, with a balanced representation of sex, workplace locality and varied SEIFAs, which collectively increases the validity of the results. However, one limitation was that only GPs in Victoria were included, and as public dental care is state funded, the identified barriers to accessing dental care may not be generalisable to all patients and GPs around Australia. Nonetheless, the provision of dental care through both the public and private sectors is similar nationally. As such, more research should be targeted to the specific barriers identified in this study. As patient factors were a predominant theme that evolved from this study that influence antibiotic prescription by GPs, co-designed educational interventions for patients may be one option to improve patient-driven antibiotic prescription. Interviewing patients to further understand and explore their perceptions towards seeking dental care from GPs would also enhance the findings from this study.
Conclusion
In this study, factors that influenced antibiotic prescribing by GPs were identified. These included patients’ anxiety and expectations for antibiotics, GPs’ knowledge and education in dental conditions, and patients’ cost and access to dental care. Future interventions can target these barriers to improve the use of antibiotics for these conditions, including targeting patient and GP education about the use of antibiotics for dental presentations.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declaration of funding
Leanne Teoh received a National Health and Medical Research Council Investigator grant (ID: 2016647), and Angel Leong received support from the Honours program at Melbourne Dental School, University of Melbourne. Neither of the funders have any involvement with the manuscript.
References
Adams C, Slack-Smith L, Larson A, O’Grady M (2004) Dental visits in older Western Australians: a comparison of urban, rural and remote residents. Australian Journal of Rural Health 12, 143-149.
| Crossref | Google Scholar | PubMed |
AIHW (2018) A discussion of public dental waiting times information in Australia: 2013–14 to 2016–17. Available at https://www.aihw.gov.au/reports/dental-oral-health/discussion-of-public-dental-waiting-times/summary [Accessed 28 May 2023]
AIHW (2022) Oral and dental care in Australia. Costs. Available at https://www.aihw.gov.au/reports/dental-oral-health/oral-health-and-dental-care-in-australia/contents/costs
AlQahtani HA, Ghiasi FS, Zahiri AN, Rahmani NI, Abdullah N, Al Kawas S (2019) Self-medication for oral health problems among adults attending the University Dental Hospital, Sharjah. Journal of Taibah University Medical Sciences 14, 370-375.
| Crossref | Google Scholar | PubMed |
Alsharif AT, Kruger E, Tennant M (2015) Dental hospitalization trends in Western Australian children under the age of 15 years: a decade of population-based study. International Journal of Paediatric Dentistry 25, 35-42.
| Crossref | Google Scholar | PubMed |
Anderson R, Calder L, Thomas DW (2000) Antibiotic prescribing for dental conditions: general medical practitioners and dentists compared. British Dental Journal 188, 398-400.
| Crossref | Google Scholar | PubMed |
Bhattarai R, Khanal S, Shrestha S (2020) Prevalence of self-medication practices for oral health problems among dental patients in a dental college: a descriptive cross-sectional study. Journal of the Nepal Medical Association 58, 209-213.
| Crossref | Google Scholar | PubMed |
Biezen R, Brijnath B, Grando D, Mazza D (2017) Management of respiratory tract infections in young children – a qualitative study of primary care providers’ perspectives. npj Primary Care Respiratory Medicine 27, 15.
| Crossref | Google Scholar | PubMed |
Biezen R, Grando D, Mazza D, Brijnath B (2018) Why do we not want to recommend influenza vaccination to young children? A qualitative study of Australian parents and primary care providers. Vaccine 36, 859-865.
| Crossref | Google Scholar | PubMed |
Biniecki E, Foote C, Gilbert G, Abbott P (2018) General medical practitioners’ knowledge and management of oral and dental problems. Australasian Medical Journal 11, 390-396.
| Crossref | Google Scholar |
Cope AL, Wood F, Francis NA, Chestnutt IG (2015) General practitioners’ attitudes towards the management of dental conditions and use of antibiotics in these consultations: a qualitative study. BMJ Open 5, e008551.
| Crossref | Google Scholar | PubMed |
Cope AL, Chestnutt IG, Wood F, Francis NA (2016a) Dental consultations in UK general practice and antibiotic prescribing rates: a retrospective cohort study. British Journal of General Practice 66, e329-e336.
| Crossref | Google Scholar | PubMed |
Cope AL, Francis NA, Wood F, Chestnutt IG (2016b) Antibiotic prescribing in UK general dental practice: a cross-sectional study. Community Dentistry and Oral Epidemiology 44, 145-153.
| Crossref | Google Scholar | PubMed |
Cope AL, Wood F, Francis NA, Chestnutt IG (2018) Patients’ reasons for consulting a GP when experiencing a dental problem: a qualitative study. British Journal of General Practice 68, e877-e883.
| Crossref | Google Scholar | PubMed |
HealthPathways (2023) HealthPathways Melbourne. Available at https://melbourne.communityhealthpathways.org/LoginFiles/Logon.aspx?ReturnUrl=%2f
IACG (2019) No time to wait: securing the future from drug-resistant infections. Report to the Secretary-General of The United Nations. (Interagency Coordination Group on Antimicrobial Resistance) Available at https://www.who.int/docs/default-source/documents/no-time-to-wait-securing-the-future-from-drug-resistant-infections-en.pdf
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A (2005) Making psychological theory useful for implementing evidence based practice: a consensus approach. Quality and Safety in Health Care 14, 26-33.
| Crossref | Google Scholar |
Michie S, van Stralen MM, West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science 6, 42.
| Crossref | Google Scholar | PubMed |
Mittal P, Chan OY, Kanneppady SK, Verma RK, Hasan SS (2018) Association between beliefs about medicines and self-medication with analgesics among patients with dental pain. PLoS ONE 13, e0201776.
| Crossref | Google Scholar | PubMed |
Nagarakanti S, Epari V, Athuluru D (2013) Knowledge, attitude, and practice of medical doctors towards periodontal disease. Journal of Indian Society of Periodontology 17, 137-139.
| Crossref | Google Scholar | PubMed |
Nguyen S, Ahmed L, Villarosa A, George A, Yaacoub A (2023) The use of antibiotics in acute oral health patients presenting at public dental clinics in the Western Sydney region. Family Practice 40, 9-15.
| Crossref | Google Scholar | PubMed |
Painter JE, Sales JM, Pazol K, Grimes T, Wingood GM, DiClemente RJ (2010) Development, theoretical framework, and lessons learned from implementation of a school-based influenza vaccination intervention. Health Promotion Practice 11, 42S-52S.
| Crossref | Google Scholar | PubMed |
Park JS, Page AT, Shen P-H, Price K, Tennant M, Kruger E (2022) Management of dental emergencies amongst Australian general medical practitioners – a case-vignette study. Australian Dental Journal 67, 30-38.
| Crossref | Google Scholar | PubMed |
Scott SE, Walter FM, Webster A, Sutton S, Emery J (2013) The model of pathways to treatment: conceptualization and integration with existing theory. British Journal of Health Psychology 18, 45-65.
| Crossref | Google Scholar |
Sen Gupta T, Stuart J (2020) Medicine and dentistry: shall ever the twain meet? Australian Journal of General Practice 49, 544-548.
| Crossref | Google Scholar | PubMed |
Stormon N, Sowa PM, Anderson J, Ford PJ (2021) Facilitating access to dental care for people experiencing homelessness. JDR Clinical & Translational Research 6, 420-429.
| Google Scholar | PubMed |
Suda KJ, Calip GS, Zhou J, Rowan S, Gross AE, Hershow RC, Perez RI, McGregor JC, Evans CT (2019) Assessment of the appropriateness of antibiotic prescriptions for infection prophylaxis before dental procedures, 2011 to 2015. JAMA Network Open 2, e193909.
| Crossref | Google Scholar | PubMed |
Teoh L, Marino RJ, Stewart K, McCullough MJ (2019) A survey of prescribing practices by general dentists in Australia. BMC Oral Health 19, 193.
| Crossref | Google Scholar | PubMed |
Teoh L, Hopcraft M, McCullough M, Manski-Nankervis J-A, Biezen R (2023) Exploring the appropriateness of antibiotic prescribing for dental presentations in Australian general practice – a pilot study. British Journal of Clinical Pharmacology 89, 1554-1559.
| Crossref | Google Scholar | PubMed |
Trivedy C, Kodate N, Ross A, Al-Rawi H, Jaiganesh T, Harris T, Anderson JE (2012) The attitudes and awareness of emergency department (ED) physicians towards the management of common dentofacial emergencies. Dental Traumatology 28, 121-126.
| Crossref | Google Scholar | PubMed |
WHO (2022) Global oral health status report: towards universal health coverage for oral health by 2030. World Health Organization, Geneva. Available at https://www.who.int/publications/i/item/9789240061484
Yeng T, O’Sullivan AJ, Shulruf B (2020) Medical doctors’ knowledge of dental trauma management: a review. Dental Traumatology 36, 100-107.
| Crossref | Google Scholar | PubMed |