The evaluation of the Plan–Do–Study–Act cycles for a healthcare quality improvement intervention in primary care
Deborah Manandi A * , Qiang Tu A , Nashid Hafiz A , Rebecca Raeside A , Julie Redfern A B and Karice Hyun A C
A * , Qiang Tu A , Nashid Hafiz A , Rebecca Raeside A , Julie Redfern A B and Karice Hyun A C
A
B
C
Abstract
The Plan–Do–Study–Act (PDSA) cycle is an iterative framework that has been gaining traction in primary care for quality improvement. However, its implementation remains understudied. This study evaluated the completion, achievement of goal, content quality, and enablers and barriers associated with completion of high-quality PDSA cycles in cardiovascular disease management in general practices.
This study analysed data from intervention practices of the QUality improvement in primary care to prevent hospitalisations and improve Effectiveness and efficiency of care for people Living people with coronary heart disease (QUEL) study. Content quality of cycles was assessed using a scoring system created based on established criteria of ideal PDSA cycles in the healthcare context. Practice-level factors associated with completion and cycles achieving the planned goal were explored through logistic regression models, and with content quality score through linear regression model. Enablers and barriers were assessed using thematic analysis of practices’ responses to the PDSA sections.
Ninety-seven cycles were reported by 18/26 (69%) practices. Seventy-seven percent of the cycles were completed and 68% achieved the planned goal. Content quality was low, with a median score of 56% (interquartile interval: 44%, 67%). Odds of cycles that were completed and achieved what was planned increased by 3.6- and 9.6-fold, respectively, with more general practitioners (GPs) within practices. Content quality was higher by 15% with more GPs. Lack of interprofessional engagement was a barrier to implementation.
Cycles were well completed, but poor in content quality, with high variability between practices. Human or capital resources and organisational support may be critical for the completion and cycles achieving the planned goals.
Keywords: cardiovascular disease, chronic disease, coronary heart disease, general practice, PDSA, Plan–Do–Study–Act cycles, primary care, quality improvement, secondary prevention.
Introduction
Cardiovascular disease (CVD) remains a leading cause of death (Roth et al. 2020; Australian Institute of Health and Welfare 2023). A cohort study of 21 countries (n = 155 722) attributed over 70% of CVD-related deaths to modifiable risk factors (Yusuf et al. 2020). These risk factors include high blood pressure, high cholesterol level, smoking, poor diet, physical inactivity and excess alcohol consumption (Heart Research Institute 2023). Patients with CVD have reported a higher number of these risk factors than the remaining population (Australian Institute of Health and Welfare 2023); hence, they are at heightened risk of not only recurrent hospitalisations and premature death, but also significant disease, psychosocial and financial burden.
Primary care, given its accessibility for long-term management, is an ideal setting for ongoing CVD management (Redfern et al. 2012; Hespe et al. 2022; The Royal Australian College of General Practitioners 2022); that is, primary care practitioners can build rapport and provide patients with individualised support to manage CVD risk factors. However, there remains opportunities for improvement in primary care (National Heart Foundation of Australia 2015; Ali et al. 2017; Messom and Wells 2022). A narrative review suggested patients with access to a computerised primary care infrastructure practised better management of blood pressure level, and achieved a greater number of treatment goals (Gill et al. 2019; Lopez et al. 2019). Electronic health records (EHRs) have also been pervasively available across primary care (Ben-Assuli 2015); yet, they remain underutilised for computerising, monitoring or individualising patients’ CVD risk factors management (Hodgkins et al. 2020).
The growing promotion of quality improvement research are among efforts to achieve improvements in primary care (Backhouse and Ogunlayi 2020). Quality improvement research aims to implement systematic but cost-effective changes to improve patient experience or outcomes (Backhouse and Ogunlayi 2020). A flexible and iterative quality improvement method that has been gaining traction in general practices includes the Plan–Do–Study–Act (PDSA) cycle (Fig. 1) (Institute of Healthcare Improvement 2003; The Royal Australian College of General Practitioners 2010; Davidoff et al. 2015). In the ‘Plan’ stage, general practices would decide on a goal or a change to learn, test or implement. In the ‘Do’ stage, they would attempt and observe the change. In the ‘Study’ stage, the practices would learn from the results of the change. In the ‘Act’ stage, they would decide whether to re-test or implement the change (Langley et al. 2009). Since the 2017–19 triennium, completing PDSA cycles aimed at reviewing practices’ performance or measuring outcomes has been an eligible activity to cover for general practitioners’ (GPs) continuing professional development (CPD) requirements (The Royal Australian College of General Practitioners 2016, 2020, 2023). Fulfilling CPD requirements demonstrates GPs updating their knowledge, maintaining expertise and competence in their practices. The methodological criteria of ideal PDSA sections and cycles in the healthcare context have been detailed by Langley et al. (2009). However, past applications of PDSA cycles were often incompletely documented, and even the documented cycles often failed to conform to the methodological criteria (Taylor et al. 2014; Knudsen et al. 2019). The implementation of PDSA cycles in general practice remains largely understudied. Practice characteristics or local contexts that can influence the implementation of PDSA cycles have also yet to be identified (Kaplan et al. 2010; Reed and Card 2016).
Plan–Do–Study–Act cycles in collaborative quality improvement interventions (Institute of Healthcare Improvement 2003; Redfern 2022).
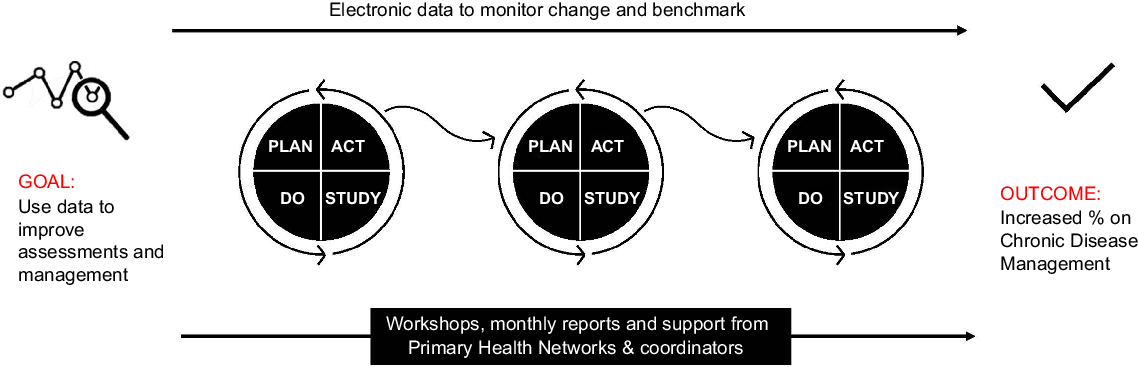
The QUality improvement in primary care to prevent hospitalisations and improve Effectiveness and efficiency of care for people Living people with coronary heart disease (QUEL) study is a cluster randomised trial of quality improvement intervention to reduce cardiac-related readmissions and improve secondary prevention. It recognised the value of flexible and iterative improvements for closing the evidence-practice gap in ongoing CVD management. As part of a data-driven quality improvement intervention, the participating general practices were encouraged to complete monthly PDSA cycles (Redfern et al. 2020). As a sub-study of the QUEL study, we aim to evaluate the completion, achievement of goal, content quality of the reported cycles, and enablers and barriers associated with completion of high-quality PDSA cycles in CVD management in Australian general practices.
Methods
Study design
Multi-method research was conducted to achieve the objective of this sub-study. In brief, the QUEL study is a cluster randomised controlled intervention that included 52 general practices across urban and rural Australia (Redfern et al. 2020). Twenty-six practices randomised to the intervention engaged in activities, including PDSA cycles, to achieve a series of change targets such as optimising EHRs, increasing prescriptions of cardioprotective medications and achievement of national risk-factor targets such as blood pressure, cholesterol and smoking. The study evaluates the effectiveness of the data-driven quality improvement intervention using unplanned hospital readmissions and cardiovascular risk factors at 12 and 24 months as outcomes (Redfern et al. 2020). A full protocol is published elsewhere (Redfern et al. 2020). Ethics approval for the study was obtained from the New South Wales Population and Health Services Research Ethics Committee (HREC/18/CIPHSS/44).
Data sources
Data were extracted from deidentified PDSA cycle data and practice characteristics were obtained from the intervention practices of the QUEL study. Practices were given the option to focus each PDSA cycle on one of four change principles; the first change principle: ‘understand your population’; second: ‘provide systematic and proactive care’; third: ‘implement self-management principles and support patient self-management’; and fourth: ‘ensure patients receive coordinated and integrated care’. Three sections, ‘Goal’, ‘Idea’ and ‘Measure’ were added to existing sections of a regular PDSA cycle (‘Plan’, ‘Do’, ‘Study’ and ‘Act’) to assist in planning the cycles. The practice characteristics collected included number of GPs, State (whether it is New South Wales (NSW), South Australia (SA) or Queensland (Qld) and Victoria (Vic.)), and rurality (whether it is rural or urban). Qualitative analyses were based on the practices’ responses to the PDSA sections. An example of the response is attached as Supplementary Table S1.
PDSA content quality score
A PDSA content quality score was developed based on the criteria proposed in the study by Langley et al. (2009) of ideal PDSA cycles in the healthcare context. The finalised content quality scoring indicator is attached as Supplementary Table S2. This score was used to assess the content quality of the reported cycles. Criteria of the ‘Plan’ section assessed whether cycles fulfilled criteria of an ‘objective’, ‘predictions of the answers to the questions’ and ‘plan to carry out the cycle’. Criteria of the ‘Do’ section assessed whether cycles fulfilled criteria of ‘carry out the plan’ and ‘documentation of problems or unexpected situations’. The criteria proposed in the study by Langley et al. (2009) recommends beginning analysis of the data in the ‘Do’ section; however, to better suit our study, we have assessed whether the practices looked at their data as part of carrying out the plan.
The ‘Study’ section assessed whether cycles fulfilled criteria of ‘compare data to predictions or plans’ and recorded ‘summary of what was learned’. Finally, criteria of the ‘Act’ section assessed whether the cycle fulfilled criteria of ‘future actions or changes to be made were postulated’ and ‘iteration planned or indicated to be needed’. Furthermore, additional questions were added to assess whether the responses were recorded in correct sections of the cycle and to capture iteration of cycles.
Outcomes
For this sub-study, four outcomes were explored: (i) completion of PDSA sections and overall cycles; (ii) achievement of planned goal; (iii) content quality of sections and cycles; and (iv) enablers and barriers associated with completion of high-quality cycles. Each PDSA section was considered complete if any response was recorded. PDSA cycles with 100% completion of all sections were categorised as ‘complete’, whereas remaining cycles were categorised as ‘incomplete’. PDSA cycles that documented any achievement of the planned improvement were categorised as ‘achieved goal’, whereas remaining cycles were categorised as ‘did not achieve goal’. Content quality was assessed using the created scoring system based on the criteria by Langley et al. (2009) criteria. The ‘Goal’, ‘Idea’ and ‘Measure’ sections were jointly scored with the ‘Plan’ section. Content quality was reported in percentages, out of the maximum of 18 points. The cycles were scored by two researchers (DM and QT), independently. Uncertain scores were resolved in consultation with two other researchers (NH and KH).
Analysis
The practice characteristics were compared by the completion status, whether the practices achieved the planned goal and the content quality of the cycle. The PDSA cycle characteristic was the four change principles. The practice characteristics were the number of GPs (≤5, 6 to 9 or ≥10), state (NSW, SA/Qld or Vic.) and rurality (rural or urban). Fisher’s exact test was used to compare the completion and achievement of goal by the categorical variables due to the low number of observations in each category. The median content quality was compared using the Wilcoxon rank-sum test to compare the categorical variable with two categories, and the Kruskal–Wallis test was used to compare variables with more than two categories. Multivariable logistic regressions were performed to identify variables associated with the completion status and whether cycles achieved the planned goal. Multivariable linear regression was performed to identify variables associated with increase in content quality. The threshold P-value for practice characteristics to be included in the models is <0.2. The PDSA characteristic also included in the model with the achievement of goal was median quality score. All quantitative statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
The qualitative analysis was performed by two researchers (DM and RR) independently. Following the thematic analysis method by Braun and Clarke (2006), researchers read through the practices’ responses to the PDSA sections to familiarise themselves with the data. Responses to the sections were then coded, and through a reflexive process were put into themes. The themes were then reviewed by both researchers together and combined or expanded until final themes were defined and named. Example textual data to support the final themes was extracted. Any disagreements were resolved in discussion with a third researcher (KH). All qualitative analyses were performed using NVivo version 12.6.1 (QSR International, Burlington, MA, USA).
Results
A total of 97 PDSA cycles were reported by 18 of the 26 (69%) general practices in the intervention arm. The number of PDSA cycles reported by the intervention practices ranged between 1 and 10. The median number of cycles reported was six (interquartile interval [IQI]: 3, 8).
Completion
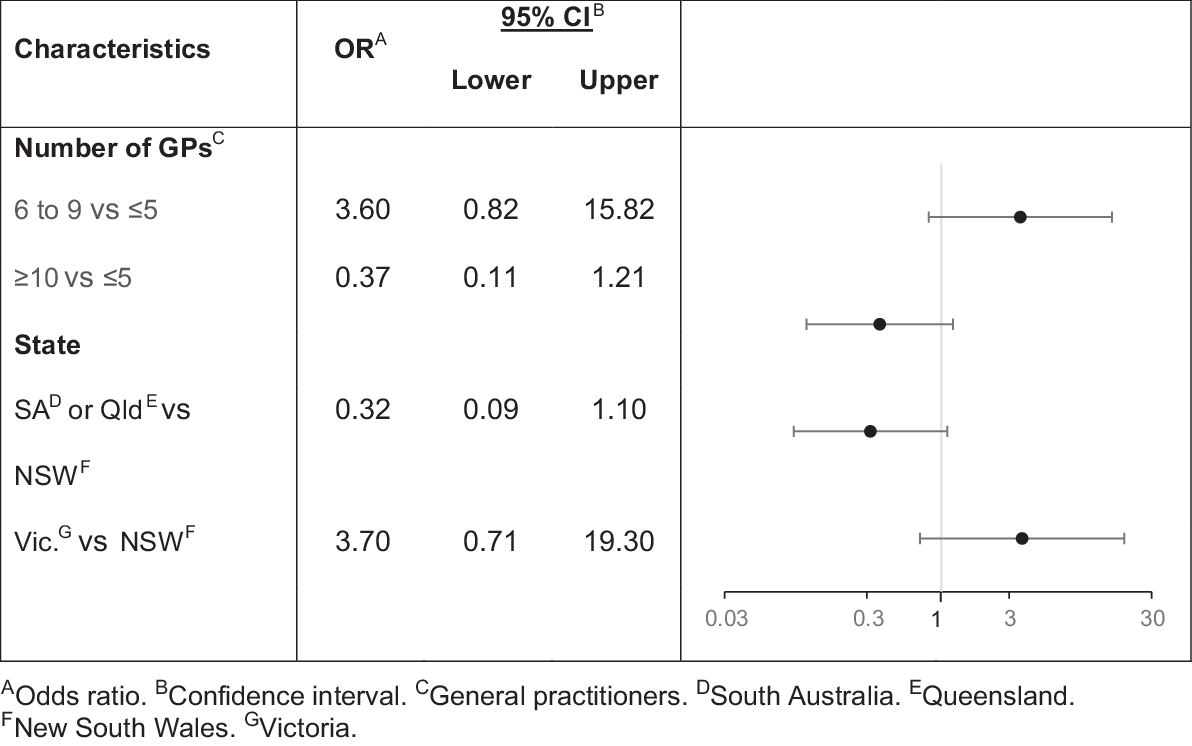
The completion of PDSA sections were generally high, but declined along the sections. The completion of ‘Goal’ was 97%, ‘Idea’ was 96%, ‘Measure’ was 96%, ‘Plan’ was 94%, ‘Do’ was 81%, ‘Study’ was 79% and ‘Act’ was 78%. The completion of each cycle ranged between 29% and 100% of sections. Of the 97 PDSA cycles, 75 cycles (77%) were categorised as ‘complete’, whereas the remaining 22 cycles (23%) were categorised as ‘incomplete’. The practices with less than 10 GPs were more likely to complete the cycles than practices with 10 GPs or more (P = 0.0145), and the completion rate varied across states (P = 0.0325) (Table 1). However, this was not significantly different across the change principle of cycles and rurality of practices. After adjustment, the number of GPs and state were found not to be significantly associated with completion status of cycles (Fig. 2).
| Characteristics | Total (n = 97) | Completion | Achievement of planned goal | Content quality | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Complete (n = 75) n (%) | Incomplete (n = 22) n (%) | P-value | Achieved goal (n = 66) n (%) | Did not achieve goal (n = 31) n (%) | P-value | Median (Q1 A, Q3 B) | P-value | |||
| Number of GPs C | ||||||||||
| ≤5 | 39 (40) | 30 (40) | 9 (41) | 0.0145 (*) | 21 (32) | 18 (58) | 0.0597 | 56 (39, 72) | 0.0013 (**) | |
| 6–9 | 34 (35) | 31 (41) | 3 (14) | 26 (39) | 8 (26) | 61 (50, 78) | ||||
| ≥10 | 24 (25) | 14 (19) | 10 (45) | 19 (29) | 5 (16) | 44 (17, 56) | ||||
| State | ||||||||||
| NSW D | 53 (55) | 41 (55) | 12 (55) | 0.0325 (*) | 34 (52) | 19 (61) | 0.1199 | 61 (44, 72) | <0.0001 (***) | |
| SA E or Qld F | 19 (20) | 11 (15) | 8 (36) | 11 (17) | 8 (26) | 44 (17, 44) | ||||
| Vic. G | 25 (26) | 23 (31) | 2 (9.09) | 21 (32) | 4 (13) | 67 (50, 78) | ||||
| Change principle | ||||||||||
| 1 | 39 (40) | 29 (39) | 10 (45) | 0.1995 | 23 (35 | 16 (52) | 0.142 | 56 (44, 72) | 0.3801 | |
| 2 | 35 (36) | 29 (39) | 6 (27) | 25 (38) | 10 (32) | 56 (39, 67) | ||||
| 3 | 6 (6) | 6 (8.00) | 0 (0.00) | 6 (9.09) | 0 (0.00) | 61 (44, 78) | ||||
| 4 | 14 (14) | 10 (13) | 4 (18) | 11 (17) | 3 (9.68) | 61 (17, 72) | ||||
| None chosen | 3 (3) | 1 (1.33) | 2 (9.09) | 1 (1.52) | 2 (6.45) | 44 (11, 44) | ||||
| Rurality | ||||||||||
| Urban | 83 (86) | 63 (84) | 20 (90.91) | 0.5134 | 56 (85) | 27 (87) | 1 | 56 (44, 67) | 0.0123 (*) | |
| Rural | 14 (14) | 12 (16) | 2 (9.09) | 10 (15) | 4 (13) | 78 (33, 89) | ||||
| Content quality | ||||||||||
| Median (Q1 A, Q3 B) | 56 (44, 67) | 61 (50, 72) | 17 (11, 22) | <0.0001 (***) | 58 (44, 72) | 39 (17, 67) | 0.0043 (**) | |||
Achievement of goal
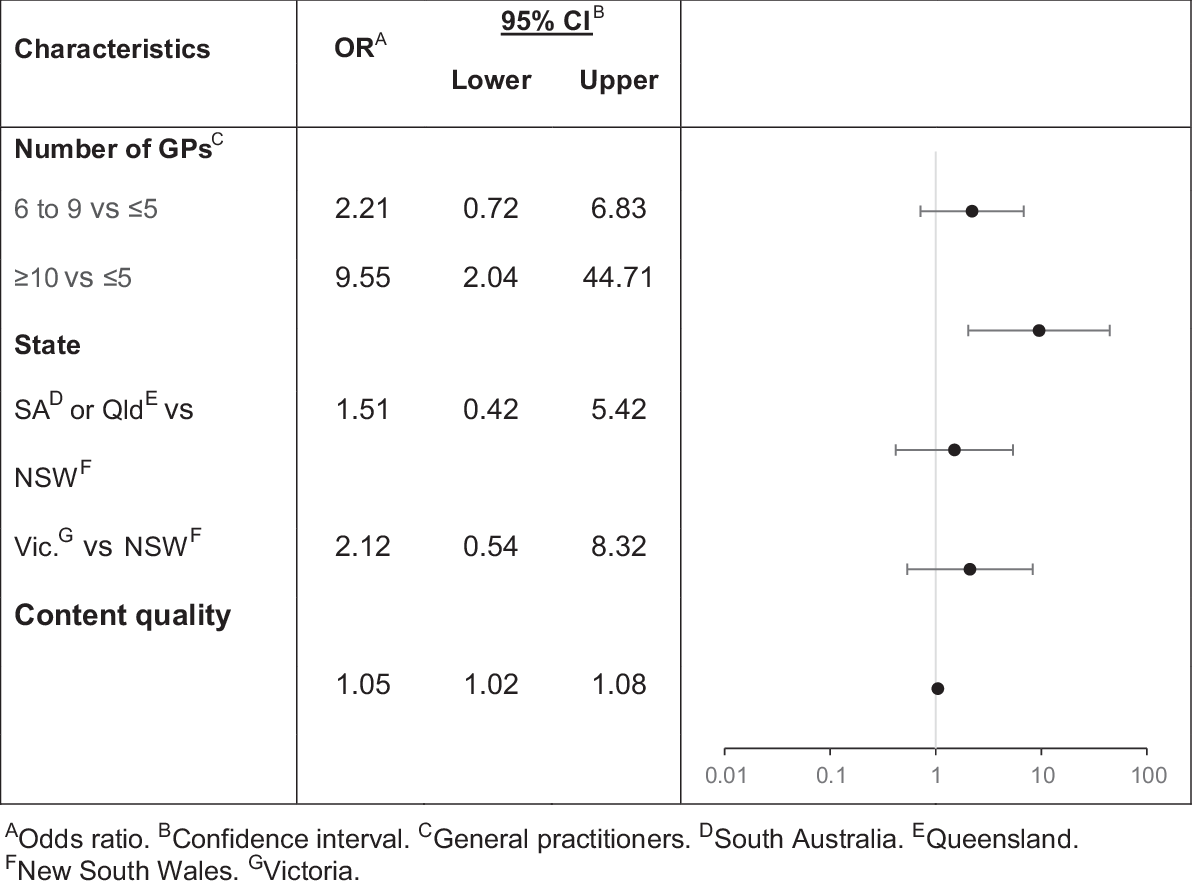
Of the 97 PDSA cycles, 66 cycles (68%) were categorised as ‘achieved goal’, whereas the remaining 31 cycles (32%) were categorised as ‘did not achieve goal’. The median content quality was higher in those who had achieved the planned improvement (P = 0.0043) of the cycles (Table 1). However, this was not significantly different across the number of GPs, state and rurality of practices, and change principle of cycles. Meanwhile, after adjustment, number of GPs ≥10 compared to ≤5, and content quality were found to be enablers significantly associated with whether cycles achieved the planned goal (Fig. 3).
Content quality
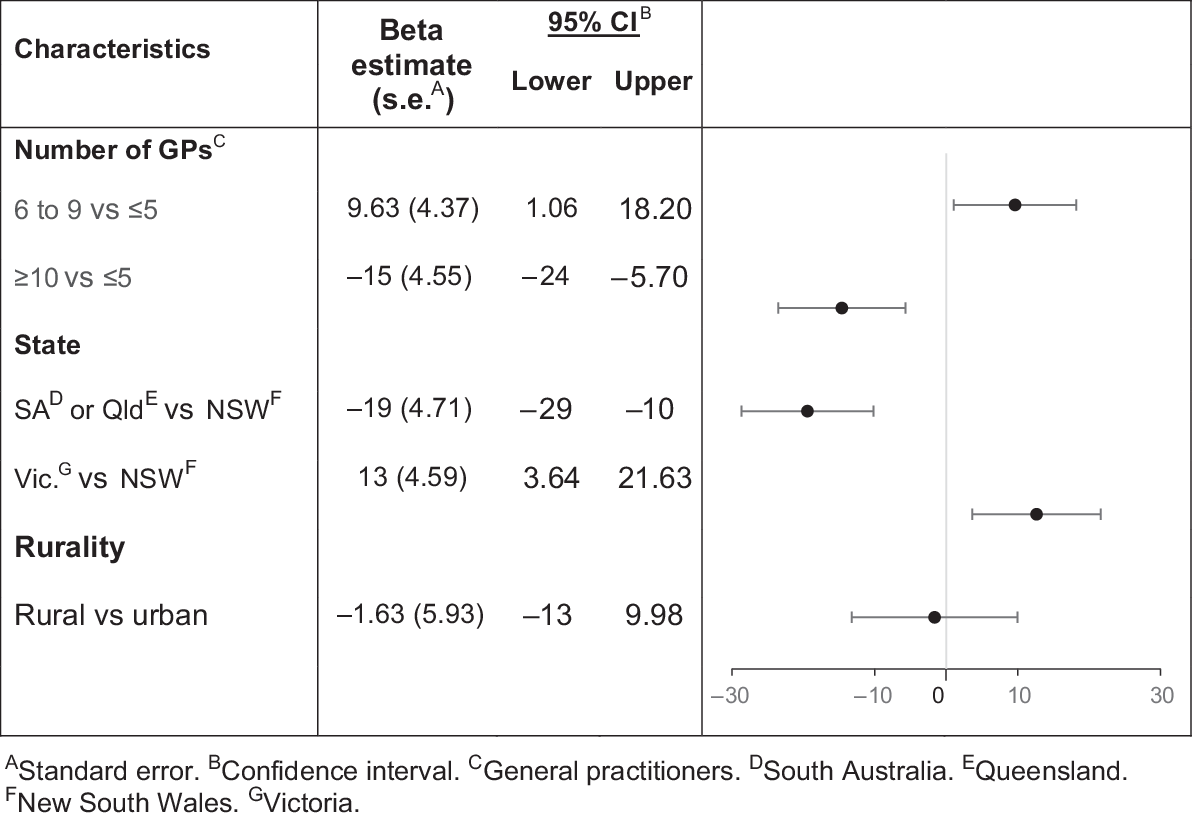
The median content quality of PDSA sections varied across the sections. The median content quality of ‘Plan’ was 60% (IQI: 40%, 60%), ‘Do’ was 50% (IQI: 25%, 50%), ‘Study’ was 67% (IQI: 33%, 100%), and ‘Act’ was 33% (IQI: 0%, 67%). The median content quality of additional questions was 67% (IQI: 33%, 67%). The content quality of the overall cycle ranged between 3% and 94%. The median content quality of all cycles was 56% (IQI: 44%, 67%). The median content quality was the highest from practices with six to nine GPs (P = 0.0013), in Vic. (P < 0.001) and rural areas (P = 0.0123) (Table 1); however, this was not significantly different across the change principle of cycle. From the adjusted linear regression analysis, number of GPs and state were found to be associated with the increase in content quality (Fig. 4).
Enablers and barriers to completion of high-quality cycles
From the qualitative analysis, thematic coding of content identified five barriers to complete high-quality PDSA cycles.
The practices workforce responsible for the cycles observed a lack of interprofessional engagement. For example, there was lack of response from GPs regarding patients who needed follow up. Consequently, some patients failed to be followed up and the patient data remained incomplete. This could pose as a barrier to attempt, observe or learn from results of a change, hence a barrier to complete high-quality cycles that achieve planned improvements.
Doctor’s never returned my reports so I could add recalls in clinical programme and have patients come in for review. (Practice M)
Lack of interprofessional engagement among the practices workforce could be attributed to the lack of shared accountability or motivation. Lack of shared accountability or motivation were potentially exacerbated by the high workload and consequent time constraints in practices.
Unfortunately, doctors either reluctant or too busy to review. Likely cause to lack of incentive to review. (Practice K)
Furthermore, the practices workforce responsible for the cycles also observed a lack of engagement from followed-up patients. Consequently, some patient data remained incomplete. This could pose as another barrier to complete high-quality cycles that achieve planned improvements.
18 were on our recall system and had received recall letters with no response. (Practice A)
Further organisational support such as continuing quality improvement training, professional development and support or regular meetings for health professionals were suggested strategies to build engagement, as well as capacity to analyse or utilise data.
Found since recruiting a nurse in July our results are starting to increase. (Practice M)
Encouraged doctors to look for missing data through Top Bar. Found they are starting to show interest. (Practice M)
The coronavirus disease 2019 (COVID-19) pandemic, bushfires and flooding around the commencement of the QUEL study significantly impacted Australian general practices. These unforeseen circumstances could have exacerbated the practices’ difficulty in engaging health professionals and patients, or time constraints.
With COVID-19, we ceased care plans for a period of time, then restarted with telehealth. (Practice A)
Due to COVID, bushfires, flooding and staffing levels I was unable to meet my goal by 5%. (Practice M)
Discussion
This current study was one of the first in-depth evaluation of PDSA cycles used for quality improvement in general practice. More than three-quarters of PDSA cycles analysed in this study recorded a response under all sections. However, the content quality of these cycles varied between 6% and 94%, with a median quality rate of 56%. Cycles that achieved the planned improvements and achieved higher content quality were more likely to be completed by general practices with a higher number of professionals more committed to quality improvement and maintain more accurate patient data. These results highlight how the PDSA cycles have been applied by general practices. The completion rate observed in this sub-study was considerably high. Past studies attributed incomplete documentation of PDSA cycles to the lack of rigorous reporting structure (Speroff et al. 2004; Taylor et al. 2014; Reed and Card 2016; Knudsen et al. 2019). This observed high completion rate confirms benefits of a more rigorous PDSA cycles structure in the QUEL study, such as the change principles and three additional ‘Goal’, ‘Idea’ and ‘Measure’ sections. However, the content quality observed in this sub-study were evidently low. Meanwhile, past studies attributed quality of PDSA cycles to the health professionals’ understanding of the core PDSA components (Reed and Card 2016). This observed poor content quality suggests the need for future quality improvement interventions to reinforce wider, continuous and cross-platform training to all health professionals within practices who might have a rostering schedule (Health Foundation 2012; Gosling et al. 2021; van Assen 2021). Training could also foster motivation and encourage formation of teams committed to quality improvement within practices.
Our study suggests that a higher number of GPs might have enabled the practices to achieve the planned goals of cycles. A higher number of GPs often signifies larger-sized practices with higher capital to navigate imprecise and incomplete patient data or unforeseen circumstances, and human resources with allocated time or clearer role for quality improvement (Wolfson et al. 2009; Reed and Card 2016; Swerissen et al. 2018; The Royal Australian College of General Practitioners 2018). Future quality improvement interventions could consider reducing the frequency of recommended PDSA cycles to complete, emphasising to practices with fewer number of GPs on the potential use of PDSA cycles for fulfilling CPD requirements, requesting more support from the Primary Health Networks or encouraging internal leadership for stronger project support. Furthermore, our study suggests that the stronger interprofessional engagement among time-constrained practice workforces might have further enabled the implementation of cycles.
The QUEL study included general practices from Vic. and SA, in addition to SA and Qld as detailed in the protocol. This protocol deviation carried no/minimal impact on the study implementation, quality of data and outcomes. However, there are several limitations to consider in this study. First, there were limited practice characteristics collected to assess whether they have a confounding effect on the outcomes of this current study. Second, there might have been a clustering effect on the completion and content quality of the PDSA cycles, as some practices might have been more committed to the use of the cycles than others. However, due to the low number of PDSA cycles provided by some practices, the clustering effect could not be accounted for in the analyses. Most importantly, this study was greatly limited by unforeseen circumstances, such as the COVID-19 pandemic, bushfire and flooding around the commencement of the QUEL study. These likely affected the reporting rate, completion, achievement of goal and content quality of cycles. Consequently, the effective implementation of the PDSA cycles in the primary healthcare setting could be underestimated. Further studies with varied study designs are therefore required to ultimately resolve the concerns regarding the validity, generalisability and overall effectiveness of PDSA cycles in general practices. In the current study, the implementation of PDSA cycles were explored. In future studies, the effect of quality cycles on clinical outcomes, including the reduction of CVD-related hospitalisation and death rates, ought to be assessed. A study is also needed to explore other possible barriers and enablers to complete high-quality cycles, which have not been captured in this study. Moreover, further validation of the content quality scoring indicator is needed to determine the appropriate quality categories (i.e. high, intermediate and low) and test its fidelity under other study or healthcare settings.
Conclusion
The current study suggests that although general practices can complete the PDSA cycles to a high rate, these cycles were not always completed to a sufficiently high content quality. However, completion, achievement of goal, content quality and implementation of these PDSA cycles varied between practices depending on local contexts, level of interprofessional engagement and technology or financial resources. Learnings drawn from this study can inform how to better implement the PDSA cycles and improve future quality improvement studies in health care. The structure employed in this study might also serve as a framework by which future PDSA cycles, including those reported for covering GPs’ CPD requirements, can be evaluated, which in doing so, can further contribute to the study of the PDSA cycles’ effectiveness and scalability in healthcare settings.
Data availability
The data that support this study cannot be publicly shared due to ethical or privacy reasons and may be shared upon reasonable request to the corresponding author if appropriate.
Declaration of funding
The QUEL study is a National Health and Medical Research Council (NHMRC) Partnership Project (APP1140807) and in-kind or cash support were received from Amgen, Austin Health, Australian Cardiovascular Health and Rehabilitation Association, Australian Commission on Safety and Quality in Health Care, Australian Primary Health Care Nurses Association, Brisbane South PHN, Fairfield General Practice Unit, Heart Support Australia, Improvement Foundation, Inala Primary Care, National Heart Foundation of Australia, Nepean Blue Mountains PHN, The Royal Australian College of General Practitioners, South Western Sydney PHN, The George Institute for Global Health and The University of Melbourne. This collaborative study also received cash support from Sanofi via the Externally Sponsored Collaboration pathway. DM is funded by a University of Sydney Tuition Fee Scholarship, SOLVE-CHD PhD Scholarship (SC3751) and a Faculty of Medicine and Health Postgraduate Research Supplementary Scholarship (SC4455). JR is funded by a NHMRC Investigator Grant (GNT2007946). KH is funded by an NHMRC Investigator Grant (GNT1196724).
Acknowledgements
The authors thank the general practices and primary health networks (PHNs) involved in the QUEL study. The authors thank investigators of the QUEL study: Andrew Knight, Charlotte Hespe, Clara Chow, Tom Briffa, Robyn Gallagher, Christopher Reid, David Hare, Nicholas Zwar, Mark Woodward, Stephen Jan, Emily Atkins, Tracy-Lea Laba, Elizabeth Halcomb and Tim Usherwood. The authors also thank Farzaneh Boroumand for assistance with the quantitative analyses.
References
Ali MA, Yasir J, Sherwani RN, Fareed M, Arshad F, Abid F, Arshad R, Ismail S, Khan SA, Siddiqui U, Muhammad MG, Fatima K (2017) Frequency and predictors of non-adherence to lifestyle modifications and medications after coronary artery bypass grafting: a cross-sectional study. Indian Heart Journal 69, 469-473.
| Crossref | Google Scholar | PubMed |
Australian Institute of Health and Welfare (2023) Heart, stroke and vascular disease: Australian facts. AIHW, Canberra. Available at https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts [Accessed 1 September 2023]
Backhouse A, Ogunlayi F (2020) Quality improvement into practice. BMJ 368, m865.
| Crossref | Google Scholar | PubMed |
Ben-Assuli O (2015) Electronic health records, adoption, quality of care, legal and privacy issues and their implementation in emergency departments. Health Policy 119, 287-297.
| Crossref | Google Scholar | PubMed |
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3, 77-101.
| Crossref | Google Scholar |
Davidoff F, Dixon-Woods M, Leviton L, Michie S (2015) Demystifying theory and its use in improvement. BMJ Quality & Safety 24, 228-238.
| Crossref | Google Scholar | PubMed |
Gill J, Kucharski K, Turk B, Pan C, Wei W (2019) Using electronic clinical decision support in patient-centered medical homes to improve management of diabetes in primary care: the DECIDE study. J Ambul Care Manage 42, 105-115.
| Crossref | Google Scholar | PubMed |
Gosling J, Mays N, Erens B, Reid D, Exley J (2021) Quality improvement in general practice: what do GPs and practice managers think? Results from a nationally representative survey of UK GPs and practice managers. BMJ Open Quality 10, e001309.
| Crossref | Google Scholar | PubMed |
Health Foundation (2012) Quality improvement training for healthcare professionals. The Health Foundation. Available at https://www.health.org.uk/sites/default/files/QualityImprovementTrainingForHealthcareProfessionals.pdf
Heart Research Institute (2023) Risk factors for cardiovascular disease. Available at https://www.hri.org.au/health/learn/risk-factors/risk-factors-for-cardiovascular-disease#:~:text=The%20main%20preventable%20risk%20factors,nutrition%20and%20excessive%20alcohol%20consumption. [Accessed 1 September 2023]
Hespe CM, Giskes K, Harris MF, Peiris D (2022) Findings and lessons learnt implementing a cardiovascular disease quality improvement program in Australian primary care: a mixed method evaluation. BMC Health Services Research 22, 108.
| Crossref | Google Scholar | PubMed |
Hodgkins AJ, Mullan J, Mayne DJ, Boyages CS, Bonney A (2020) Australian general practitioners’ attitudes to the extraction of research data from electronic health records. Australian Journal of General Practice 49, 145-150.
| Crossref | Google Scholar |
Institute for Healthcare Improvement (2003) The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. Institute of Healthcare Improvement: Massachusetts. Available at http://www.ihi.org/resources/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx
Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, Margolis P (2010) The influence of context on quality improvement success in health care: a systematic review of the literature. The Milbank Quarterly 88, 500-559.
| Crossref | Google Scholar | PubMed |
Knudsen SV, Laursen HVB, Johnsen SP, Bartels PD, Ehlers LH, Mainz J (2019) Can quality improvement improve the quality of care? A systematic review of reported effects and methodological rigor in plan-do-study-act projects. BMC Health Services Research 19, 683.
| Crossref | Google Scholar | PubMed |
Lopez PM, Divney A, Goldfeld K, Zanowiak J, Gore R, Kumar R, Laughlin P, Sanchez R, Beane S, Trinh-Shevrin C, Thorpe L, Islam N (2019) Feasibility and outcomes of an electronic health record intervention to improve hypertension management in immigrant-serving primary care practices. Medical Care 57(Suppl 6), S164-S171.
| Crossref | Google Scholar | PubMed |
Messom R, Wells L (2022) Strengthening Medicare and investing in Primary Health Care: a Roadmap for Reform. Consumers Health Forum of Australia, Australia. Available at https://chf.org.au/sites/default/files/17062022_strengthening_medicare_and_investing_in_primary_health_care_a_roadmap_for_reform_final.pdf [Accessed 4 September 2023]
National Heart Foundation of Australia (2015) Chronic disease prevention and management in primary care. Heart Foundation Submission to House of Representatives Standing Committee on Health, Sydney. Available at https://www.aph.gov.au/DocumentStore.ashx?id=fee944a8-5c73-45a3-a92a-fb72906a38e3&subId=402231
Redfern J, Chow C, Brieger D, Briffa T, Chew D, Ferry C, Leeder S, Peiris D, Turnbull F (2012) National Secondary Prevention of Coronary Disease Summit. The George Institute for Global Health Technical Report, Sydney. Available at https://www.georgeinstitute.org/sites/default/files/documents/events/coronary-disease-summit-2011-report.pdf
Redfern J, Hafiz N, Hyun K, Knight A, Hespe C, Chow CK, Briffa T, Gallagher R, Reid C, Hare DL, Zwar N, Woodward M, Jan S, Atkins ER, Laba T-L, Halcomb E, Billot L, Johnson T, Usherwood T (2020) QUality improvement in primary care to prevent hospitalisations and improve effectiveness and efficiency of care for people living with coronary heart disease (QUEL): protocol for a 24-month cluster randomised controlled trial in primary care. BMC Family Practice 21, 36.
| Crossref | Google Scholar | PubMed |
Reed JE, Card AJ (2016) The problem with Plan-Do-Study-Act cycles. BMJ Quality & Safety 25, 147-152.
| Crossref | Google Scholar | PubMed |
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Oliveira GMd, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V (2020) Global burden of cardiovascular diseases and risk factors, 1990–2019: update From the GBD 2019 study. Journal of the American College of Cardiology 76, 2982-3021.
| Crossref | Google Scholar | PubMed |
Speroff T, James BC, Nelson EC, Headrick LA, Brommels M (2004) Guidelines for appraisal and publication of PDSA quality improvement. Quality Management in Health Care 13, 33-39.
| Crossref | Google Scholar | PubMed |
Swerissen H, Duckett S, Moran G (2018) Mapping primary care in Australia. Grattan Institute, Australia. Available at https://grattan.edu.au/wp-content/uploads/2018/07/906-Mapping-primary-care.pdf [Accessed 14 September 2023]
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE (2014) Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Quality & Safety 23, 290-298.
| Crossref | Google Scholar |
The Royal Australian College of General Practitioners (2010) QA&CPD Category 1 activity: Rapid PDSA cycles – improving practice processes for the care of patients with diabetes. The Royal Australian College of General Practitioners, East Melbourne, Victoria, Australia. Available at https://www.racgp.org.au/download/documents/guidelines/diabetes/cat1_rapidpdsacycles.pdf [Accessed 6 September 2023]
The Royal Australian College of General Practitioners (2016) QI&CPD Program: 2017–19 triennium handbook for general practitioners. RACGP, East Melbourne, Victoria, Australia. Available at https://www.racgp.org.au/FSDEDEV/media/documents/Education/Professional%20development/QI-CPD/QICPD-Handbook-2017-19-triennium.pdf [Accessed 6 September 2023]
The Royal Australian College of General Practitioners (2018) General Practice: Health of the Nation 2018. RACGP, East Melbourne, Victoria, Australia. Available at https://www.racgp.org.au/download/Documents/Publications/Health-of-the-Nation-2018-Report.pdf [Accessed 6 September 2023]
The Royal Australian College of General Practitioners (2020) Continuing Professional Development (CPD) Program: Handbook for general practitioners. RACGP, East Melbourne, Victoria, Australia. Available at https://www.racgp.org.au/FSDEDEV/media/documents/Education/Professional%20development/QI-CPD/GP-Handbook-2020-22-triennium.pdf [Accessed 6 September 2023]
The Royal Australian College of General Practitioners (2022) General Practice: Health of the Nation 2022. RACGP, East Melbourne, Victoria, Australia. Available at https://www.racgp.org.au/getmedia/80c8bdc9-8886-4055-8a8d-ea793b088e5a/Health-of-the-Nation.pdf.aspx [Accessed 4 September 2023]
The Royal Australian College of General Practitioners (2023) Activities for your Continuing Professional Development (CPD) in 2023. RACGP, East Melbourne, Victoria, Australia. Available at https://cesphn.org.au/wp-content/uploads/All_Categories/CPD/PDFs/Activities-for-your-CPD.pdf [Accessed 6 September 2023]
van Assen MF (2021) Training, employee involvement and continuous improvement – the moderating effect of a common improvement method. Production Planning & Control 32, 132-144.
| Crossref | Google Scholar |
Wolfson D, Bernabeo E, Leas B, Sofaer S, Pawlson G, Pillittere D (2009) Quality improvement in small office settings: an examination of successful practices. BMC Family Practice 10, 14.
| Crossref | Google Scholar | PubMed |
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, Brauer M, Kutty VR, Gupta R, Wielgosz A, AlHabib KF, Dans A, Lopez-Jaramillo P, Avezum A, Lanas F, Oguz A, Kruger IM, Diaz R, Yusoff K, Mony P, Chifamba J, Yeates K, Kelishadi R, Yusufali A, Khatib R, Rahman O, Zatonska K, Iqbal R, Wei L, Bo H, Rosengren A, Kaur M, Mohan V, Lear SA, Teo KK, Leong D, O’Donnell M, McKee M, Dagenais G (2020) Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 395, 795-808.
| Crossref | Google Scholar | PubMed |